* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Diarrhoea and Vomiting
Survey
Document related concepts
Transcript
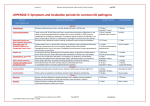
CG10 | VERSION 1.0 1/6 trust clinical guideline Guideline ID CG10 Version 1.0 Title Diarrhoea and Vomiting Approved by Clinical Effectiveness Group Date Issued 01/01/2013 Review Date 31/12/2016 Directorate Clinical Authorised Staff Clinical Publication Category Ambulance Care Assistant Emergency Care Assistant Student Paramedic Advanced Technician Paramedic (non-ECP) Nurse (non-ECP) ECP Doctor Guidance (Green) - Deviation permissible; Apply clinical judgement 1.Scope 1.1 This guideline details the assessment and management of patients experiencing diarrhoea and vomiting. 2. Background and Definitions 2.1Norovirus 2.1.1 Norovirus is the most common cause of infectious gastroenteritis (diarrhoea and vomiting) in England and Wales. The illness is generally mild and people usually recover fully within 2-3 days; there are no long term effects that result from being infected. Infections can occur at any age. The virus is easily transmitted from one person to another. The infectious dose is very low, swallowing as few as 10 - 100 virus particles may be enough to cause illness. 2.1.2 The incubation period is usually 12 to 48 hours, and the infected person commonly presents with sudden onset of nausea, followed by projectile vomiting and watery diarrhoea. Some affected individuals have a raised temperature, headache and aching limbs. The illness is self-limiting and the symptoms will last for 12 to 60 hours, although the person will be infectious for up to 48hrs after the symptoms have fully resolved. responsive committed effective CG10 | VERSION 1.0 2/6 trust clinical guideline 2.2 Clostridium Difficile 2.2.1 Clostridium difficile is a spore forming bacterium which is present as one of the normal bacteria in the gut of up to 3% of healthy adults. It is much more common in babies, with up to two thirds of infants having it in their gut, where it rarely causes problems. People over the age of 65 are more susceptible to contracting the infection. 2.2.2 It is usually kept under control by other bacteria that live in the gut that are essential for maintaining good health. The infection often occurs after someone has taken antibiotics to treat another illness. The medication disturbs the bacteria normally found in the gut and allows Clostridium difficile to multiply. It produces poisons (toxins) which can lead to diarrhoea and severe inflammation of the bowel. 2.3 Other Causes 2.3.1 Food poisoning is caused by someone eating food which may be contaminated with a range of infection causing bugs. Some gastrointestinal infections, such as Campylobacter, can also be caught from pets and other animals. 3.Guidance 3.1Assessment 3.1.1 When assessing the severity of illness consider: ▲▲ Frequency and consistency of stools; ▲▲ The presence of blood in stools; ▲▲ Frequency of vomiting; ▲▲ Ability to eat and drink. 3.1.2 Perform an appropriate examination: ▲▲ Check conscious level, respiratory rates, pulse rate, blood glucose, blood pressure and temperature using an CABCD approach; ▲▲ Assess for abdominal tenderness; ▲▲ Assess for features of dehydration. 3.1.3 Investigate potential causes or contributing factors: ▲▲ Recent contact with someone with acute diarrhoea and/or vomiting; ▲▲ Exposure to a known source of enteric infection (possibly contaminated water or food); ▲▲ Recent travel abroad; ▲▲ Recent antibiotics or hospital admission within the last 8 weeks (suspect infection with Clostridium difficile). responsive committed effective CG10 | VERSION 1.0 3/6 trust clinical guideline 3.2 Clinical Features of Dehydration 3.2.1 Table 1 details the signs and symptoms of different degrees of dehydration. 3.2.2 Table 1 - Dehydration Mild Moderate Severe Lassitude (feeling of weariness, diminished energy). Apathy/tiredness. Profound apathy. Anorexia, nausea. Dizziness. Weakness. Light headedness. Muscle cramps. Confusion, leading to coma. Postural hypotension. Pinched face. Shock. Usually no signs. Dry tongue or sunken eyes. Tachycardia. Reduced skin elasticity. Marked peripheral vasoconstriction. Postural hypotension (systolic blood pressure > 90 mmHg). Systolic blood pressure < 90 mmHg. Tachycardia. Oliguria or anuria (low or no urine output). Oliguria (low urine output). 3.2.3 Children may be at an increased risk when assessing dehydration if: ▲▲ Under one year of age, particularly if under 6 months old; ▲▲ Low birth weight; ▲▲ Past more than 5 diarrhoeal stools in past 24hrs; ▲▲ More than 2 episodes of vomiting in past 24 hours; ▲▲ Children who have not been tolerant of supplementary fluids; ▲▲ Infants who have stopped feeding during the illness ; ▲▲ Children with malnutrition. 3.3Admission 3.3.1 Consider conveying to hospital if: ▲▲ The person is vomiting and unable to retain oral fluids, particularly in infants who have stopped feeding; ▲▲ They have features of severe dehydration. Be alert for the signs of septic shock which are detailed in Clinical Guideline CG21 - Sepsis, Including Meningitis. responsive committed effective CG10 | VERSION 1.0 4/6 trust clinical guideline 3.3.2 Other factors influencing admission (clinical judgement should be used) include: ▲▲ Recent foreign travel; ▲▲ Older age (people 60 years of age or older are more at risk of complications); ▲▲ Home circumstances and level of support; ▲▲ Fever; ▲▲ Bloody diarrhoea; ▲▲ Abdominal pain and tenderness; ▲▲ Faecal incontinence; ▲▲ Diarrhoea lasting more than 10 days; ▲▲ Increased risk of poor outcome, for example: Coexisting medical conditions: Immunodeficiency, inflammatory bowel disease, valvular heart disease, diabetes mellitus, renal impairment, rheumatoid disease, systemic lupus erythematosus; ▲▲ Drugs: Immunosuppressants or systemic steroids, proton pump inhibitors, H2-receptor antagonists, simple antacids, angiotensin-converting enzyme inhibitors, diuretics. 3.3.3 The Diarrhoea and Vomiting Hospital Liaison Guidelines detailed in Appendix 1 must be applied when a patient is conveyed. 3.4Rehydration 3.4.1 In most otherwise healthy adults, encouraging fluid intake (especially if supplemented with fruit juice and soups) will be sufficient. 3.4.2 In adults who are at increased risk of a poor outcome (for example people who are 60 years of age or older, frail, or with comorbidities with which dehydration may be a concern, consider supplementing fluid intake with oral rehydration salt solution. 3.4.3 Consumption of solid food should be guided by appetite. Advise the person to eat small, light meals and avoid fatty, spicy, or heavy food. 3.4.4 In children with suspected gastroenteritis without indication of clinical dehydration, encourage continuation of breastfeeding and other milk feeds. Encourage fluid intake, but discourage the use of fruit juices and any carbonated drinks. 3.5Medication 3.5.1 Anti-diarrhoeal drugs are not usually necessary for the management of gastroenteritis. Anti-motility drugs may be useful for symptomatic control in adults with mild-to-moderate diarrhoea, for example if quicker resolution of responsive committed effective CG10 | VERSION 1.0 5/6 trust clinical guideline diarrhoea would enable the person to continue essential activities. They should be avoided if there is blood and/or mucus in the stools, or high fever. Antibiotics are not recommended for adults with acute diarrhoea of unknown pathology. Anti-emetics are not usually necessary for the primary care management of gastroenteritis. 4. Incident Closure 4.1 Patients must be admitted if indicated under Section 3.3, with the Diarrhoea and Vomiting Hospital Liaison Guidelines applied to ensure a seamless hospital handover. Patients who remain on-scene must be supplied with a copy of the PCR, a patient information leaflet and advised to seek further medical advice if: ▲▲ Their condition does not improve within 48 hours; ▲▲ Symptoms exacerbate or their condition worsens; ▲▲ Warning signs or symptoms develop (such as severe vomiting or dehydration, persistent fever, abdominal distension, or frank blood in stools). 5.Documentation 5.1 In line with Trust Policy, a Patient Clinical Record must be completed and annotated appropriately. Any deviation from this guideline must be recorded, with any potential or actual adverse event reported through the incident reporting system. responsive committed effective CG10 | VERSION 1.0 6/6 trust clinical guideline Appendix 1 - Diarrhoea and Vomiting Hospital Liaison Guidelines Patient presents with sudden onset of diarrhoea and/or vomiting? YES Does the patient present with any of the following: ▲▲Unexpected onset of diarrhoea and/or vomiting? E.g. cannot be explained by other presenting conditions. Examples may include, but are not limited to - recent prescription of medication which may cause D&V, patient vomiting but appears under the influence of alcohol, overdose, recent bowel surgery, heart attack? ▲▲Recent contact with someone with diarrhoea and/or vomiting within the previous 48 hours? ▲▲Resides, works or visits an institution with a known infectious outbreak? ▲▲Taken antibiotics within the previous 14 days? ▲▲Alternative method of feeding present e.g. PEG, naso-gastric tube? YES NO Does the patient’s condition require them to be transported to an Emergency Department Resuscitation Room?* YES Transport patient directly to ED resuscitation room.* State ‘patient likely to require isolation’ during the hospital prealert. Enter department immediately upon arrival at hospital. Is the patient vomiting or actively experiencing diarrhoea following arrival of ambulance clinician? NO YES Transport patient to normal destination. Transport patient to normal destination. Place a hospital prealert specifically to state ‘patient likely to require isolation’. No specific pre-alert regarding infectious status required. On arrival attendant to remain with patient, whilst driver discusses case with senior nurse on duty before patient enters department. If patient’s clinical condition permits attendant to remain with patient on arrival, whilst driver discusses case with senior nurse on duty before patient enters department. NO Transport patient to normal destination. On arrival, convey patient into department. Discuss any issues regarding diarrhoea and/ or vomiting with nurse during routine handover. *May also include transport to catheter laboratory for primary angioplasty, to other condition specific bypasses. responsive committed effective