* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download RENAL SYNDROMES
Survey
Document related concepts
Transcript
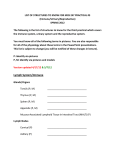
Main kidney syndromes Renal diseases RENAL SYNDROMES • • • • • • • URINARY SYNDROME NEPHROTIC SYNDROME NEPHRITIC SYNDROME ACUTE RENAL FAILURE CHRONIC RENAL FAILURE TUBULAR DISORDERS HYPERTENSION 2 Urinary syndrome Clinical manifestation: latent course, no complaints. Urine tests • Hematuria (commonly microhematuria) • Leucocyturia • Proteinuria (< 3 g/24 h) Nephritic syndrome • Etiology : Infection Vaccinations Systemic diseases • Clinical manifestations edema (face, eye lids) oliguria Hypertension Proteinuria, hematuria («meat slops») ± lung edema, acute renal failure Diagnostic criteria of nephrotic syndrome • • • • • Massive proteinuria (>3.5 g/24 h) Hypoalbuminuria (< 35 g/l) Disproteinemia (hyper-α2-globulinemia) Dislipidemia Edema (due to of serum oncotic pressure and retention of Na ) COMMOM CAUSES OF NEPHROTIC SYNDROME Non-inflammatory glomerulonephritis Minimal change nephropathy Focal and segmental glomerulosclerosis (FSGS) Membranous nephropathy Proliferative/inflammatory glomerulonephritis Mesangiocapillary glomerulonephritis (MCGN) Other “subacute” proliferative nephritis Systemic lipus erythematosus (SLE) (with a variety of histopathological types) Systemic diseases Diabetic nephropathy Amyloidosis 6 CONSEQUENCES AND COMPLICATIONS OF NEPHROTIC SYNDROME Edema Caused by avid sodium retention and hypoalbuminemia Hypercoagulability Presumed relative loss of inhibitors of coagulation Venous thromboembolism is common and sometimes fatal Hypercholesterolemia High rate of arterial occlusions and disease Infection Especially by pneumococci Associated with hypogammaglobulinemia 7 Hypertensive syndrome • Patogenesis : retention of Na and water due to activation of renin-angiotensin-aldosteron system (RAAS) and depression of prostaglandin-callecrein system function. • Clinical manifestation: depends on degree of BP elevation and damage of cardiovascular system Changes in urine appears before increase of BP and usually are moderate Hypertensive syndrome • May be detected in: acute glomerulonephritis acutely progressive (crescent) GN hypertensive and mixed GN chronic pyelonephritis chronic kidney failure renal artery stenosis Uncommon in latent course of chronic GN and chronic interstitial nephritis Tubular abnormalitis Etiology : kidney congenital diseases, pyelonephritis, interstitial nephritis, autoimmune diseases, tumors. • • • • • • • • Polyuria Nocturia < of urine density Nephrogenic osteopathy Electrolytes disorders Glucosuria Acidosis Normal GFR ACUTE RENAL FAILURE (ARF) Deterioration in renal funcction manifestated by an acute rise in serum creatinine and blood urea nitrogen caused by inability to clear water, electrolytes, and nitrogenous wastes, occurring over hours to days/ • Prerenal: reduction in effective circulating volume and renal perfusion or bilateral renal artery occlusion • Intrarenal: vascular, glomerular or tubular injuries • Postrenal: obstruction of urinary tract or bilateral renal veins ACUTE RENAL FAILURE Risk factors • Age (newborns, pregnancy, labor, >60 years) • Metabolic abnormalities (gout, atherosclerosis, diabetes) • Hemodynamic (heart failure, liver cirrhosis) • Drugs (sulfanilamide, antibiotics, ACE inhibitors, contrast nephropathy) • Toxins (alcohol, narcotics) • Trauma (multiple traumas, massive burns, heart surgery) • Renal causes (urinary tract obstruction, nephrotic syndrome, gestosis, chronic renal failure) Prerenal ARF • Ischemic kidney 1. Decreased cardiac output (cardiogenic shock, congestive heart failure, lung embolism) 2. Vasodilation (anaphylactic shock, sepsis, drug indused hypotension) 3. Volume depletion (bleeding, diarrhea, vomiting, polyuria, reduction of effective circulation volume due to hypoalbuminemia) 4. Other reasons for GFR (hypercalciumemia, hepatorenal syndrome) Intrarenal ARF • Exogenous intoxication (poisons, snake bites and stings, drugs) • Acute infection-toxic kidney (hemorrhagic fever, leptospirosis, acute pyelonephritis) • Injury of renal vessels (hemolitico-uremic syndrome, scleroderma, thromboembolic and atheroembolic disease, systemic vasculitis, acute glomerulonephritis, interstitial nephritis, acute tubular necrosis, contrast nephropathy) • Kidneys traumas • Postischemic ARF • Intratubular blok (pathologic cylinders, cristalls) Postrenal ARF • Urinary tract and renal veins obstruction (nephrolithiasis, tumors, retroperitonal fibrosis, renal necrotic papillitis, prostatic hypertrophy, renal vein thrombosis) • Urinary retention (diabetes, spinal cord injury, M-cholinergic antagonists and ganglionic blockers) Clinical manifestation of ARF • Initial stage (I): clinical manifestation of situation leading to ARF • Oligouria or anuria (II): acute development of oligouria or anuria, vomiting, impairment of consciousness, edema, lung and brain edema, of urea, creatinine, potassium, GFR, metabolic acidosis • Restoration of diuresis (III): polyuria, увеличивается количество мочи до степени полиурии, of urea, creatinine, potassium, sodium • Recovery (IV): takes 6-12 monthes Chronic renal failure • Constant and progressive decrease of all kidney functions • Kidneys are incompetent to support normal homeostasis Causes of chronic renal failure Chronic glomerulonphritis Systemic hypertension Diabetes mellitus with nephropathy Chronic obstructive uropathy Polycystic of the kidneys Analgesic nephropathy 18 Signs of chronic renal failure Sallow complection Anaemia (normocytic, normochromic) Uraemic fetor Deep acidotic breathing (Kussmaul respiration) Hypertension Mental clouding Uraemic encephalopathy (flapping tremor) Pleural and pericardial effusion Pericardial rub (pericarditis) Evidence of fluid overload or depletion Renal masses (polycystic kidneys) Large bladder (chronic bladder outlet obstruction) 19 Mechanisms of progression • Activity of disease • hemodinamic – Hyperfiltration and intraglomerular hypertension – Systemic hypertension • Metabolic – ↑phosphorus – – – – ↑ calcium ↑ lipids ↑ glucose ↑ uric acid • Provoking factors infections, UT obstruction, pregnancy, allergic reactions, nephrotoxic drugs, hypovolemia, dehydration, bleeding REVERSIBLE FACTORS IN CHRONIC RENAL FAILURE Hypertension Reduced renal perfusion Renal artery stenosis Hypotension due to drug treatment Sodium and water depletion Decreased cardiac output Urinary tract obstruction Urinary tract infection Other infections: increased catabolism and urea production Nephrotoxic medications 21 Conservative treatment of CRF • Low-protein diet, control of phosphorus and potassium according to level of GFR • Control of BP (target BP < 130/80 mm Hg) • Control of water-salt and acid-base balance • Correction of renal anemia (erythropoetine) • Prophylaxis of hypertireoidism • Excretion of nitrogen rests via GIT • Treatment of infectious complications • Decrease of cardiovascular risk Cardiovascular risk • Cardiovascular risk in patients with CRF is 15-20 times higher then in general population • 40% patients starting dialysis have features of ischemic heart disease Markers of activity of renal disease • • • • • • • Increase of proteinuria Increase of hematuria Sudden increase of BP Rapid increase of creatinin Rapid decrease of GFR Increase of EST Hyper-α2 or gammaglobulinemia • Intravascular blood coagulation Glomerulonephritis Provoking factors • Infection (streptococci, staphylococci, tuberculosis, luis, hepatitis B and C, other viruses, malaria, ricketsiosis) • • • • • • • • • Vacination Systemic diseases, tumors Concomitant diseases Drugs Narcotics Allergic reactions Toxic substances Radiation Overcooling Clinical classification of GN • Acute • Rapidly progressive • Chronic - latent - latent with hematuria - nephrotic - hypertensive - combined Acute GN • Develops in 10-20 days after infection or injury (ß-hemolitic streptococcus, gr. A) • Nephritic syndrome - edema, oliguria BP, hematuria, proteinuria • In some patients - lung edema, eclampcia, ARF • АSLO • In case of cyclic course recovery in 2 -3 weeks • Morphology: diffuse proliferative GN Clinical case 1 • Genesis of nephrotic syndrome Drug-induced? Secondary lues? • Treatment Exclude the intake of carbamazepine and phenobarbital? Treatment of lues? Clinical case 1 • Diagnosis Secondary lues. Acute glomerulonephritis with nephrotic syndrome. Preserved renal function. • Morphology Most common membranose nephropathy with deposits of Ig G, Ig M and Trepanema pallidum on basal membran • Catamnesis In 6 months there were no signs of kidney damage Rapidly progressive GN • Nephritic and/or nephrotic syndrome, BP • Rapid developpment of renal failure (dubbling of creatinine every 3 months) • Without treatment death in 1-2 years • Morphology: creschendic nephritis with “demilunes” • Etiology: systemic vasculitis, systemic diseases, hepatitis C Latent chronic GN • • • • Most common form (44%) Isolated urinary syndrome Rarely BP 10-years survival 88% • Morphology: mesangioproliferative GN Hematuric chronic GN • Episodes of micro- and macrohematuria after flu and respiratory viral infections • More common in males • of Ig A in blood • In most cases – benign course • Morphology: mesangioproliferative GN • Berge disease, alcoholic damage of kidneys Nephrotic GN • • • • • • • Course with exacerbations Edema Proteinuria > 3,5 g/24 h Hypoalbuminuria < 35 g/l ↑of α-2 and γ-globulines Hypercholesterolemia Morphology: minimal changes, membranous and mesangioproliferative GN, focal segmental glomerulosclerosis • Develops in infective endocarditis, systemic diseases, drug induced damage, Alport’s syndrome Hypertensive GN • ↑BP, sometimes malignant • Urinary syndrome (proteinuria < 1g/24 h) • Differential diagnosis with renovascular hypertension, Conn syndrome, pheochromocytoma, essential hypertension, chronic pyelonephritis Combined GN • • • • Nephrotic syndrome Hypertension Chronic renal failure develops in2-3 years Morphology: membranoproliferative GN, focal segmental glomerulosclerosis • Diseases: systemic lupus erythematosus, systemic vasculitis • Differential diagnosis with renal vein thrombosis, acute interstitial nephritis, scleromermic kidney Treatment of glomerulonephritis • If possible detect the etiologic factor and eliminate it • Decrease the activity of the processes • Stabilize the course of disease and decrease the temp of progression (if possible – achieve the involution of disease) Treatment of glomerulonephritis Etiologic treatment - Antibiotics in post-strepthococcal GN and infective endocarditis - Specific treatment of GN associated with lues, malaria, tuberculosis, viral infections - Effective treatment of tumors in case of paraneoplastic nephritis - Exclusion of drugs in drug induced nephritis - Refuse of alcohol in alcoholic nephritis - Exclusion of allergic factor in atopic nephritis Treatment of glomerulonephritis Pathogenic treatment Immunosupression Corticosteroids Cytostatics nonselective alkalizing: cyclophosphamide, clorbutin antimetabolic: azathioprine, metatrexat selective -cyclosporine А -tacrolimus -micofenolat mofetil Monoclonal antibodys (?) Indications for corticosteroids • • • • Nephrotic syndrome in minimal changes disease Rapidly progressive GN Exacerbation of GN in systemic diseases Acute GN with long lasting nephrotic syndrome and increase of creatinin • Exacerbation of GN with first episode of kidney failure and/or nephrotic syndrome • Drug induced GN or interstitial nephritis Mechanism of corticosteroids action • Redistribution of inflammatory and immune system cells in blood flow, prevention of their migration in the kidney tissue • Depression of inflammatory cells proliferation and production of inflammatory mediators Methods of steroid therapy • Prednisolone 1 mg/kg (but not more than 80 mg) every day • Dabbled dose of prednisolone every other day - ↓risk of adrenocortical insufficiency - ↓risk of infective complications • Pulse therapy - IV infusion of very high doses of prednisolone (1000 mg) during 3 days every month Complications of corticosteroid therapy • CNS - psychosis • Bones and muscles - osteoporosis - myopathy • Eyes – glaucoma, cataract • GIT – peptic ulcer, pancreatitis • Cardiovascular system – AH, HF, cardiopathy • Immune system – immunosuppression • Endocrine system and metabolic changes – – – – Steroid diabetes Ameorrhea Cushing syndrome Fatty liver Complications of corticosteroid therapy • Endocrine system and metabolic changes – – – – – ↑of glucose level (steroid diabetes) Dislipidemia Cushing’s syndrome Fatty liver P-Ca metabolism abnormalities - Mechanism of cytostatics agents action • Antimetabolites – impair basic nitrogens synthesis • Alkylating agents – suppress the information reading from DNA and damage the protein synthesis in ribosomes • Cyclosporine А – decrease the activity of Т-helpers, proliferation of В-lymphocytes, production of IL-2 and other cytokines Indications for cytostatics • • • • • Acutely progressive GN Exacerbation of GN in SLE High activity of GN Recurrent and persisting nephrotic syndrome Steroid sensitivity and resistency Complications of cytostatic therapy • • • • • • • • • Decrease of thrombocytes and leucocytes Infections Gastro-intestinal disorders Liver damage Amenorrhea Alopecia Cystitis Teratogenicity Cancer genesis Control of leucocytes is obligatory (neutrophils - > 1500!) Influence on non-immune mechanisms of GN progression • ACE-inhibitors and angiotensin II receptor blockers • Anticoagulants and antiaggregants heparin dipiridamol • Antihiperlipidemic drugs CLINICAL PRESENTATION OF URINARY TRACT INFECTION Asymptomatic bacteriuria Symptomatic acute urethritis and cystitis Acute prostatitis Acute pyelonephritis Septicaemia (usually Gramm-negative bacteria) 49 UNCOMPLICATED AND COMPLICATED URINARY TRACT INFECTION Uncomplicated Anatomically and physiologically normal urinal tract Normal renal function No associated disorder which impairs defense mechanisms Complicated Abnormal urinary tract, e.g. obstruction, calculi, vesicoureteric reflux, neurological abnormality, in-dwelling catheter, chronic prostatitis, cystic kidney, analgesic nephropathy, renal scarring Impaired renal function Associated disorder which impairs defense mechanisms (e.g. diabetes mellitus, immunosuppressive therapy) 50 FACTORS WHICH LIMIT MULTIPLICATION IN THE URINARY TRACT A high rate of urine flow Regular complete bladder emptying Urinary glucosaminoglycans (Tamm - Horsfall mucoprotein) which may bind to E.coli, thus preventing their attachment to urothelium Mucosal defences: this surface layer on glucosaminoglycans, secretion of IgA and IgG, mucosal phagocytosis 51 Investigation of patients with acute urinary tract infection Investigation Indications Culture of MSU or urine obtained by suprapubic aspiration Microscopic examination of urine for white cells, red cells and casts Dipstick examination of urine for blood, protein and glucose Full blood count All patients Plasma urea, electrolytes, creatinine All patients All patients Infants; children; acute pyelonephritis or prostatitis Infants; children; acute pyelonephritis; recurrent UTI 52 Investigation of patients with acute urinary tract infection Blood culture Pelvic examenation Intravenous urography (IVU) including film of bladder after voiding, to identify physiological and anatomical abnormalities Renal ultrasonography Micturating cystourethrography (MCU) to identify and quantitate vesico-ureteric reflux and disturbed bladder emptying Cystoscopy Fever, rigors or evidence of septic shock Women with recurrent UTI Infants; children Men after single UTI Women who (1) have acute pyelonephritis; (2) have recurrent UTI after urinary tract treatment; (3) have had UTI or covert bacteriuria in pregnancy (IVU 6 weeks after delivery) Alternative to IVU to identify obstruction, cysts, calculi Infants; children with abnormal IVU; any patient thought to have a disturbance of bladder emptying Patients with chronic haematuria; patients with a suspected bladder lesion 53