* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download There are two types of food poisoning
Survey
Document related concepts
Transcript
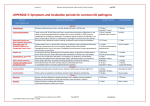
FOOD POISONING & Bacterial causes of acute infectious gastroenteritis What is food poisoning??: • any illness resulting from the consumption of food • There are two types of food poisoning: 1) Food infection refers to the presence of bacteria or other microbes which infect the body after consumption. 2) Food intoxication refers to the ingestion of toxins contained within the food, including bacterially produced exotoxins, which can happen even when the microbe that produced the toxin is no longer present or able to cause infection Food poisoning Food poisoning occurs after: 1- Ingestion of food contaminated with chemical toxin 2- Ingestion of food contaminated with bacterial pathogens and/or their toxins Bacterial food poisoning 1) food poisoning caused by bacterial toxins • Staphylococcus Aureus • Bacillus Cerus • Clostridium perfringens • Clostridium botulinum 2) food poisoning caused by bacterial infection • Salmonella • E. Coli • Shigella spp. • Camplobacter jejuni • Listeria • Yersinia enterocolitis Staphylococcus Aureus Found in human nose and throat (also skin) Salmonella Found in animals, raw poultry and birds Bacillus Cereus Found in soil, vegetation, cereals and spices Clostridium Perfingens Found in animals and birds Clostridium Botulinum Found in the soil and associated with vegetables and meats STAPHYLOCOCCAL FOOD POISONING • Staph. aureus is a common commensal of the anterior nares. • transmission takes place via the hands of food handlers to foodstuffs such as dairy products, including cheese, and cooked meats. • Inappropriate storage of these foods allows growth of the staph. and production of one or more heat-stable enterotoxins. (Toxin may survive boiling for up to 30 minutes. ) • Incubation period 1-6 hrs STAPHYLOCOCCAL FOOD POISONING Clinical features: • Nausea and profuse vomiting develop within 16 hours. • Diarrhoea may not be marked. • Most cases settle rapidly but severe dehydration and rare fatalities have occurred due to acute fluid loss and shock. Management: • Antiemetics and appropriate fluid replacement are the mainstays of treatment. • Suspect food should be cultured for staphylococci and demonstration of toxin production. BACILLUS CEREUS • Ingestion of the heat-stable exotoxins of B. cereus causes rapid onset of vomiting and diarrhoea within hours of food consumption, which resolves within 24 hours. • sources of infections : Fried rice or freshly made vanilla sauces • If viable bacteria are ingested the toxin formation takes place within the gut lumen BACILLUS CEREUS Clinical features • the incubation period is longer (12-24 hours) • Vomiting, watery diarrhoea and abdominal cramps are the predominant symptoms. • The disease is self-limiting but can be quite severe. • Management : Rapid and judicious fluid replacement and appropriate notification of the public health CLOSTRIDIUM PERFRINGENS • Spores of Cl. perfringens are widespread in the guts of large animals and in soil. • If contaminated meat products are incompletely cooked and stored in anaerobic conditions, Cl. perfringens spores germinate and viable organisms multiply to give large numbers. • Subsequent reheating of the food causes heat-shock sporulation of the organisms during which they prduces an enterotoxin. CLOSTRIDIUM PERFRINGENS • Symptoms - Abdominal pain, diarrhoea, occasional vomiting and fever. • Duration is usually 12 to 48 hours. • Clostridial enterotoxins are potent and most people who ingest them will be symptomatic. • Point source' outbreaks, in which nomber of cases all become symptomatic following ingestion, classically occur after school or canteen lunches where meat stews are served. What is botulism food poisoning • Botulism is a disease caused by the bacterium scientifically known as Clostridium botulinum. • Botulism food poisoning occurs when a toxin produced by the bacteria is consumed in improperly preserved foods. The disease is caused by a potent neurotoxin produced by the bacteria. • It manifests as abdominal cramping, double or blurred vision, difficulty breathing, muscle weakness, and other serious symptoms. • Botulism is not spread from person to person. CAMPYLOBACTER JEJUNI • This infection is essentially a zoonosis. • the organisms originating in the gut of cattle and poultry. • The most common source of the infection is meat, such as chicken, or contaminated milk products. • The leading cause of enteritis worldwide • Very low infective does required to cause infection • The incubation period is 2-5 days. • Colicky abdominal pain, which may be quite severe and mimic surgical pathology, occurs with nausea, vomiting and significant diarrhoea, frequently containing blood. CAMPYLOBACTER JEJUNI • The majority of Campylobacter infections affect fit young adults • Infection is self-limiting, 5-8 days, then individuals become carriers for up to 4 weeks • About 10-20% will have prolonged symptomatology, occasionally meriting treatment with antibiotics such as ciprofloxacin 500 mg twice daijy for 5- 7 days . • Approximately 1% of cases will develop bacteraemia and possible distant foci of infection. • Post infection complicatin could lead to Guillain-Barre’ syndrome ( acute post-infective polyneuritis) Salmonella spp.(non-typhohdal) infection • Salmonella serotypes (other than S. typhi and S. paratyphi ), are subdivided into five distinct subgroups which produce gastroenteritis. • Second leading cause of enteritis worldwide • Two serotypes are most important world-wide: S. enteritidis S. typhimurium . • Infected personnel become carriers • Infection requires low does (estimated 200 cells) • Transmission is by contaminated water or food, particularly poultry, egg products and related fast foods. Salmonella infection • The incubation period of Salmonella gastroenteritis is 12-72 hours and • the predominant feature is diarrhoea & vomiting . and blood is quite frequently noted in the stool. • Reactive (post-infective) arthritis occurs in approximately 2% of cases. • Rieter,s disease (arthritis, conjunctivi & urethritis) may occures • Antibiotics are not indicated for uncomplicated Salmonella gastroenteritis. • However, evidence of bacteraemia is a clear indication for antibiotic therapy MOST COMMON CAUSES OF TRAVELLERS' DIARRHOEA • • • • • Enterotoxigenic E. coli (ETEC) Shigella spp. Campylobacter jejuni Salmonella spp. Non-cholera Vibrio spp. ESCHERICHIA COLI • Many serotypes of this major member of the Enterobacteriaceae may be present in the human gut at any given time. • Types of E. Coli Enterotoxigenic E. coli (ETEC) Entero invasive E. Coli (EIEC) Enteropathogenic E. coli (EPEC) Entero-aggregative E. coli (EAEC): Enterohaemorrhagic E. coli (EHEC): • Travel to unfamiliar areas of the world allows contact with previously unknown strains of endemic E. coli and the development of travellers' diarrhoea. Enterotoxigenic E. coli (ETEC) : • These cause most cases of travellers' diarrhoea in developing countries. • The organisms produce either heat-labile enterotoxin or heat-stable enterotoxin, causing marked secretory diarrhoea and vomiting after 1-2 days' incubation. • The illness is usually mild and self-limiting after 3-4 days. • Antibiotics, such as ciprofloxacin, have been used to limit the duration of symptoms but are of questionable value. Entero-invasive E. coli (EIEC): • This illness is very similar to Shigella dysentery and is caused by invasion and destruction of colonic mucosal cells. • No enterotoxin is produced. • Acute watery diarrhoea, abdominal cramps and some scanty blood-staining of the stool are common. • The symptoms are rarely severe and are usually selflimiting. Enteropathogenic E. coli (EPEC): • These are very important in infant diarrhoea. • Ability to attach to the gut mucosa is the basis of their pathogenicity. • This causes destruction of microvilli and disruption of normal absorptive capacity. • The symptoms vary from mild non-bloody diarrhoea to quite severe illness. • Bacteraemia/septicaemia is virtually unheard of. • These strains have the genetic codes for adherence to the mucosa but also produce a locally active enterotoxin. • They have been associated with prolonged diarrhoea. Enterohaemorrhagic E. coli (EHEC): • E. coli O157:H7 is perhaps the best known verocytotoxigenic E. coli (VTEC). • The reservoir of infection is in the gut of herbivores. Sources of infection • contaminated water which is used to irrigate vegetable crops • contaminated milk • meat products (especially hamburgers which have been incompletely cooked) • lettuce and apple juice • Enterohaemorrhagic E. coli (EHEC): • The incubation period is between 1 and 7 days. • Initial watery diarrhoea becomes frankly and uniformly blood-stained in 70% of cases and is associated with severe and often constant abdominal pain. • There is little systemic upset, vomiting or fever. • Enterotoxins, if produced, have both a local effect on the bowel and a distant effect on particular body tissues such as glomerular apparatus, heart and brain. • The potentially life-threatening haemolytic uraemic syndrome (HUS) occurs in 10-15% of sufferers from this infection, arising 5-7 days after the onset of symptoms. • It is most likely at the extremes of age, is heralded by a high peripheral leucocyte count and may be induced, particularly in children, by antibiotic therapy. • HUS is treated by dialysis plasma exchange. ANTIBIOTIC-ASSOCIATED DIARRHOEA (CL. DIFFICILE INFECTION) • A history of any antibiotic therapy in the 6 weeks prior to the onset of diarrhoea can be related to the finding of Cl. difficile or its toxins in the stool. • This is a potent cause of diarrhoea and can produce life-threatening pseudomembranous colitis. • This diagnosis is by stool ex. For cl. Difficile cytotoxin stool culture for cl. Difficile • Treatment metronidazole 400 mg 8-hourly for 10 days. vancomycin may be used (125 mg orally6-hourly for 1 week). • YERSINIA ENTEROCOLITICA • This organism, commonly found in pork, causes mild to moderate gastroenteritis mesenteric adenitis • incubation period of 3-7 days. • It predominantly causes disease in children but adults may also be affected. BACILLARY DYSENTERY (SHIGELLOSIS) • Shigellae are Gram-negative rods, closely related to E. coli, that invade the colonic mucosa. • There are four main groups: Sh. dysenteriae, Sh. flexneri, Sh. boydii Sh. sonnei. • In the tropics bacillary dysentery is usually caused by Sh. Flexneri. • The organism only infects humans and its spread is facilitated by its low infecting dose of around 10 organisms. Epidemiology of shigellosis: • Spread may occur via contaminated food or flies, but transmission by unwashed hands after defaecation is by far the most important factor. • Outbreaks occur in mental hospitals, residential schools and other closed institutions, • dysentery is a constant accompaniment of wars and natural catastrophes which lead to crowding and poor sanitation. Clinical features • Disease severity varies from Sh. sonnei infections is mild that may escape detection Sh. Flexneri is more severe infections, Sh. dysenteriae may be fulminating and cause death within 48 hours. • In a moderately severe illness, the patient complains of diarrhoea, colicky abdominal pain and tenesmus. Stools are small, and after a few evacuations contain blood and purulent exudate with little faecal material. • Fever, dehydration and weakness with tenderness over the colon occur. Management • Oral rehydration therapy or, if diarrhoea is severe, intravenous replacement of water and electrolyte loss will be necessary. • Antibiotic therapy with ciprofloxacin 500 mg 12hourly for 3 days is effective in known shigellosis and appropriate in epidemics. • The use of antidiarrhoeal medication should be avoided in all but the mildest cases. NON-INFECTIOUS CAUSES OF FOOD POISONING Plant toxins • Legumes and beans produce oxidants which are toxic to people with glucose-6-phosphate dehydrogenase (G6PD) deficiency Consumption produces headache, nausea and fever progressing to severe haemolysis, haemoglobinuria and jaundice (favism). • Many fungal species induce a combination of gastroenteritis and cholinergic symptoms of blurred vision, salivation, sweating and diarrhoea. • Amanita phalloides (death head mushroom) causes acute abdominal cramps and diarrhoea followed by hepatorenal failure, often fatal Chemical toxins • Paralytic shellfish toxin Consumption produces gastrointestinal symptoms within 30 minutes, followed by respiratory paralysis. • Warm-water coral reef fish Consumption produces gastrointestinal symptoms 1-6 hours later with associated paraesthesiae of the lips and extremities, distorted temperature sensation, myalgia and progressive flaccid paralysis. . The gastrointestinal symptoms resolve rapidly but the neuropathic features may persist for months. Chemical toxins • Scombrotoxic fish poisoning Consumption produces symptoms within minutes with flushing, burning, sweating, urticaria, pruritus, headache, colic, nausea and vomiting, diarrhoea, bronchospasm and hypotension. Management is with salbutamol and antihistamines. • Thallium and cadmium can cause acute vomiting and diarrhoea resembling staphylococcal enterotoxin poisoning. References: •www.slideshare.net