* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Immune prophylaxis of infectious diseases in children
Gastroenteritis wikipedia , lookup
Rotaviral gastroenteritis wikipedia , lookup
Neonatal infection wikipedia , lookup
Brucellosis wikipedia , lookup
Hepatitis C wikipedia , lookup
Orthohantavirus wikipedia , lookup
Typhoid fever wikipedia , lookup
Poliomyelitis eradication wikipedia , lookup
Poliomyelitis wikipedia , lookup
Cysticercosis wikipedia , lookup
Hepatitis B wikipedia , lookup
Antiviral drug wikipedia , lookup
Meningococcal disease wikipedia , lookup
Anthrax vaccine adsorbed wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Active immunization of
children, its importance for the
infectious diseases prophylaxis.
Vaccination schedule.
Postvaccinal complications.
Lecturer:
Gorishna Ivanna Lubomyrivna
Plan of the lecture
Short history about immunization
Recommended immunization schedule for
infants and children
Vaccinal reactions
Postvaccinal complications
Contraindications to the vaccination
The immune system
is a complex system of interacting cells whose
primary purpose is to identify foreign (“non-self”)
substances referred to as antigens.
The immune system develops a defense against the
antigen.
This defense is known as the immune response and
usually involves the production of protein molecules,
called antibodies (or immunoglobulins), and of
specific cells (also known as cell-mediated immunity)
whose purpose is to facilitate the elimination of
foreign substances.
The task of immuneprophylaxis
management of immunological answer to
prevent the disease between separate
persons and groups of the population.
There are two basic mechanisms
for acquiring this protection
active and passive.
Active immunity
Active immunity are defenses developed by the
body that last many years or even a life time.
1. Active-natural immunity – means invasion of the body by
microorganisms resulting in development of antibodies and
sensitized lymphocytes. Examples: childhood diseases chicken pox, measles.
2. Active-artificial immunity is attained by inoculation or
immunization with antigen of live or killed vaccines that are
less virulent than contacting the disease.
Passive immunity
is temporary, trasmitted from another source that
has developed immunity through previous
disease or immunization.
Passive-natural immunity is trasplacental and
colostrum transfer from mother to child of antibodies.
Immunity does not last.
Passive-artificial immunity is injections with
Gamma Globulin.
Classification of vaccine
Vaccines, which include complete killed microorganisms
(pertussis, typhoid, cholera) or inactivated viruses (influenza,
poliomyelitis Salk vaccine)
Anatoxins, which contains inactivated toxin of the bacteria
(diphtheria, tetanus)
The vaccines from alive attenuated viruses (measles, mumps
and others.)
Vaccines, which contains crossing alive microorganisms
(BCG)
Chemical vaccines from fraction of killed microorganisms
(pneumococcal, meningococcal)
Gene-engineering recombinant, chemical synthesized
(hepatitis В, influenza)
Associated (in composition of which enters several vaccines)
Composition of vaccines
Active or immunizing antigens
Fluid base
Preservatives, stabilizers, antibiotics
Auxiliary facilities
Provide active life long immunity against
disease
1. Recommended immunization Schedule for Healthy
Infants and Children
The recommended childhood vaccination
schedule (Ukraine)
Birth
Hepatitis B
3-7 days
BCG
1 month
Hepatitis B
3 month
IPV, DTaP, Hib
4 month
IPV, DTaP, Hib
5 month
OPV, DTaP, Hib
6 month
Hepatitis B
12
MMR
18 month
OPV, DTaP
6 years
DT-M, OPV, MMR
7 years
BCG
14 years
Tetanus-diphtheria booster, OPV
15 years
Rubella, Mumps
18 years
Tetanus-diphtheria booster
Ways of the vaccination
1. Intramuscular (DTP, DT, DT-M, antirhabic,
meningococcal B)
2. Subcutaneous (measles, mumps, rubella,
meningococcal A+C)
3. Intracutaneous (BCG)
4. On skin (plague, tularemia, brucellosis)
5. Peroral (poliomyelitis)
6. Intranasal (Influenza, inactivated)
Vaccination for tuberculosis prevention could not be
done in the same day with other vaccines or other
parenteral manipulations
Vaccines are injected to all
newborns, which has no
contraindications.
Immunization is done by
a vaccine to prevent
tuberculosis (BCG). For
vaccination of premature
infants weighing ≥ 2000 g
should be used TB
vaccine with reduced
antigen content (BCG-M).
Mantoux test
Mantoux test
before
vaccination
against TB
should be
done for
babies elder
than 2
months. A
negative test
result allows
making
vaccination
Immunization by monovalent hepatitis B
vaccine
If mother of a newborn is HBsAg "-" (negative),
the child may begin vaccination during the first
months of life, or combined with vaccination
against pertussis, diphtheria, tetanus, polio. The
recommended scheme is: 3-4-5-18 months, or: 3-49 mo.
Newborns weighing <2000 g born by HBsAg
negative mothers, vaccination is done when the
child’s weight will be 2000 g or at the age of 1 mo.
If the newborn child is in critical condition, the
child immunization should be done when he will
be better before hospital discharge.
Vaccination against viral hepatitis B of newborns,
whose mothers are carriers of HBsAg, is necessary
to do by the accelerated scheme: 0-1-2 and 12 mo.
Vaccinations for the prevention of
diphtheria, tetanus and pertussis
in the age 3, 4 and 5 months by diphtheria-tetanus-pertussis
vaccine (DTP), or vaccine with acellular pertussis component
(DTaP)
The interval between the first and second, second and third
vaccination is 30 days, the interval between the third and
fourth vaccination should be not less than 12 months.
The first booster at 18 months is done by DTaP.
The second and third booster at 6, 14 years is done by DT.
The first adult booster vaccination should be made by DT-M
at interval of 5 years after the last vaccination. Further booster
vaccinations for adults by DT-M with a minimum 10 years
interval from the previous vaccination.
For the prevention of diphtheria, tetanus, pertussis,
polio, hepatitis B and infections caused by bacteria
Haemophilus influenza type b (Hib), you can use the
combined vaccine
Inactivated vaccine to prevent polio (IPV) is
used for the first two immunizations
oral polio vaccine
(OPV) is used for 3
- 6th vaccination
(third vaccination
and age
revaccination) with
no contraindications
to OPV.
After the OPV is
proposed to restrict
injections, parenteral
intervention, routine
operations for 40
days, exclude contact
with HIV-infected
Vaccination to prevent Hib-infection
can be done by mono- and combined vaccines
containing Hib- components.
It is advisable to use combined Hib-vaccines for
primary vaccination.
Vaccination to prevent measles,
mumps and rubella
by the combined vaccine (hereafter - MMR) at the age of 12
months.
The second vaccine to prevent measles, mumps and rubella
- in 6 years.
Kids who were not vaccinated vaccination can begin at any
age before 18 years (2 doses with the minimum spacing
between them).
Children age 15 who received 1 or 2 vaccinations against
measles, but not vaccinated against rubella and mumps
and didn’t ill with these infections, vaccinations against
mumps (guys) or rubella (girls) is scheduled.
18-teens or older who have not previously been vaccinated
can be vaccinated with one dose before 30 years.
Recommended vaccinations
Varicella zoster
Hepatitis A
Hepatitis B
Flu
Pneumococcal infection
Passive immunization is indicated
To children with insufficient antibodies syntheses as a
result of congenital or acquired cellular defects of Вlymphocytes.
At absence of vaccines against infection, when single way
of protection is introduction of ready antibodies.
If required immediate preventive maintenance of the
disease for epidemiological causes (the contact with sick on
measles, preventive maintenance of rabies, tetanus).
For neutralization of the antigen-toxin by specific antitoxic
antibodies.
With medical purpose at the beginning of the diseases (at
diphtheria, botulism, tetanus).
Vaсcinal process
is a change of homeostasis, which appears in
organism in response to introduction of vaccinal
preparation and include the complex of reactions
to which belongs: formation of antibodies,
adaptation and postvaccinal reactions,
postvaccinal complications.
Vaccinal reactions
appear in response to entering the vaccines,
are characterized by appearance of clinical
manifestations typical to this type of
vaccine, which have a round-robin duration,
are short, do not cause serious changes of
vital activity in the organism.
Vaccinal reactions
Increased temperature to 39˚ C.
Increased temperature over 39˚ C (severe total reaction).
Temperature, which is not registered in medical
documentation.
Pain, soft tissue swelling > 50 mm, hyperemia in the
place of injection > 80 mm, infiltration > 20 mm (severe
local reaction).
Lymphadenopathy.
Headache.
Irritability, sleep disturbance.
Non allergic rash.
Anorexia, nausea, abdominal pain, indigestion and
diarrhea.
Catarrhal phenomena.
Myalgia, arthralgia.
Postvaccinal complications
- all pathological phenomena, which appear
after vaccination and are not inherent to the
usual vaccinal process, but obvious, their
relationship with performed vaccination:
1. Postvaccinal unusual reactions and
complications, caused strictly by vaccine
("true").
2. Joining of intercurrent infections in
postvaccinal period.
3. Exacerbation of chronic diseases and
primary manifestations of latent diseases.
Complication of vaccination
1. Anaphylactic shok
Angioneurotic edema
2. General rash, Stenen-Johnson
syndrome, Lyell’s syndrome,
3. Encephalitis, encephalopathy,
polyradiculoneuritis, mononeuritis
4. Febril seizures
unfebril seizures
5. Serous meningitis, myocarditis,
anemia, hemorrhagic vasculitis,
trombocytopenia
6. Sudden death syndrome
First 24 hr.
First 10 days
First 15 days
First 15 days
30 days
30 days
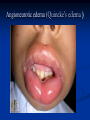
Angioneurotic edema (Quincke’s edema )
urticaria
(hives)
StevensJohnson’s
syndrome
Lyell’s syndrome
DTP-vaccine
Postvaccinal reactions
Postvaccinal complications
Temperature 37.5-39 ºС,
anxiety, poor sleeping, rarely vomiting.
Local reaction (more often on
revaccination) - in the
manner of hyperemia,
infiltration.
Febrile seizures
seizures
Encephalitis
Anaphylactic shok
Angioneurotic edema
febril temperature with seizures
persistent, uncontrolled crying that
lasts for more than 3 hours at a time
within 2 days after injection
Exacerbation allergic
manifestations (in children
with exudative-catarrhal
diathesis)
OPV-vaccine
Postvaccinal reactions
Postvaccinal complications
No
Anaphylactic shok
Angioneurotic edema
Vaccinassocated poliomyelitis in
immunized and in contact persons
(on background of
immunodeficiency) - 1:1,500000.
MMR vaccine
Postvaccinal reactions
Postvaccinal complications
Fever of 39.4°C
Rash develops at 7-10 days
after vaccination.
Arthralgia
Increasing of paroid glands
Serous meningitis
Angioneurotic edema
febril temperature
Seizures
Hemorrhagic vasculitis
Mild lymphadenopathy
Arthritis
thrombocytopenia
BCG-Vaccination
Postvaccinal reactions
Postvaccinal complications
Local reaction:
papule, vesicle,
lymphadenitis
1.
2.
3.
4.
5.
6.
Subcutaneous cool abscess
Purulent lymphadenitis.
Keloid scars.
Lymph nodes calcification.
Generalized BCG-infection
on background of immune
deficiency (4: 1000000).
6. Osteitis, osteomyelitis
Main rules of vaccination
Take allergic history
Take life history
Take history of vaccination
Take family history
Do objective exanimation of the child
Take temperature of the body
Do vaccination at special room
Follow the instruction of vaccine
Supervise the vaccinated person for 30 days
CONTRAINDICATIONS TO THE
VACCINATION by all vaccines and toxoids
Severe complications from the previous dose
in the form of anaphylactic shock.
Allergy to any vaccine component.
Progressive diseases of the nervous system,
hydrocephalus in decompensation stage,
epilepsy, epileptic syndrome with
convulsions 2 times a month and more often.
Acute illness or chronic disease exacerbation
CONTRAINDICATIONS TO THE
VACCINATION by all live vaccines
Congenital combined immune deficiency,
primary hypogammaglobulinemia (entering
the vaccine is not contraindicated in
selective Ig A and Ig M immunodeficiency),
transitional hypogammaglobulinemia
malignant tumors,
pregnancy,
AIDS,
immune suppression therapy
CONTRAINDICATIONS TO THE BCG-VACCINATION
baby weight less than 2000 g:
1500 - 1999 g vaccinations are not done up to
1 month.
1000 - 1499 g - up to 2 months.
Complicated reactions to previous vaccine
(adenitis, cold abscess, skin ulcers over 10
mm in diameter, kelloid scar, osteomyelitis,
generalized BCG infection).
Tubinfection.
Defects of phagocytosis
CONTRAINDICATIONS TO THE
VACCINATION
OPV
Children whom live vaccine is contraindicated,
as well as to members of their families is
recommended vaccination by polio inactivated
vaccine (IPV)
DTP
A history of convulsions (instead DTP vaccine DTaP vaccine or DT toxoid is injected)
CONTRAINDICATIONS TO THE
VACCINATIONS
By living vaccine against measles, living
mumps vaccine, vaccine against rubella or
trivaccine (measles, mumps, rubella)
Allergic reactions on Aminoglucosides
Anaphylactic reactions on eggs protein