* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Viral Diarrhoea and Vomiting Prevention and Management Policy
Herpes simplex virus wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Hepatitis B wikipedia , lookup
Oesophagostomum wikipedia , lookup
Rotaviral gastroenteritis wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Marburg virus disease wikipedia , lookup
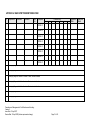
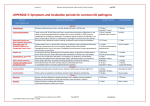
PREVENTION AND MANAGEMENT OF VIRAL DIARRHOEA AND VOMITING Version 2 Name of responsible (ratifying) committee Infection Prevention Management Committee Date ratified 17 March 2017 Document Manager (job title) Dr Caroline Mitchell - Head of Infection Prevention Date issued 11 April 2017 Review date 10 April 2020 Electronic location Infection Control Policies Related Procedural Documents Isolation Policy, Hand Hygiene Policy, Standard Precautions Policy Key Words (to aid with searching) Norovirus, Rotavirus, Adenovirus, Viral Gastroenteritis, Diarrhoea, Vomiting, Outbreak Version Tracking Version Date Ratified Brief Summary of Changes Author 2 17.03 2017 Minimal changes; removal of Difficil-S IPT 1 28.01.2015 Replaces Management of Outbreaks of Viral Diarrhoea and Vomiting IPT Prevention and Management of Viral Diarrhoea and Vomiting Version: 2 Issue Date: 11 April 2017 Review Date: 10 April 2020 (Unless requirements change) Page 1 of 16 CONTENTS 1. INTRODUCTION ......................................................................................................................... 4 2. PURPOSE ................................................................................................................................... 4 3. SCOPE ........................................................................................................................................ 4 4. DEFINITIONS .............................................................................................................................. 4 5. DUTIES AND RESPONSIBILITIES.............................................................................................. 5 6. PROCESS ................................................................................................................................... 5 7. TRAINING REQUIREMENTS ...................................................................................................... 8 8. REFERENCES AND ASSOCIATED DOCUMENTATION ............................................................ 9 9. EQUALITY IMPACT STATEMENT ............................................................................................ 10 10. MONITORING COMPLIANCE WITH PROCEDURAL DOCUMENTS ........................................ 11 APPENDIX A: WARD SYMPTOM MONITORING FORM ................................................................. 12 APPENDIX B: INFORMATION FOR STAFF ..................................................................................... 13 APPENDIX C: INFORMATION FOR STAFF .................................................................................... 14 EQUALITY IMPACT SCREENING TOOL ......................................................................................... 15 Prevention and Management of Viral Diarrhoea and Vomiting Version: 2 Issue Date: 11 April 2017 Review Date: 10 April 2020 (Unless requirements change) Page 2 of 16 QUICK REFERENCE GUIDE For quick reference the guide below is a summary of actions required. This does not negate the need for the document author and others involved in the process to be aware of and follow the detail of this policy. 1. Staff must critically assess all cases of diarrhoea and/or vomiting to determine the cause. This may include underlying conditions, recent anaesthetic, antibiotics, laxatives, feeding regimen etc. 2. If the onset of diarrhoea and/or vomiting is sudden and the symptoms are not clearly attributable to an underlying condition or therapy the patient must be isolated. Do not wait for further episodes of diarrhoea and/or vomiting before isolating. 3. Patients with suspected viral diarrhoea and/or vomiting should be isolated within two hours of onset of symptoms, preferably in a room with an en-suite toilet and washing facilities. If an en-suite is not available a commode should be provided for their sole use. It is not acceptable to leave a patient with suspected viral diarrhoea and/or vomiting in an open ward. Where no suitable single room is available in the immediate clinical area, staff should escalate to: i. Specialty flow coordinator (then) ii. Duty hospital manager (then) iii. (On-call) Infection Prevention Team 4. Any member of staff experiencing symptoms of diarrhoea and/or vomiting must stay away from work until two days after symptoms fully resolve. 5. A potential outbreak is classified as two or more cases of unexplained diarrhoea (type 6/7) and/or vomiting affecting patients or staff in a clinical area over a 48-hour period. Factors that may indicate an outbreak is occurring: Generally both staff and patients are affected Symptom are of rapid onset (particularly nausea) Vomiting (often projectile) can occur in more than 50% of cases There is an incubation period of 15- 48 hours. 6. Effective communication is essential at all times during a suspected or confirmed outbreak. If you require advice please contact: In hours: The Infection Prevention and Control Team (IPCT) on the Clinical Lead Bleep (0064) Out of Hours (inc. weekends): The IPCT via the main hospital switchboard. 7. The following immediate control measures must be implemented by clinical staff if an outbreak of viral gastroenteritis is suspected (full list of actions see section 7.5): Isolate symptomatic individuals immediately and keep all bay and side room doors closed Wear gloves and apron for contact with an affected patient or environment Wash hands with soap and water after contact with an affected patient / environment / PPE Do not use alcohol hand rub to decontaminate hands Remove all exposed food e.g. fruit from lockers etc. and de-clutter all areas Provide fresh drinking water and encourage regular sips of fluid for affected patients Use a chlorine-based agent (1000ppm Actichlor plus) to disinfect all surfaces and touch points e.g. door handles, bed rails, tables, chair handles at least twice daily Clean and disinfect vomit and faeces spillages promptly Use clear signage to alert staff and visitors that they are entering a restricted area (Appendix B) and emphasise hand hygiene before and after visiting patients Avoid transfer of patients and staff to unaffected wards or departments (unless medically urgent or for the specific purpose of isolation after consultation with IPCT) Prevention and Management of Viral Diarrhoea and Vomiting Version: 2 Issue Date: 11 April 2017 Review Date: 10 April 2020 (Unless requirements change) Page 3 of 16 1. INTRODUCTION The most common causes of infectious viral diarrhoea and/or vomiting are Noroviruses, followed by Adenoviruses and Rotaviruses. Norovirus accounts for at least 50% of all viral gastroenteritis outbreaks worldwide 1,2 and can be detected throughout the year. An estimated 600,000 to one million people contract Norovirus annually in the UK, mainly in their own homes. Approximately 3000 people a year are admitted to hospital with Norovirus in England. The Hospital Norovirus Outbreak Reporting System (HNORS) in England estimate that, on average, reported outbreaks are associated with 13,000 patients and 3,400 staff becoming ill, 8,900 days of ward closure and the loss of over 15500 bed-days, annually3 with a cost to the NHS in excess of £100 million per annum in years of high incidence.4,5 2. PURPOSE This Policy defines the actions taken by the Trust to ensure prompt recognition of viral diarrhoea and/or vomiting and to reduce the risk of transmission of infection by reducing the movement of the patient and contacts and preventing cross infection within the healthcare environment. 3. SCOPE This policy applies to all PHT Healthcare workers (HCW), including agency, bank and locum staff, Carillion staff including porters and house-keepers and visiting Health and Social Care Workers from other organisations. ‘In the event of an infection outbreak, flu pandemic or major incident, the Trust recognises that it may not be possible to adhere to all aspects of this document. In such circumstances, staff should take advice from their manager and all possible action must be taken to maintain ongoing patient and staff safety’ 4. DEFINITIONS Adenovirus: Types 40 and 41 cause gastroenteritis especially in children under the age of two. The virus is transmitted by the faecal-oral route with an incubation period of 3-10 days. The illness lasts approximately one week. Diarrhoea is more prominent than vomiting or fever, and respiratory symptoms are often present. Long-term immunity is acquired in childhood. Diarrhoea and vomiting: Diarrhoea refers to type 6/7 stool on the Bristol Stool Chart. Any case of diarrhoea or vomiting amongst patients or staff should be regarded as potentially infectious and treated as such unless an infectious cause can be confidently excluded. Norovirus: Norovirus has a small infective dose with an incubation period of 12 to 48 hours. Peak viral shedding occurs between two to five days. The virus is transmitted by the faecal-oral route or from contaminated surroundings. Occasionally food may be implicated in its transmission. Symptoms are typically rapid onset nausea and vomiting (often projectile), followed by watery diarrhoea. Symptoms persist for one to two days, and are generally mild but may be more serious in the extremes of age or when other pre-existing disease is present. In the elderly population, typical projectile vomiting frequently may not occur and the main symptoms are nausea and diarrhoea. In the elderly or immuno-compromised, symptoms may continue for four to seven days. Rotavirus: Is the most common cause of severe diarrhoea among infants and young children. Immunity develops with each infection, so subsequent infections are less severe; adults are rarely affected. The virus is transmitted by the faecal-oral route. Rotavirus gastroenteritis is characterised by vomiting, watery diarrhoea, and low-grade fever. The incubation period is around two days. Symptoms often start with vomiting followed by four to eight days of profuse diarrhoea. Prevention and Management of Viral Diarrhoea and Vomiting Version: 2 Issue Date: 11 April 2017 Review Date: 10 April 2020 (Unless requirements change) Page 4 of 16 Rotavirus vaccine is now routinely offered to infants. 5. DUTIES AND RESPONSIBILITIES All Trust employees, including agency, bank and locum staff, are responsible for performing appropriate infection control practice. Any member of staff experiencing symptoms of diarrhoea and/or vomiting must stay away from work until two days after symptoms fully resolve. Effective communication is essential at all times during a suspected or confirmed outbreak. If you require advice please contact: In hours: The Infection Prevention and Control Team (IPCT) on the Clinical Lead Bleep (0064) Out of Hours (inc. weekends): The IPCT via the main hospital switchboard. Clinicians: diarrhoea and/or vomiting can be feature of many serious illnesses. It is essential that clinicians assess each symptomatic patient for possible infectious causes and escalate suspected infectious cases to the nurse in charge for isolation. Clinicians are also responsible for managing patient’s hydration and underlying health conditions which may be affected by viral gastroenteritis A&E / MAU / Direct Admissions: patients referred to hospital with symptoms of diarrhoea and / or vomiting, particularly if there is a household history of other cases, should be admitted into an isolation room Patient Flow Managers: are responsible for facilitating rapid isolation of suspected or confirmed cases of viral gastroenteritis and for following the advice of the IPCT Wards: are responsible for assessing each case of diarrhoea and/or vomiting and making a risk assessment over possible infectious causes. Suspected cases should be isolated immediately and the IPCT informed if there are two or more cases amongst patients or staff. Ward staff are responsible for the prompt cleaning and disinfection of patient equipment and areas contaminated by vomit and faeces and the maintenance of hydration of affected patients. IPCT: are responsible for ensuring staff are appropriately educated and supported to prevent outbreaks, for managing suspected and confirmed outbreaks of viral gastroenteritis and for liaising with the trust management during an outbreak 6. PROCESS 6.1 ACTION TO BE TAKEN IN RESPONSE TO AN INDIVIDUAL CASE OF DIARRHOEA AND/OR VOMITING It is critical that staff assess all cases of diarrhoea and/or vomiting to determine the cause. Assess cause of diarrhoea and/or vomiting (including underlying conditions, recent anaesthetic, antibiotics, laxatives, feeding regimen etc) If onset is sudden and the diarrhoea and/or vomiting is not clearly attributable to an underlying condition or therapy the patient must be isolated Do not wait for further episodes of diarrhoea and/or vomiting before isolating Patients with suspected viral diarrhoea and/or vomiting should be isolated within two hours of onset of symptoms, preferably in a room with an en-suite toilet and washing facilities. If an ensuite is not available a commode should be provided for their sole use. It is not acceptable to leave a patient with suspected viral diarrhoea and/or vomiting in an open ward Where no suitable single room is available in the immediate clinical area, staff should escalate to: i. Specialty flow coordinator (then) ii. Duty hospital manager (then) Prevention and Management of Viral Diarrhoea and Vomiting Version: 2 Issue Date: 11 April 2017 Review Date: 10 April 2020 (Unless requirements change) Page 5 of 16 iii. (On-call) Infection Prevention Team Observe contacts for symptoms of viral gastroenteritis and isolate further cases as required Obtain an infectious clean of the vacated bed-space and implement touch point cleaning (door handles, bed rails, chair arms, taps etc. in the vacated area Accurately record all episodes of diarrhoea and/or vomiting on VitalPAC/Bristol Stool Chart. 6.2 ACTION TO BE TAKEN BY THE NURSE-IN-CHARGE IN A SUSPECTED OUTBREAK A potential outbreak is classified as two or more cases of unexplained diarrhoea (type 6/7) and/or vomiting affecting patients or staff in a clinical area over a 48-hour period Factors that may indicate an outbreak is occurring Generally both staff and patients are affected Symptom are of rapid onset (particularly nausea) Vomiting (often projectile) can occur in more than 50% of cases There is an incubation period of 15- 48 hours. Notify the IPCT (section 5) as soon as an outbreak is suspected Isolate in single cubicles with transmission precautions the first cases Accurately record all episodes of diarrhoea and/or vomiting on VitalPAC/Bristol Stool Chart. Collect specimens for microbiological testing Inform the Senior Nurse or bleep holder for unit/department Inform the Duty Hospital Manager on bleep 118 Information required by the IPCT will include the following that should be recorded on the Ward Symptom Monitoring Form (Appendix A): The number of patients and/or staff members affected. For each patient/member of staff, the date and time of onset and the symptoms. For each patient, any treatment e.g. antibiotics, laxatives, NG feeds etc. they are receiving, and any confirmed microbiology results e.g. Clostridium difficile. The dates any stool specimens have been taken and the results if known. A stool specimen should be obtained from affected patients and sent for both M C & S and virology. Members of staff who become symptomatic while on duty should inform their manager and contact the Occupational Health Service. They must leave the clinical area and Must Not return to work until they have been symptom free for 48 hours. Catering staff must seek advice regarding return to duty from the Occupational Health Service. 6.3 ACTION TO BE TAKEN BY THE IPCT IN A SUSPECTED OUTBREAK The IPCT will conduct an immediate clinical assessment of the patients affected and the ward area. Early, aggressive intervention is critical in breaking the chain of transmission and preventing uncontrolled onwards spread. Following assessment, the IPCT will determine the most appropriate course of action to protect patients and the operational functioning of the hospital. NOT AN OUTBREAK: Symptoms are clearly attributable to non-infectious causes – no further action and ward staff to monitor LOW POSSIBILITY OF AN OUTBREAK: Most symptoms clearly attributable to non-infectious causes. Immediate isolation of patient(s) with suspicious symptoms and implementation of enhanced cleaning and precautions, ward open to admissions, discharges and transfers Prevention and Management of Viral Diarrhoea and Vomiting Version: 2 Issue Date: 11 April 2017 Review Date: 10 April 2020 (Unless requirements change) Page 6 of 16 HIGH POSSIBILITY OF AN OUTBREAK: Most symptoms are suspicious of, or attributable infectious causes. Immediate isolation of patient(s) with suspicious symptoms and implementation of enhanced cleaning and precautions, transfers from the ward may be restricted. 6.4 ENHANCED OUTBREAK PRECAUTIONS AND WARD RESTRICTIONS It may become necessary to place a ward under enhanced outbreak precautions and restrict the movement of patients (transfers to other wards or care facilities) if the transmission rate (attack ratio) is such that the safety of patients and staff is affected. The decision to restrict the movement of patients must be made under the guidance of the IPCT. Restricted movement will generally involve: No general transfer of patients to other wards in the hospital (unless for the purpose of isolation or specific specialty treatment). This should not compromise the safety, efficacy or quality of the patient’s care No discharge of patients receiving a package of care or to other institutions/healthcare facilities (unless the patient has been in an unaffected area of the ward or the receiving facility can implement isolation and barrier precautions The IPCT will determine if it is appropriate to admit patients to a restricted area. Where patients can be safely discharged, this should be encouraged to reduce the potential reservoir of patients and create space on the ward. Patients may be discharged to their own homes, provided they are medically fit for discharge and have support. The IPCT will request enhanced cleaning measures from the Carillion Help Desk when appropriate. 6.5 CONTROL MEASURES TO BE PUT IN PLACE IF THE WARD IS UNDER ENHANCED OUTBREAK PRECAUTIONS AND WARD RESTRICTIONS Isolate symptomatic individuals immediately - only cohort under the guidance of the IPCT Keep all bay and side room doors closed (when safe to do so) Wear gloves and apron for contact with an affected patient or environment Wash hands with soap and water after contact with an affected patient or environment (after removing gloves and apron) Do not use alcohol hand rub to decontaminate hands Remove all exposed food e.g. fruit from lockers etc. and de-clutter all areas Provide fresh drinking water for all patients, dish washer jugs and cups and implement intentional rounding for affected patients to encourage regular sips of fluid Use a freshly prepared chlorine-based agent (e.g. 1000ppm Actichlor plus) to disinfect all surfaces and touch points e.g. door handles, bed rails, tables, chair handles at least twice daily Clean and disinfect vomit and faeces spillages promptly Consider use of antiemetics for patients with vomiting Use clear signage to alert staff and visitors that they are entering a restricted area (Appendix B) and emphasise hand hygiene before and after visiting patients Take time to inform patients and their visitors/ relatives of the nature and extent of the outbreak and the consequences for the patient Provide written information to staff, patients and relatives (Appendix C). Leaflets for patients and visitors can be obtained from medical photography (MPI 10/471) Exclude affected staff from the ward immediately and until 48 hours symptom-free Avoid transfer of patients and staff to unaffected wards or departments (unless medically urgent or for the specific purpose of isolation after consultation with IPCT) Exclude non-essential staff from affected clinical areas Prevention and Management of Viral Diarrhoea and Vomiting Version: 2 Issue Date: 11 April 2017 Review Date: 10 April 2020 (Unless requirements change) Page 7 of 16 Admissions to wards should be risk assessed by the IPCT to prevent the unnecessary introduction of further susceptible individuals Staff working on affected wards must not work in unaffected areas for 48 hours after the end of shift Vacuum cleaning carpets and buffing floors during an outbreak have the potential to recirculate Norovirus and are not recommended. Toys in paediatric wards should be capable of withstanding disinfection and this should be carried out on a daily basis Thoroughly clean the ward and change the bed curtains before lifting restrictions Restrictions should not be lifted until 72 hours after the last new case and 72 hours after uncontained vomiting and diarrhoea (as guided by the IPCT). 6.6 TESTING FOR NOROVIRUS It is important that initial management is based on symptoms in order to facilitate rapid isolation and control measures. Wards should not wait for the results of specimens to initiate control measures. Testing will be guided by the IPCT. Only unformed faecal specimens from symptomatic individuals within three days of onset of symptoms should be referred for Norovirus PCR testing. 6.7 COMMUNICATIONS Communications are always important in the control of suspected or confirmed outbreaks. Wards should inform the IPCT immediately whenever there are two or more cases of unexplained vomiting or diarrhoea among patients or staff Other areas in the hospital should be alerted early so that all staff are vigilant and can give notice of spread of infection to new areas. This alert should extend to services such as radiology, physiotherapy, phlebotomy and portering where staff and patient movements can potentially allow rapid spread of infection to all areas of the hospital. Managers and Patient Flow must be updated at least daily during an outbreak to allow appropriate operational and manpower planning. The Consultant in Communicable Disease Control (CCDC) should be informed where there is uncontrolled onwards tranmission despite adequate control measures The lead Clinical Commissioning Group (CCG) should be informed where the staffing of the hospital is compromised or the operational capacity of the hospital is affected All outbreaks should be reported to Public Health England (PHE) via the Hospital Norovirus Outbreak Reporting Tool 6.8 LIFTING OF WARD RESTRICTIONS The decision to lift enhanced outbreak precautions and ward restrictions can only be made in collaboration with a member of the IPCT. The attack rate and the recovery rate The decontamination of the clinical area to render it fit for safe patient care The overall need to admit new patients to the ward The staff/patient ratio in outbreaks that have debilitated the staff numbers Other organisational factors. 6.9 TERMINAL CLEANING AND DISINFECTION The timing of the terminal clean process should ideally be at least 72-hours post the last uncontrolled episode of vomiting or diarrhoea. The presence on the ward of isolated patients with unformed but contained faeces (i.e. delivered directly into a toilet or bedpan) should not delay the start of terminal cleaning 7. TRAINING REQUIREMENTS The IPCT will work with the Modern Matrons, Clinical Directors, clinical leads and infection control link advisors to improve adherence to infection control policies and guidelines. The IPCT will provide induction and ongoing education through the Setting Direction and Patient Safety study days. Prevention and Management of Viral Diarrhoea and Vomiting Version: 2 Issue Date: 11 April 2017 Review Date: 10 April 2020 (Unless requirements change) Page 8 of 16 All staff have a duty of care to their patients to ensure they deliver a high standard of care in line with current research and recommendations. Modern Matrons / Service Leads have a duty to report any deficiencies in knowledge and ensure appropriate training is undertaken. Modern Matrons / Service Leads must ensure that all staff attend annual mandatory infection prevention updates according to hospital policy. 8. REFERENCES AND ASSOCIATED DOCUMENTATION 1. Polage CR, Solnick JV, Cohen SH. Nosocomial diarrhea: evaluation and treatment of causes other than Clostridium difficile. Clin Infect Dis 2012; 55: 982–989. 2. Ahmed SM, Hall AJ, Robinson AE, et al. Global prevalence of Norovirus in cases of gastroenteritis: a systematic review and meta-analysis. Lancet Infect Dis 2014; 14: 725–730. 3. Harris JP, Adams NL, Lopman BA, Allen DJ, Adak GK. The development of web-based surveillance provides new insights into the burden of Norovirus outbreaks in hospitals in England. Epidemiol Infect. 2014; 142: 1590–1598. 4. Lopman BA, Reacher MH, Vipond IB, et al. Epidemiology and cost of nosocomial gastroenteritis, Avon, England, 2002-2003. Emerg Infect Dis 2004; 10: 1827–1834. 5. Danial J, Cepeda JA, Cameron F, Cloy K, Wishart D, Templeton KE. Epidemiology and costs associated with Norovirus outbreaks in NHS Lothian, Scotland 2007-2009. J Hosp Infect 2011; 79: 354–358. Prevention and Management of Viral Diarrhoea and Vomiting Version: 2 Issue Date: 11 April 2017 Review Date: 10 April 2020 (Unless requirements change) Page 9 of 16 9. EQUALITY IMPACT STATEMENT Portsmouth Hospitals NHS Trust is committed to ensuring that, as far as is reasonably practicable, the way we provide services to the public and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds. This policy has been assessed accordingly Our values are the core of what Portsmouth Hospitals NHS Trust is and what we cherish. They are beliefs that manifest in the behaviours our employees display in the workplace. Our Values were developed after listening to our staff. They bring the Trust closer to its vision to be the best hospital, providing the best care by the best people and ensure that our patients are at the centre of all we do. We are committed to promoting a culture founded on these values which form the ‘heart’ of our Trust: Respect and dignity Quality of care Working together Efficiency This policy should be read and implemented with the Trust Values in mind at all times. Prevention and Management of Viral Diarrhoea and Vomiting Version: 2 Issue Date: 11 April 2017 Review Date: 10 April 2020 (Unless requirements change) Page 10 of 16 10. MONITORING COMPLIANCE WITH PROCEDURAL DOCUMENTS This document will be monitored to ensure it is effective and to assure compliance Minimum requirement to be monitored Lead All diarrhoea and vomiting patients routinely monitored via the infection prevention team IPCT Time to isolate monitored by the infection prevention team IPCT Tool VitalPAC and IPC Manager Frequency of Report of Compliance Monthly Reporting arrangements Policy audit report to: Lead(s) for acting on Recommendations Dr Caroline Mitchell Matrons NMAC IPMC VitalPAC and IPC Manager Monthly Policy audit report to: Dr Caroline Mitchell Matrons NMAC IPMC Number of outbreaks reported as KPI monthly to Trust Board and CSC’s via dashboard IPCT Annual outbreak report to be compiled by infection prevention team IPCT Data Manager Monthly Data logs Annual Prevention and Management of Viral Diarrhoea and Vomiting Version: 2 Issue Date: 11 April 2017 Review Date: 10 April 2020 (Unless requirements change) Policy audit report to: Dr Caroline Mitchell Trust Board Policy audit report to: Trust Board Page 11 of 16 Dr Caroline Mitchell APPENDIX A: WARD SYMPTOM MONITORING FORM No. Hospital No. Forename Surname Bed No. 1. Symptoms Commencing D D&V V 2. D D&V V 3. D D&V V 4. D D&V V 5. D D&V V 6. D D&V V 7. D D&V V 8. D D&V V 1. Underlying Diagnosis, Antibiotics / Laxatives / Feeds, relevant information 2. Underlying Diagnosis, Antibiotics / Laxatives / Feeds, relevant information 3. Underlying Diagnosis, Antibiotics / Laxatives / Feeds, relevant information 4. Underlying Diagnosis, Antibiotics / Laxatives / Feeds, relevant information 5. Underlying Diagnosis, Antibiotics / Laxatives / Feeds, relevant information 6. Underlying Diagnosis, Antibiotics / Laxatives / Feeds, relevant information 7. Underlying Diagnosis, Antibiotics / Laxatives / Feeds, relevant information Prevention and Management of Viral Diarrhoea and Vomiting Version: 2 Issue Date: 11 April 2017 Review Date: 10 April 2020 (Unless requirements change) Page 12 of 16 Specimen Date Specimen Result APPENDIX B: INFORMATION FOR STAFF IMPORTANT NOTICE This area currently has a high number of cases of diarrhoea and vomiting If your visit is essential, please use the hand washing facilities before entering and when leaving the ward or department Please follow all instructions from members of staff If your visit is not essential, we would suggest that you do not visit until the number of cases of diarrhoea and vomiting has reduced CONTACT Infection Prevention & Control Bleep 0064 or via switchboard Prevention and Management of Viral Diarrhoea and Vomiting Version: 2 Issue Date: 11 April 2017 Review Date: 10 April 2020 (Unless requirements change) Page 13 of 16 APPENDIX C: INFORMATION FOR STAFF Norovirus (also known as Small Round Structured Viruses (SRSVs), Norwalk like Viruses, winter vomiting disease) The symptoms are predominately vomiting, diarrhoea, and occasionally fever. Nausea and abdominal pain may also occur. Symptoms last between one to three days and recovery is usually rapid thereafter. It is a virus that is spread from person to person by the faecal-oral route. The vomitus will also be infectious. Criteria for suspecting an outbreak; 1. 2. 3. 4. Vomiting often projectile occurs in more than 50% of cases Unexplained diarrhoea with, or without nausea, fever, and abdominal pain Incubation period of 15-48 hours Staff and patients affected. Control measures for minimising transmission at ward level Isolate symptomatic individuals immediately - only cohort under the guidance of the IPCT Keep all bay and side room doors closed (when safe to do so) Wear gloves and apron for contact with an affected patient or environment Wash hands with soap and water after contact with an affected patient or environment (after removing gloves and apron) Do not use alcohol hand rub to decontaminate hands Remove all exposed food e.g. fruit from lockers etc. and de-clutter all areas Provide fresh drinking water for all patients, dish washer jugs and cups and implement intentional rounding for affected patients to encourage regular sips of fluid Use a freshly prepared chlorine-based agent (e.g. 1000ppm Actichlor plus) to disinfect all surfaces and touch points e.g. door handles, bed rails, tables, chair handles at least twice daily Clean and disinfect vomit and faeces spillages promptly Consider use of antiemetics for patients with vomiting Use clear signage to alert staff and visitors that they are entering a restricted area (Appendix B) and emphasise hand hygiene before and after visiting patients Take time to inform patients and their visitors/ relatives of the nature and extent of the outbreak and the consequences for the patient Provide written information to staff, patients and relatives (Appendix C). Leaflets for patients and visitors can be obtained from medical photography (MPI 10/471) Exclude affected staff from the ward immediately and until 48 hours symptom-free Avoid transfer of patients and staff to unaffected wards or departments (unless medically urgent or for the specific purpose of isolation after consultation with IPCT) Exclude non-essential staff from affected clinical areas Admissions to wards should be risk assessed by the IPCT to prevent the unnecessary introduction of further susceptible individuals Staff working on affected wards must not work in unaffected areas for 48 hours after the end of shift Contact numbers for Infection Prevention and Control: In hours: The Infection Prevention and Control Team (IPCT) on the Clinical Lead Bleep (0064) Out of Hours (inc. weekends): The IPCT via the main hospital switchboard. Prevention and Management of Viral Diarrhoea and Vomiting Version: 2 Issue Date: 11 April 2017 Review Date: 10 April 2020 (Unless requirements change) Page 14 of 16 EQUALITY IMPACT SCREENING TOOL To be completed and attached to any procedural document when submitted to the appropriate committee for consideration and approval for service and policy changes/amendments. Stage 1 - Screening Title of Procedural Document: Prevention and Management of Diarrhoea and Vomiting Date of Assessment 20/02/2017 Responsible Department Infection Prevention Name of person completing assessment Kathryn Noble Job Title Infection Prevention Manager/Analyst Does the policy/function affect one group less or more favourably than another on the basis of : Yes/No Age No Disability Learning disability; physical disability; sensory impairment and/or mental health problems e.g. dementia No Ethnic Origin (including gypsies and travellers) No Gender reassignment No Pregnancy or Maternity No Race No Sex No Religion and Belief No Sexual Orientation No Comments If the answer to all of the above questions is NO, the EIA is complete. If YES, a full impact assessment is required: go on to stage 2, page 2 More Information can be found be following the link below www.legislation.gov.uk/ukpga/2010/15/contents Prevention and Management of Viral Diarrhoea and Vomiting Version: 2 Issue Date: 11 April 2017 Review Date: 10 April 2020 (Unless requirements change) Page 15 of 16 Stage 2 – Full Impact Assessment What is the impact Level of Impact Responsible Officer Mitigating Actions (what needs to be done to minimise / remove the impact) Monitoring of Actions The monitoring of actions to mitigate any impact will be undertaken at the appropriate level Specialty Procedural Document: Specialty Governance Committee Clinical Service Centre Procedural Document: Clinical Service Centre Governance Committee Corporate Procedural Document: Relevant Corporate Committee All actions will be further monitored as part of reporting schedule to the Equality and Diversity Committee Prevention and Management of Viral Diarrhoea and Vomiting Version: 2 Issue Date: 11 April 2017 Review Date: 10 April 2020 (Unless requirements change) Page 16 of 16