* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Activity 1 – Surface Anatomy
Survey
Document related concepts
Transcript
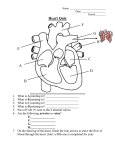
APE 5: Arteries and Veins – Tutor - 2016-17 Lesson Plan Tutors The APE sessions so far have covered surface anatomy of bones, joints and muscles. They have also mapped the peripheral nervous system and learnt about motor and sensory testing. For All APE sessions The aim of APE is to teach clinical skills with surface anatomy. This is not a re-teach of dissection room anatomy. Students must do this as SDL and direct appropriate anatomical questions to the anatomists. These sessions have been lovingly crafted by clinicians. If you have a problem with the content or the way something is taught, please discuss with me directly – we welcome your feedback – but do not change the session It is ok to say ‘I don’t know’ – you are not expected to know everything! Ask me – I am always around Please do not say ‘you need to do it this way for the OSCEs’. Exams are important and motivate people, but this is not the point of these sessions. Good clinical skills are for life, not just for OSCEs! Anatomy of the Physical Examination (APE) Page 1 APE 5: Arteries and Veins – Tutor - 2016-17 Suggested Timing 1 13.3013.35 (5 mins) Activity Introduction Introductions, register Run through objectives Suggested Timing 2 15.3015.35 (5mins) 13.3514.00 (25 mins) Activity 1 – 2: Upper Limb Arteries Draw arteries on volunteer in group Palpate arteries in pairs Allen’s test – Stage 2 demo, Stage 4 in pairs 15.3516.00 (25 mins) 14.0014.25 (25 mins) Activity 3 – 4: Lower Limb Arteries Draw arteries on volunteer Palpate arteries in pairs/on self 16.0016.25 (20 mins) 14.2514.40 (15 mins) Activity 5 – 6: Venous anatomy Draw on UL veins – identify on self Draw on LL veins Answer questions 16.2516.40 (15 mins) 14.4014.45 (5 mins) Activity 7: Doppler demonstration Briefly explain theory/purpose Demonstrate pedal pulse on volunteer 16.4016.45 (5 mins) 14.4515.00 (15 mins) Activity 8 – Clinical context Work through the questions Keep concepts and terminology simple Close and summarise Reiterate learning objectives, signpost SDL, answer any questions 16.4517.00 (15 mins) Anatomy of the Physical Examination (APE) Page 2 APE 5: Arteries and Veins – Tutor - 2016-17 Learning objectives At the end of this session and with SDL students should be able to: Explain the course of major arteries and veins Describe the differences between arteries and veins on examination Know the surface anatomy of important arteries and veins Accurately locate palpable peripheral pulses Recognise a Doppler machine and understand its use. Dress Code T-shirts to allow access to arms, and shorts or trousers that can be rolled up above the knee. Clothing should allow access to abdomen (to palpate abdominal aorta in both males and female students). PE Overview We will be looking at and palpating the clinically important arterial and venous vessels of the upper and lower limb. Activity 1 – Surface Anatomy- Upper Limb Arteries Tutors –. Work as a group ideally drawing on a male volunteer, answering the questions as you go. If they are all unwilling then draw on the laminated man (though this is less preferable) With the help of your tutor, draw the following structures on a volunteer or the laminated man: 1. The arch of the aorta and its branches the brachiocephalic artery common carotid arteries subclavian arteries Look at the image of the aorta below to help visualise this as you draw Tutors – Use bony, muscular or joint landmarks the have already learnt to help define the course of the vessels – get them to identify these on themselves as you go through. You can refer to the crib sheet throughout to help you Anatomy of the Physical Examination (APE) Page 3 APE 5: Arteries and Veins – Tutor - 2016-17 The aorta ascends retrosternally – the arch originates at the level of the right 2nd sternocostal joint and arches to the left and posteriorly On the right, draw the brachiocephalic trunk, splitting into common carotid and subclavian just under the sternoclavicular joint. The common carotids ascend medially to the SCM to the angle of the mandible, lateral to trachea. The subclavians on both sides should arise from behind the sternoclavicular joint and curve supralaterally, passing behind medial third of the clavicle. Diagram of aortic arch and its branches (Accessed and edited http://my.clevelandclinic.org/PublishingImages/heart/aortaLG.jpg 2/8/10) Three branches come off the arch: Brachiocephalic artery – comes off to the right and at the sternoclavicular joint divides into the right subclavian and right common carotid Left common carotid and left subclavian come off from the left side. Anatomy of the Physical Examination (APE) Page 4 APE 5: Arteries and Veins – Tutor - 2016-17 2. The axillary artery Can you recall where the subclavian artery becomes the axillary artery?... Accessed and edited http://home.comcast.net/~wnor/ axillaryartparts.jpg 2/8/10 Tutors – These markers should have been covered in anatomy this morning – as it crosses over first rib 3. The brachial artery And where does it become the brachial? Where does this lie in the cubital fossa? Inferior border of teres major (dark brown muscle in picture). This is one of the muscles that makes up the posterior wall of the axilla – get them to palpate this Draw the artery descending medially to the humerus – crossing the cubital fossa medial to the biceps tendon – again facilitate the students finding this. 4. The radial and ulnar arteries Just distal to the elbow the brachial artery divides into the radial and ulnar artery. What course do these take to the hand? Radial – laterally (radial side forearm); traverses wrist between radial styloid and flexor carpi radialis Ulnar – medially (ulnar side); lateral to flexor carpi ulnaris/pisiform at wrist Anatomy of the Physical Examination (APE) Page 5 APE 5: Arteries and Veins – Tutor - 2016-17 Activity 2 – Palpation of upper limb arteries It is vital to be able to accurately assess the pulse to carry out basic assessments such as calculating heart rate and taking a blood pressure (to be covered in a later sessions). It is also an important skill in the diagnosis and management of certain conditions including peripheral vascular disease. Always feel for a pulse with the tips of your index and middle fingers placed along the line of the artery. Do not press too hard. Always remember to feel pulses bilaterally so you are comparing sides. This can give you clues to pathology. If you are struggling – do not despair! Everyone’s anatomy is a little bit different. Try adjusting your finger position slightly. Tutors – let students work in pairs to locate pulses. Please go around the group and assist. Ensure they are all appropriately explaining the procedure and gaining consent, and using alcohol gel before examining. 1. In pairs, palpate the following arteries on yourself and your partner; remember to use the communication skills from APE 1 throughout this session and ensure hand hygiene. Subclavian – o Gently push down behind the clavicle (about a third of the way from the sternoclavicular joint). o This can be difficult to feel and may not be palpable in everyone. Axillary – o Allow the arm to hang relaxed and place your fingers (or thumb) towards the ‘apex’ of the axilla. o Press against the lateral wall to compress the artery between your fingers and the humerus. Brachial – o Palpate approx.1cm medial to the biceps tendon o Flex the bicep to help locate the tendon Radial – o Palpate between the flexor carpi radialis tendon & the radial styloid. o Flex the wrist to help locate the tendon Ulnar – o Palpate laterally to the flexor carpi ulnaris tendon. o Flex the wrist to help you locate the tendon Anatomy of the Physical Examination (APE) Page 6 APE 5: Arteries and Veins – Tutor - 2016-17 Allen’s Test Most distal arteries are interconnected by smaller blood vessels so that if one became occluded the blood would still be able to flow to supply the tissue adequately. This connection between blood vessels is called an “anastamosis”. Some capillary beds are supplied by only a single artery, called "end-arteries" and if they become blocked the tissue they supply will die. The radial and ulnar arteries anastomose in the hand and therefore it has a dual blood supply Approximately 3% of people do not have this dual blood supply and therefore when inserting arterial lines or taking arterial blood samples from the radial artery you must perform the Allen test. This ensures both arteries are patent (and therefore, should the radial artery be damaged/become blocked, the ulnar artery will continue to perfuse the hand) Tutors – briefly go over the concept above and then demonstrate Allen’s test (stage 2), supervise and assist the students practicing in pairs 2. Watch your tutor demonstrate Allen’s test, then perform this on your partner: Put one thumb over the radial and one over the ulnar artery. Ask your partner to make a tight fist. Press firmly down with both thumbs and then ask your partner to straighten the fingers. The palm will be blanched. Release the thumb over the radial thumb check for prompt flushing of the hand. Repeat the whole test but this time releasing the thumb over the ulnar artery If the hand flushes in both tests your partner has adequate supply from the radial and ulnar artery to their hand. Activity 3 - Surface Anatomy- Lower Limb Arteries With the help of your tutor, draw the following structures on the laminated man initially, then a volunteer: Tutors – draw from distal femoral to pedal arteries 1. The abdominal aorta Do you recall at what level this bifurcates? The thoracic aorta becomes the abdominal aorta as it passes behind the diaphragm at the level of T12. It bifurcates the level of L4 (just above the umbilicus) into the right and left common iliac arteries. Anatomy of the Physical Examination (APE) Page 7 APE 5: Arteries and Veins – Tutor - 2016-17 2. The common iliac arteries and external iliac arteries The common iliac artery bifurcates again and descends as the external iliac to the mid inguinal point. Where is this found? Locate this on yourself. Mid inguinal point = halfway along line drawn from ASIS to pubic symphysis (this should have been covered in APE3) 3. Femoral artery The mid inguinal point marks the start of the femoral artery. What structure does it pass underneath? How does it descend? Inguinal ligament (the ligament runs from the anterior superior iliac spine or ASIS, to the pubic tubercle). Medially, then posteriorly about a hand's breadth above the knee 4. The popliteal artery Where does this begin? The popliteal fossa 5. The posterior and anterior tibial arteries What course do these take to the foot? Posterior artery continues posteriorly and passes behind the medial malleolus. Anterior tibial artery moves anteriorly between the tibial tuberosity and the fibula head, it continues its descend anteriorly, crossing the ankle midway between the malleoli, then lies lateral to extensor hallucis longus (they located this last week) Activity 4 – Palpation of lower limb arteries As before recall your communication and hand hygiene techniques. Tutors – Do 1 together (all to have a go), then let them pair off for 2. Circulate and assist with technique. 1. With the group, palpate the abdominal aorta (female volunteer) o Using both hands held horizontally fingers pointing toward the midline, place your fingers gently either side of the middle in the area above the umbilicus (about 3cm apart). Anatomy of the Physical Examination (APE) Page 8 APE 5: Arteries and Veins – Tutor - 2016-17 palpate the femoral pulse (on yourself +/- a partner’s over their clothing if they consent). o Palpate approx. 2cm below the mid inguinal point Note the iliac arteries cannot be palpated as they are deep structures. 2. Now, in pairs, palpate The popliteal pulse o o The posterior tibialis pulse o Flex the knee to about 120 degrees Place your thumbs on the patella and press your fingers up into the popliteal fossa Palpate approximately 1/3 of the distance from medial malleolus to heel, just behind the medial malleolus. The dorsalis pedis pulse (continuation of anterior tibial) o Palpate just lateral to the extensor hallucis longus tendon in the mid foot. Activity 5 – Surface Anatomy – Upper Limb Veins There are two main groups of veins; the deep and superficial. The deep veins follow the course of the arteries and have the same names. As we have already covered the upper limb arterial system you should be able to name most of the deep upper limb veins. What are they? Subclavian, axillary brachial, ulnar and radial veins. The palmar metacarpal veins and deep palmar venous arch are also in this group. The superficial veins are very useful clinically as site for venepuncture and cannulation (insertion of an intravenous line). On a volunteer (with visible forearm veins) or the laminated man draw the following: 1. The cephalic vein From the superficial veins at the back of the hand, find the vein which runs across the lateral (radial) side of the wrist Trace this as it runs proximally – identify it in the antecubital fossa From here, it continues up the lateral side of the arm Anatomy of the Physical Examination (APE) Page 9 APE 5: Arteries and Veins – Tutor - 2016-17 2. The basilic vein Trace this from the hand again, though this time on the medial (ulnar) border of the forearm and elbow Roughly halfway between the elbow and shoulder the basilic vein becomes deep. 3. The median cubital vein This is a branch of the cephalic vein given off in the antecubital fossa. It runs from the cephalic vein upwards and medially to connect to the basilic vein. The main vessels used for venepuncture are the medial cubital and cephalic veins. Identify and palpate these in your own antecubital fossa. Tutors – Get them to recall how we might make veins more prominent (they did this is APE1) – hang arm down, clench fist, tourniquet (also heat) Note the the variation; ease/difficultly of visualisation – e.g. skin colour. Emphasise that when taking blood, we often ‘feel’ for a vein rather than looking for one – get them familiar with the ‘springy’ feel of a vein. Diagram of cephalic, basilic and median cubital veins (accessed and edited http://www.calgarylabservices.com/files/HealthcareProfessionals/SiteSelection.jpg 9/8/10) Anatomy of the Physical Examination (APE) Page 10 APE 5: Arteries and Veins – Tutor - 2016-17 Activity 6 – Surface Anatomy – Lower Limb Veins Much like the upper limb the lower limb also has two groups of veins; the deep and superficial which are joined by communicating veins. Name the deep veins of the lower limb Common, external and internal, femoral, popliteal, posterior and anterior tibial veins. The digital veins and plantar venous arch are also in this group. The two main superficial veins of the lower limb are the long and short saphenous veins. Draw these on a volunteer or the laminated man: 1. The long/great saphenous vein Starts at the medial half of the dorsum of the foot and crosses the ankle 2cm anterior the medial malleolus Runs medially up the entire leg Drains into the femoral vein 2. The short/small saphenous vein Starts at lateral dorsum of foot and runs behind lateral malleolus Runs posteriorly to popliteal fossa Answer the questions below: How are the saphenous veins sometimes used clinically? Tutors – bypass graft for CABG – esp long saphenous; emphasise this is what a medial lower leg scar might indicate on examination You will have been introduced to femoral triangle today in the DR. Working laterally to medially, can you recall in which order are the femoral artery, nerve and vein are found? NAVY mnemonic –nerve, artery, vein, y-fronts How is this useful clinically? We occasionally need to access the femoral artery or vein for blood taking (‘femoral stab’) or procedures. For example – if you require access to the vein, you would insert your needle medial to the femoral pulse; if you inserted your needle into the femoral triangle and the patient felt a sharp shooting pain down the front of the thigh – what has happened? What should you do with the needle to access the vessels? (femoral nerve, move medially). Also, femoral nerve block – can inject local anaesthetic to numb leg – where would you do this, in relation to the pulse? Medially Anatomy of the Physical Examination (APE) Page 11 APE 5: Arteries and Veins – Tutor - 2016-17 Activity 7 – Doppler Ultrasound tutor demonstration Tutors – do not spend too long on this activity. It is more for clinical interest. Ask for volunteer and try the student’s dorsalis pedis and or posterior tibial artery. Doppler ultrasound A “Doppler” is an important device in the examination of the peripheral vascular system. It detects blood flow in vessels. It is named after Christian Doppler (1842) who was the first to describe the change in the pitch of a note coming from an object that first approaches and then leaves the listener. We are now familiar with this effect from e.g. racing cars or ambulance sirens. This difference in frequency is called the ‘Doppler shift’. If the source itself is silent the same effect can be produced by reflecting a beam of ultrasound off the moving object (in this instance blood) and this is the principle of the “Doppler machines” in clinical use. The reflected signal is converted by the Doppler unit into audible output or a graphical waveform. Uses To assess the arterial blood supply to the lower limb To locate relevant pulses. To obtain an Ankle Brachial Pressure Index (you will do in Semester 2) To assess for venous reflux Your tutor will demonstrate the Doppler machine to you by locating the peripheral pulses in a group member; you will learn to use this equipment in Semester 2. Anatomy of the Physical Examination (APE) Page 12 APE 5: Arteries and Veins – Tutor - 2016-17 Clinical context Work through the following questions with your tutor: 1. a) How would you recognise the difference between arterial bleeding and venous bleeding? Colour - oxygenated blood is brighter red relative to darker venous blood; arterial pulsatile flow and rapid speed of rate of flow b) What is the most useful thing you can do to stop bleeding? Apply pressure, oppose gravity, do not advise a tourniquet unless advice from senior as this could lead to limb ischaemia 2. If the main artery to a limb becomes blocked acutely… a. What colour will the limb become? Pale/white (think of Allen’s…) b. What sort of temperature will the limb be? Cold c. What symptoms might the patient? Pain, paraesthesia/paralysis due to lack of blood supply to tissues/nerves (get them to think what they feel if they have fallen asleep on arm in an awkward position) d. Is this an emergency? Yes – if prolonged this will lead to tissue death (necrosis) which is irreversible. Emphasise the 6 P’s of limb ischaemia – pale, painful, pulseless, paraesthesia, paralysis and ‘perishing’ cold 3. Veins contain unidirectional valves to assist venous blood return to the heart. a. With the help of your tutor see if you can find a valve. Find a vein in the upper or lower limb which is visible over a reasonable length. Compress it distally. ‘Milk’ the blood out of the vein proximally, then release. You will find it does not flow right back to your compressing finger but only as far as a valve, leaving a section of the vein which will only refill if you release the distal compression b. Can you name any conditions where these valves fail? Varicose veins; venous ulcers, chronic venous insufficiency – signpost to SDL – common findings in older patients Anatomy of the Physical Examination (APE) Page 13 APE 5: Arteries and Veins – Tutor - 2016-17 4. a. What is an aneurysm? Dilatation of a blood vessel due to a weakened vessel wall. Can they think of any contexts where they’ve heard of this? These cause particular problems (often fatal) if they rupture b. How might we pick this up on examination? Expansile mass (vs pulsatile) – most common we identify is abdominal aorta – very important to pick up as very high mortality rate if ruptures Please note that we cannot detect all aneurysms on examination – such as cerebral Self-directed Learning 1. Practice your technique of palpating for the all upper and lower limb pulses on yourself any willing volunteers. 2. Read about Deep vein thrombosis – what does this look like on examination? Changes seen in Chronic Venous Insufficiency Anatomy of the Physical Examination (APE) Page 14