* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download How bacteria cause disease
Neonatal infection wikipedia , lookup
Lyme disease microbiology wikipedia , lookup
Magnetotactic bacteria wikipedia , lookup
Schistosomiasis wikipedia , lookup
Globalization and disease wikipedia , lookup
Molecular mimicry wikipedia , lookup
Triclocarban wikipedia , lookup
Microorganism wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Bacterial cell structure wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Disinfectant wikipedia , lookup
Schistosoma mansoni wikipedia , lookup
Infection control wikipedia , lookup
Marine microorganism wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
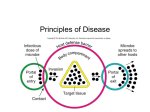
Lecture -1 pathogenic bacteria Dr . Oruba Kuttof al- Bermani Host Microbe- relationships Microorganisms display a variety of complex relationships with other microorganisms and with larger forms of life that serve as hosts for them. A host is any organism that harbors another organism. Symbiosis Symbiosis is an association between two (or more) species. Meaning “living together,” the term symbiosis encompasses a spectrum of relationships. These include mutualism, commensalism, and parasitism. mutualism in which both members of the association living together benefit from the relationshiplarge numbers of Escherichia coli live in the large intestine of humans. These bac teria release useful products such as vitamin K, which we use to make certain blood-clotting factors. Although the relationship is not obligatory, E. coli does make a modest contribution toward satisfying our need for vitamin K. The bacteria, in turn, get a favorable environment in which to live and obtain nutrients 2`Many of the bacteria on human skin are mutualistic. However, most of these organisms are commensals, which indirectly benefit us by competing with harmful organisms for nutrients and preventing those organisms from finding a site to attach to and invade tissue parasitism, in which one organism, the parasite, benefits from the relationship, whereas the other organism, the host, is harmed by itSome parasites obtain com fortable living arrangements by causing only modest harm to their host. Other parasites kill their hosts, thereby rendering themselves homeless . The most successful parasites are those that maintain their own life processes without severely damaging their hosts commensalism in which two species live together in a relationship such that one benefits and the other one neither benefits nor is harmed. For example, many microorganisms live on our skin surfaces and utilize metabolic products secreted from pores in the skin. Because those products are released whether or not they are used by microorganisms, the microorganisms benefit, and ordinarily we are nei ther benefited nor harmed. The line between commensalism and mutualism is not always clear. By taking up space and utilizing nutrients, microbes that show mutualistic or commensalistic behavior may prevent colonization of the skin by other, potentially harmful, disease-causing microbes—a phenomenon known as microbial competition. Hence these symbiotic relationships confer an indirect benefit on the host. There is also a fine line between parasitism and commensalism. In healthy hosts, many microbes of the large intestine form harmless associations, simply feeding off digested food materials. But a ‘harmless’ microbe could act as a parasite if it gains access to a part of the body where it would not normally exist. The situation in which both species harm each other without either benefiting is called antagonism. Contamination, Infection, and Disease Contamination, infection, and disease can be viewed as a sequence of conditions in which the severity of the effects microorganisms have on their hosts increases. Contamination means that the microorganisms are present. The surfaces of skin and mucous membranes can be contaminated with a wide variety of microorganisms. Infection refers to the multiplication of any parasitic organism within or on the host’s body. If an infection disrupts the normal functioning of the host, disease occurs. Disease is a disturbance in the state of health wherein the body cannot carry out all its normal functions . Both infection and disease result from interactions between parasites and their hosts. Sometimes an infection produces no observable effect on the host even though organisms have invaded tissues. More often an infection produces observable disturbances in the host’s state of health; that is, disease occurs. When an infection causes disease, the effects of the disease range from mild to severe Virulence refers to the intensity of the disease produced by pathogens, and it varies among different microbial species. For example, Bacillus cereus causes mild gastroenteritis, whereas the rabies virus causes neurological damage that is nearly always fatal. Virulence also varies among members of the same species of pathogen. For example, organisms freshly discharged from an infected individual tend to be more virulent than those from a carrier, who characteristically shows no signs of disease. The virulence of a pathogen can increase by animal passage, the rapid transfer of the pathogen through animals of a species susceptible to infection by that pathogen. As one animal becomes diseased, organisms released from that animal are passed to a healthy animal, which then also gets sick. If this sequence is repeated two or three times, each newly infected animal suffers a more serious case of the disease than the one before it. Presumably the mi crobe becomes better able to damage the host with each animal passage The virulence of a pathogen can be decreased by attenuation, by repeated subculturing on laboratory media Koch postulates. The first direct demonstration of the role of bacteria in causing disease came from the study of anthrax by the German physician Robert Koch Four criteria that were established by Robert Koch to identify the causative agent of a particular disease, these include: 1. the microorganism or other pathogen must be present in all cases of the disease 2. the pathogen can be isolated from the diseased host and grown in pure culture 3. the pathogen from the pure culture must cause the disease when inoculated into a healthy, susceptible laboratory animal 4. the pathogen must be reisolated from the new host and shown to be the same as the originally inoculated pathogen many organism that do not meet the criteria of posulates have been shown to cuase the diseases For examples, Mycobacterium leprae, the causative agent of leprosy, cannot be isolated in pure culture. additionally to Neisseria gonorrhoeae there is no animal model of infection even though the bacteria can readily be cultured in vitro Figure-1:- Experimental Koch postulates The Disease Process How Microbes Cause Disease Microorganisms act in certain ways that allow them to cause disease. These actions include gaining way access to the host, adhering to and colonizing cell surfaces, invad ing tissues, and producing toxins and other harmful meta bolic products. However, host defense mechanisms tend to thwart the actions of microorganisms. The occur rence of a disease depends on whether the pathogen or the host wins the battle; if it is a draw, a chronic disease may result. How bacteria cause disease Bacterial pathogens often have special structures or phys iological characteristics that improve the chances of suc cessful host invasion and infection. Virulence factors are structural or physiological char acteristics that help organisms cause infection and disease. These factors include structures such as pili for adhesion to cells and tis sues, enzymes that either help in evading host defenses or protect the organism from host defenses, and toxins that can directly cause disease. Direct action of bacteria Bacteria can enter the body by penetrating the skin or mucous membranes, by sexual transmission, by being ingested with food, by being inhaled in aerosols, or by transmission on contaminated object with an infectious agent. If the bacteria are immediately swept out of the body in urine or feces or by coughing or sneezing, they cannot initiate an infection. A critical point in the production of bacterial disease is the organism’s adherence, or attachment, to a host cell’s surface. The occurrence of certain infections depends in part on the interaction between host plasma membranes and bacterial adhesions: are proteins or glycoproteins found on attachment pili (fimbriae) and capsules . Most adhesins that have been identified permit the pathogen to adhere only to receptors on membranes of certain cells or tissues the capsules and attachment pili are also antiphagocytic structures. Attachment to a host cell surface is not enough to cause an infection. The microbes must also be able to colonize the cell surface . Colonization refers to the growth of microorganisms on epithelial surfaces, such as skin or mucous membranes or other host tissues. For colonization to occur after adherence, the pathogens must survive and reproduce despite host defense mechanisms. example, pathogenic bacteria on the surface of skin must withstand environmental conditions and bacteriostatic skin secretions. The degree of invasiveness of a pathogen—its ability to invade and grow in host tissues—is related to the virulence factors the pathogen possesses and determines the severity of disease ,most pathogen have additional virulence factors like enzymes that enable the pathogen to invade tissues. Among bacteria that release enzymes is Streptococci produce hyaluronidase, or spreading factor. This enzyme digests hyaluronic acid, a gluelike substance that helps hold the cells of certain tissues together .Digestion of hyaluronic acid allows streptococci to pass between epithelial cells and invade deeper tissues. Other example is Staphylococcus aureus that produces coagulase to aid in infection Coagulase is a two-edged sword: It keeps organisms from spreading but also helps wall them off from immune de fenses that might otherwise destroy them the bacterial enzyme streptokinase dissolves blood clots. Pathogens trapped in blood clots free themselves to spread to other tissues by secreting these virulence factors A B Enzymatic virulence factors help bacteria invade tissues and evade host defenses. (a) Hyaluronidase dissolves the “cement” that holds together the cells that line the intestinal tract. Bacteria that produce hyaluronidase can then invade deeper cells within the intestinal tissues. (b) Coagulase triggers blood plasma clotting, allowing bacteria protection from immune defenses. Streptokinase dissolves blood clots. Bacteria trapped within a clot can free themselves and spread the infection by producing streptokinase. BACTERIAL TOXINS. A toxin is any substance that is poisonous to other organisms. Some bacteria produce toxins, which are synthesized inside bacterial cells and are classified according to how they are released. Exotoxins are soluble substances secreted into host tissues. Endotoxins are part of the cell wall and are released into host tissues—sometimes in large quantities—from Gram negative bacteria, often when the bacteria die or destroyed endotoxins are produced by certain Gram-negative bacteria. All endotoxins consist of lipopolysaccharide (LPS) complexes They are relatively stable molecules that do not display affinities for particular tissues. Bacterial endotoxins have nonspecific effects such as fever They also cause tissue damage in diseases such as typhoid fever and epi demic meningitis Exotoxins are more powerful toxins produced by sev eral Gram-positive and a few Gram-negative bacteria. Most are polypeptides, which are denatured by heat, ultra violet light, and chemicals such as formaldehyde. Species of Clostridium, Bacillus, Staphylococcus, Streptococcus, and several other bacteria produce exotoxins Some exotoxins are enzymes. Hemolysins were first discovered in cultures of bacteria grown on blood agar plates. The action of these exotoxins is to lyse (rupture) red blood cells Virulence factors called leukocidins are exotoxins produced by many bacteria, including the streptococci and staphylococci. These toxins damage or destroy certain kinds of white blood cells called neutrophils and macrophages Table-1- types of bacterial toxinsb14.5 Properties of Toxins property Organisms producing Location in cell exotoxins Almost all Grampositive; some Gramnegative Extracellular, excreted into medium Chemical nature Mostly polypeptides Stability Unstable; denatured above 60°C and by ultraviolet light Among the most powerful toxins known (some are100 to 1 million times as strong as strychnine) Highly specific; some act as neurotoxins or cardiac muscle toxins Little or no fever Toxicity Effect on tissues Fever production endotoxins Almost all negative Gram- Bound within bacterial cell wall; released upon death of bacterium Lipopolysaccharide complex Relatively stable; can withstand several hours above 60°C Weak, but can be fatal in relatively large doses Nonspecific; ache-allover systemic effects or local site reactions Rapid rise in Antigenicity temperature to high fever stimulates Weak; recovery from production disease often does not produce immunity Strong; antibody and immunity Toxoid conversion and By treatment with heat Cannot be converted to use or chemicals; toxoid toxoid; cannot be used used to to immunize immunize against toxin Many exotoxins have a special attraction for particular tissues. Like Neurotoxins that act on tissues of the nervous system to prevent muscle contraction (botulism) Enterotoxins, such as the toxin that causes cholera, are exotoxins that act on tissues of the gut