* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Infection Control for Obstetrics and Gynecology: Ware
Tuberculosis wikipedia , lookup
Hookworm infection wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Herpes simplex wikipedia , lookup
Sarcocystis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Gastroenteritis wikipedia , lookup
Trichinosis wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Schistosomiasis wikipedia , lookup
Marburg virus disease wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Methicillin-resistant Staphylococcus aureus wikipedia , lookup
Hepatitis C wikipedia , lookup
Hepatitis B wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Lymphocytic choriomeningitis wikipedia , lookup
Anaerobic infection wikipedia , lookup
Candidiasis wikipedia , lookup
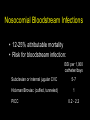
Infection Control for the OB/GYN Surgeon Gonzalo Bearman, MD, MPH Assistant Professor of Internal Medicine & Epidemiology Associate Hospital Epidemiologist Outline • Nosocomial Infections are a significant cause of morbidity and mortality • There has been increased public interest in nosocomial infections • Shifting paradigm – Many infections are preventable • SSI and OB/GYN – Surveillance data – Risk factors – Modifiable risk factors- modifiable interventions • BSI and OB/GYN – Surveillane – Risk reduction strategies • Proliferation of drug resistant nosocomial pathogens – Hand Hygeiene and Contact precautions “11,600 patients got infections in Pa. hospitals “ 7/13/2005 "The consequences clearly are huge," says Marc Volavka, executive director of the Pennsylvania Health Care Cost Containment Council, an independent state agency that published the data. "Everyone is paying the bill." Hospital-acquired infections reported by Pennsylvania hospitals in 2004: Infection Number Urinary tract 6,139 Bloodstream 1,932 Pneumonia 1,335 Surgical site 1,317 Multiple infections 945 Total 11,668 Source: Pennsylvania Health Care Cost Containment Council U.S. News and World Report, July 18, 2005. Shifting Vantage Points on Nosocomial Infections Many infections are inevitable, although some can be prevented Each infection is potentially preventable unless proven otherwise Gerberding JL. Ann Intern Med 2002;137:665-670. Nosocomial Infections • 5-10% of patients admitted to acute care hospitals acquire infections – 2 million patients/year – ¼ of nosocomial infections occur in ICUs – 90,000 deaths/year – Attributable annual cost: $4.5 – $5.7 billion • Cost is largely borne by the healthcare facility not 3rd party payors Weinstein RA. Emerg Infect Dis 1998;4:416-420. Jarvis WR. Emerg Infect Dis 2001;7:170-173. Nosocomial Infections • 70% are due to antibiotic-resistant organisms • Invasive devices are more important than underlying diseases in determining susceptibility to nosocomial infection Burke JP. New Engl J Med 2003;348:651-656. Safdar N et al. Current Infect Dis Reports 2001;3:487-495. Attributable Costs of Nosocomial Infections Cost per Infection Wound infections Sternal wound infection Catheter-associated BSI Pneumonia Urinary tract infection $3,000 - $27,000 $20,000 - $80,000 $5,000 - $34,000 $10,000 - $29,000 $700 Nettleman M. In: Wenzel RP, ed. Prevention and Control of Nosocomial Infections, 4th ed. 2003:36. Major Sites of Nosocomial Infections • • • • Urinary tract infection Bloodstream infection Pneumonia (ventilator-associated) Surgical site infection Surgical Site Infections in Obstetrics and Gynecology National Nosocomial Infections Surveillance System (NNIS) • NNIS is the only national system for tracking HAIs • Voluntary reporting system has approximately 300 hospitals • The NNIS database uses standardized definitions of HAI’s to: – Describe the epidemiology of HAIs – Describe antimicrobial resistance associated with HAIs – Produce aggregated HAI rates suitable for interhospital comparison http://www.cdc.gov/ncidod/hip/SURVEILL/NNIS.HTM National Nosocomial Infections Surveillance System (NNIS) Classification Clean Clean-contaminated: GI/GU tracts entered in a controlled manner Wound Class 0 SSI Risk Lower 1 Contaminated: open, fresh, traumatic wounds infected urine, bile gross spillage from GI tract Dirty-infected: 2 3 Higher NNIS- SSI Surveillance 1992-2004 Abdominal Hysterectomy Risk Index Number of hospitals Pooled mean rate Median- 50% percentile Per 100 operations 0 107 1.36 0.91 1 100 2.32 1.96 2,3 53 5.17 4.21 Am J Infect Control 2004;32:470-85 NNIS- SSI Surveillance 1992-2004 Vaginal Hysterectomy Risk Index Number of hospitals Pooled mean rate Per 100 operations 0,1,2,3 71 1.31 Am J Infect Control 2004;32:470-85 Median50% percentile 0.91 NNIS- SSI Surveillance 1992-2004 Cesarean Section Risk Index Number of Pooled hospitals mean rate Per 100 operations Median50% percentile 0 130 2.71 2.17 1 117 4.14 3.19 2,3 51 7.53 5.38 Am J Infect Control 2004;32:470-85 Hospital Morbidity Due to Post-operative Infections in Obstetrics and Gynecology • Post operative infections prospectively surveyed from 1997-1998 in tertiary care medical center, Bahrain – Definition of postoperative infection: • Fever • Purulent discharge from wound – With or without a positive microbiologic culture • Re-admissions for wound infections were not included in the study Saudi Medical Journal 2000: Vol 21 (3) 270-273 Hospital Morbidity Due to Post-operative Infections in Obstetrics and Gynecology Type of operation (%) No. of Operations (%) Wound Infection alone (%) Fever alone (%) Both wound Infection and Fever (%) Cesarean section 2193 35 (2) 30 (1) 7 (0.3) Major Gynecologic Surgery 1839 9 (0.4) 5 (0.3) 4 (0.2) Total 4032 35 (0.9) 35 (0.9) 11(0.3) Saudi Medical Journal 2000: Vol 21 (3) 270-273 Hospital Morbidity Due to Post-operative Infections in Obstetrics and Gynecology Organism Number of Isolates Gram Positive •S.aureus •S.epidermidis •Streptococci •Enterococci 3 (3) 13 (14) 6(6) 19 (20) Gram Negative •Enterbacter •Klebsiella •E.coli •Proteus •P.aeruginosa •Acinetobacter •Gram negative bacilli 4(4) 14(15) 11(12) 9(10) 8(8.5) 1(1) 1(1) Candida 5(5) Total 94 Saudi Medical Journal 2000: Vol 21 (3) 270-273 Genitourinary flora is a significant source of contamination during surgery Risk Factors for Surgical Site Infections Following Cesarean Section • OBJECTIVE: To identify risk factors associated with surgical-site infections (SSIs) following cesarean sections. • DESIGN: Prospective cohort study. • SETTING: High-risk obstetrics and neonatal tertiary-care center in upstate New York. • METHODS: • Prospective surgical-site surveillance was conducted using methodology of the National Nosocomial Infections Surveillance System. • Infections were identified on admission, within 30 days following the cesarean section, by readmission to the hospital or by a postdischarge survey. • Multiple logistic-regression analysis used for risk factor identification Infect Control Hosp Epidemiol. 2001 Oct;22(10):613-7 Risk Factors for Surgical Site Infections Following Cesarean Section Multiple logistic-regression analysis Risk Factor Odds Ratio/ 95% CI/ P value Absence of antibiotic prophylaxis 2.63; 1.50-4.6; P=.008 Length surgery 1.01; 1.00-1.02; P=.04 <7 prenatal visits 3.99; 1.74-9.15; P=.001 Duration of ruptured membranes 1.02; 1.01-1.03; P=.04 Infect Control Hosp Epidemiol. 2001 Oct;22(10):613-7 Summary: SSI’s in OB/GYN • NNIS- SSIs are reported to occur in 1%7% of OB/GYN surgeries • SSI are typically caused by maternal cutaneous or endometrial/vaginal flora • When an exogenous source is the cause of SSI in the obstetrical patient, S.aureus is frequently implicated Preventing Surgical Site Infections Focus on modifiable risk factors Sources of SSIs • Endogenous: patient’s skin or mucosal flora – Increased risk with devitalized tissue, fluid collection, edema, larger inocula • Exogenous – Includes OR environment/instruments, OR air, personnel • Hematogenous/lymphatic: seeding of surgical site from a distant focus of infection – May occur days to weeks following the procedure • Most infections occur due to organisms implanted during the procedure Up to 20% of skin-associated bacteria in skin appendages (hair follicles, sebaceous glands) & are not eliminated by topical antisepsis. Transection of these skin structures by surgical incision may carry the patient's resident bacteria deep into the wound and set the stage for subsequent infection. Downloaded from: Principles and Practice of Infectious Diseases © 2004 Elsevier Risk Factors for SSI • Duration of pre-op hospitalization * increase in endogenous reservoir • Pre-op hair removal * esp if time before surgery > 12 hours * shaving>>clipping>depilatories • Duration of operation *increased bacterial contamination * tissue damage * suppression of host defenses * personnel fatigue SCIP • A national partnership of organizations to improve the safety of surgical care by reducing post-operative complications through a national campaign • Goal: reduce the incidence of surgical complications by 25 percent by the year 2010 • Initiated in 2003 by the Centers for Medicare & Medicaid Services (CMS) & the Centers for Disease Control & Prevention (CDC) – Steering committee of 10 national organizations – More than 20 additional organizations provide technical expertise Putting risk reduction guidelines into practice SCIP Steering Committee Organizations • • • • • • • • • • Agency for Healthcare Research and Quality American College of Surgeons American Hospital Association American Society of Anesthesiologists Association of periOperative Registered Nurses Centers for Disease Control and Prevention Centers for Medicare & Medicaid Services Department of Veterans Affairs Institute for Healthcare Improvement Joint Commission on Accreditation of Healthcare Organizations SCIP Performance Measures Surgical infection prevention • SSI rates • Appropriate prophylactic antibiotic chosen • Antibiotic given within 1 hour before incision • Discontinuation of antibiotic within 24 hours of surgery • Glucose control • Proper hair removal • Normothermia in colorectal surgery patients Monetary incentives for promoting quality and compliance with SSI risk reduction guidelines: March 12, 2005 In recent years, the healthcare industry has placed a stronger emphasis on reducing medical errors, monitoring everything from how long doctors sleep to whether or not their handwriting is legible. Now one organization is not only recognizing the hospitals that follow patient safety and clinical guidelines, but rewarding them for doing so. Anthem Blue Cross and Blue Shield recently gave a total of $6 million to 16 Virginia hospitals as part of the company's new Quality-In-Sights Hospital Incentive Program (Q-HIP). http://www.richmond.comID=15 Infection Rate Downloaded from: Principles and Practice of Infectious Diseases Process Indicators: Appropriate Antibiotic Prophylaxis Procedure Approved Antibiotics •Cefazolin Hysterectomy •Cefoxitin Approved for β-lactam allergy •Clindamycin + gentamicin •Clindamycin + levofloxacin •Metronidazole + gentamicin •Metronidazole + levofloxacin •Clindamycin Process Indicators: Duration of Antimicrobial Prophylaxis Prophylactic antimicrobials should be discontinued within 24 hrs after the end of surgery Bratzler DW et al. Clin Infect Dis 2004;38:1706-15. Process Indicators: Timing of First Antibiotic Dose Infusion should begin within 60 minutes of the incision Bratzler DW et al. Clin Infect Dis 2004;38:1706-15. Nosocomial Bloodstream Infections Nosocomial Bloodstream Infections, 1995-2002 Rank N= 24,847 52 BSI/10,000 admissions Pathogen Percent 1 Coagulase-negative Staph 31.3% 2 S. aureus 20.2% 3 Enterococci 9.4% 4 Candida spp 9.0% 5 E. coli 5.6% 6 Klebsiella spp 4.8% 7 Pseudomonas aeruginosa 4.3% 8 Enterobacter spp 3.9% 9 Serratia spp 1.7% 10 Acinetobacter spp 1.3% Edmond M. SCOPE Project. Nosocomial Bloodstream Infections, 1995-2002 Obstetrics and Gynecology •Proportion of all BSI 0.9% (n=209) •E.coli (33%) •S.aureus (11.7%) •Enterococci (11.7) N= 24,847 52 BSI/10,000 admissions In obstetrics, BSIs are uncommon. However, the principal pathogen is E.coli and not coagulase negative staphylococci. The source is typically genitourinary Edmond M. SCOPE Project. Nosocomial Bloodstream Infections • 12-25% attributable mortality • Risk for bloodstream infection: BSI per 1,000 catheter/days Subclavian or internal jugular CVC 5-7 Hickman/Broviac (cuffed, tunneled) 1 PICC 0.2 - 2.2 Risk Factors for Nosocomial BSIs • Heavy skin colonization at the insertion site • Internal jugular or femoral vein sites • Duration of placement • Contamination of the catheter hub Prevention of Nosocomial BSIs • Coated catheters – In meta-analysis C/SS catheter decreases BSI (OR 0.56, CI95 0.37-0.84) – M/R catheter may be more effective than C/SS – Disadvantages: potential for development of resistance; cost (M/R > C/SS > uncoated) • Use of heparin – Flushes or SC injections decreases catheter thrombosis, catheter colonization & may decrease BSI Prevention of Nosocomial BSIs • Limit duration of use of intravascular catheters – No advantage to changing catheters routinely • Change CVCs to PICCs when possible • Maximal barrier precautions for insertion – Sterile gloves, gown, mask, cap, full-size drape – Moderately strong supporting evidence • Chlorhexidine prep for catheter insertion 30%-40% of all Nosocomial Infections are Attributed to Cross TransmissionImplication For The Spread Drug Resistant Pathogens NNIS: Selected antimicrobial resistant pathogens associated with HAIs Fig 1. Selected antimicrobial-resistant pathogens associated with nosocomial infections in ICU patients, comparison of resistance rates from January through December 2003 with 1998 through 2002, NNIS System. Am J Infect Control 2004;32:470-85 Antimicrobial Resistant Pathogens of Ongoing Concern • Vancomycin resistant enterocci – 12% increase in 2003 when compared to 1998-2002 • MRSA – 12% increase in 2003 when compared to 1998-2002 – Increased reports of Community-Acquired MRSA • Cephalosporin and Imipenem resistant gram negative rods – Klebsiella pneumonia – Pseudomonas aeruginosa Am J Infect Control 2004;32:470-85 Transfer of VRE via HCW Hands 16 transfers (10.6%) occurred in 151 opportunities. •13 transfers occurred in rooms of unconscious patients who were unable to spontaneously touch their immediate environment Duckro et al. Archive of Int Med. Vol.165,2005 The inanimate environment is a reservoir of pathogens X represents a positive Enterococcus culture The pathogens are ubiquitous ~ Contaminated surfaces increase cross-transmission ~ Abstract: The Risk of Hand and Glove Contamination after Contact with a VRE (+) Patient Environment. Hayden M, ICAAC, 2001, Chicago, IL. Community-associated methicillinresistant Staphylococcus aureus in hospital nursery and maternity units. • Outbreak of 7 cases of skin and soft tissue infections due to a strain of CA-MRSA. – All patients were admitted to the labor and delivery, nursery, or maternity units during a 3-week period. – Genetic fingerprinting showed that the outbreak strain was closely related to the USA 400 strain that includes the midwestern strain MW2 Emerg Infect Dis. 2005 Jun;11(6):808-13. Table 1. Clinical information for patients with methicillin-resistant Staphylococcus aureus infection during the outbreak period Age at onset Sex Strain Infection type Initial therapy Definitive therapy P1, newborn 8d F USA 400 Preseptal cellulitis Nafcillin, cefotaxime Topical gentamicin P2, newborn 13 d F USA 400 Omphalitis, otitis externa Ampicillin, cefotaxime Topical mupirocin P3, mother 33 y F USA 400 Breast abscess Cefazolin Surgical drainage, vancomycin, topical mupirocin P4, newborn 2d M USA 400 Omphalitis, pustulosis Nafcillin Gentamicin Gentamicin, topical mupirocin P5, newborn 4d M USA 400 Pustulosis Cephalexin Topical bacitracin P6, newborn 2d M USA 400 Pustulosis None Local wound care P7, newborn 1d F USA 400 Pustulosis, mastitis Topical mupirocin Vancomycin P8, mother 24 y F Unique Peripheral IV catheter site Cefazolin Trimethoprim-sulfamethoxazole, catheter removal Patient Emerg Infect Dis. 2005 Jun;11(6):808-13. Epidemic of Staphylococcus aureus nosocomial infections resistant to methicillin in a maternity ward • Seventeen cases were recorded over a nineweek period (two cases per week). – All were skin and soft tissue infections • Pulsed field gradient gel electrophoresis confirmed the clonal character of the strain. • No definite risk factors were determined by a case-control study. • Environmental factors were considered key in the persistence of this MRSA outbreak. Pathol Biol (Paris). 2001 Feb;49(1):16-22. The inanimate environment is a reservoir of pathogens Recovery of MRSA, VRE, C.diff CNS and GNR Devine et al. Journal of Hospital Infection. 2001;43;72-75 Lemmen et al Journal of Hospital Infection. 2004; 56:191-197 Trick et al. Arch Phy Med Rehabil Vol 83, July 2002 Walther et al. Biol Review, 2004:849-869 The inanimate environment is a reservoir of pathogens Recovery of MRSA, VRE, CNS. C.diff and GNR Devine et al. Journal of Hospital Infection. 2001;43;72-75 Lemmen et al Journal of Hospital Infection. 2004; 56:191-197 Trick et al. Arch Phy Med Rehabil Vol 83, July 2002 Walther et al. Biol Review, 2004:849-869 The inanimate environment is a reservoir of pathogens Recovery of MRSA, VRE, CNS. C.diff and GNR Devine et al. Journal of Hospital Infection. 2001;43;72-75 Lemmen et al Journal of Hospital Infection. 2004; 56:191-197 Trick et al. Arch Phy Med Rehabil Vol 83, July 2002 Walther et al. Biol Review, 2004:849-869 Alcohol based hand hygiene Easy to use Quick solutions Very effective antisepsis due to bactericidal properties of alcohol Hand Hygiene • Single most important method to limit cross transmission of nosocomial pathogens • Multiple opportunities exist for HCW hand contamination – Direct patient care – Inanimate environment • Alcohol based hand sanitizers are ubiquitous – USE THEM BEFORE AND AFTER PATIENT CARE ACTIVITIES Contact Precautions for drug resistant pathogens. Gowns and gloves must be worn upon entry into the patient’s room Conclusion • Nosocomial Infections are a significant causes of morbidity and mortality • There has been increased public interest in nosocomial infections- this will likely result in greater compliance with IC guidelines • Shifting paradigm – Many infections are preventable • SSI and OB/GYN – 1-7 % of all OB/GYN procedures (NNIS) – Increased scrutiny of compliance with risk reduction intervention – Preoperative antibiotics: choice, timing, discontinuation; • BSI and OB/GYN – BSI is less common than in Medicine/Surgical services – Risk reduction strategies should include appropriate use and prompt removal of invasive devices • Proliferation of drug resistant nosocomial pathogens – Importance of Hand Hygiene and Contact precautions