* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Respiratory System
Embryonic stem cell wikipedia , lookup
Cell culture wikipedia , lookup
Dictyostelium discoideum wikipedia , lookup
Artificial cell wikipedia , lookup
Chimera (genetics) wikipedia , lookup
Neuronal lineage marker wikipedia , lookup
Organ-on-a-chip wikipedia , lookup
Induced pluripotent stem cell wikipedia , lookup
Hematopoietic stem cell wikipedia , lookup
State switching wikipedia , lookup
Microbial cooperation wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Cell theory wikipedia , lookup
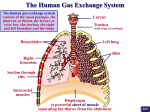
Divisions: o Conducting (upper) Pathway Conduction requires rigidity & flexibility provided by: Cartilage Elastic fibers Smooth muscle fibers Function: transmit air to lower division while warming moistening and removing particulate matter carried out by: Large blood vessels Goblet cells Extensive surface area Coordinated cilia beating Components: Nasal Cavity o Vestibule – inside nostrils Stratified squamous keratinized (slightly) Some sebaceous & sweat glands Some hair follicles Underlying CT blends w/ nasal cartilage perichondrium o Respiratory Portion – main area Respiratory Epithelium = PCCG PCCG = characteristic of maj. of conducting pthwy Pseudostatified Columnar Ciliated – beat synchronously in a posterior direction Goblet cells – produce & secrete mucus which traps particulate matter (muco-ciliary escalator system) Basal Cells – precursors of other cell types Lamina Propria Mucous & serous glands Thin-walled veins to warm air CT blends w/ periosteum or perichondrium of nasal cavity Paranasal Sinuses Continuous w/nasal cavity Lining is slightly thinner (than nasal cavity) o Olfactory Mucosa – roof of nasal cavity Exceptionally tall Pseudostratified columnar LACKS goblet cells Four types of cells: Supporting (sustentacular) Cells o Tall, cylindrical o Broad apex, narrow base o Apical microvilli o Fxn: metabolic & physical support for olfactory cells Sensory Cells (ciliated) o B/w substentacular cells o Somas in middle epithelial layer o Spindle shaped o Bipolar Neurons (continuously replaced every 30-60 days) o Apical dendrite Extends to surface Olfactory vesicle or knob w/ 10-20 modified cilia (nonmotile) Cilia > 100 types of receptor molecules for diff’t odors (degree of intensity + range of odors) Recptors linked to Gproteins (2o messenger inside cell—cAMP) o Proximal cell axon Extends to LP to olfactory bulb of brain Unmyelinated bundles by glial ensheathing cells Brush Cells o Apical microvilli o Fxn in sensation o Presynaptic to afferent fibers Basal Cells o Only cell that does NOT touch apical surface o Small conical cells with dark ovoid nuclei o Mitotically active; able to regenerate (few weeks) Lamina Propria Olfactory glands (or glands of Bowman) o Branched tubuloalveolar glands o Watery secretion Traps odoarants Moisten/cleanse surface o Also secrete Lysozyme Secretory IgA o Short ducts – run thru olfactory epi Lg. unmyelinated olfactory NN cribiform plate olfactory bulb Nasopharynx o Mostly PCCG (Str. Sq. in some areas of abrasion) o Cilia propel material toward oropharynx o LP contains glands (mostly mucous) o Abundant lymphatic tissue (including nasopharyngeal tonsils = adenoids) o Muslces = pharyngeal constrictors Oropharynx Laryngopharynx Larynx o Phonation o Respiratory conduction o Ventricular (false vocal) folds o True vocal folds (w/vocalis m) o Functions Passageway b/w pharynx & trachea Swallowing – mvmts close laryngeal entrance so that food & water cannot enter o Walls: Supporting cartilages (hyaline & elastic) Interconnecting ligaments Intrinsic muscles (skeletal) Extrinsic muscles (skeletal) CT Mucosal lining o Mucosa Abrasive areas: SSNK (vocal folds) Other areas: PCCG (ventricular folds) o Submucosa Mostly mucous glands Vocal folds: Supporting ligament of fibroelastic CT Skeletal muscle (vocalis) Trachea o 10 cm conducting tube maintained open by cartilaginous rings o Mucosa PCCG w/ distinct BM & underlying LP Cells: Ciliated columnar Goblet cells Brush cells: nonciliated columnar w/ μ-villi Basal cells Endocrine (small granule) cells – contractile role o Submucosa LCT with “mixed” glands Band of elastic tissue separates it from mucosa Lymphatic tissue o Cartilagenous layer Fxn: patency (stability) of tube ~ 20 “c”-shaped hyaline cartilages “c” opens posteriorly “c” connected by bundles of smooth mm Adj. rings connected by fibroelastic CT which blends w/ ring perichondrium o Adventitia – external to cartilages (consists of CT, bv’s & NN) Bronchi: 1o (extrapulmonary) 2o (intrapulmonary) 3o (segmental) o 10 total generations of branching o Extrapulmonary bronchi differ from trachea only in diameter o Intrapulmonary bronchi Right = 3; Left = 2 Similar to trachea/Extrapulmonary bronchi except: Initially PCCG gradually SCCG Ciliated: move material up & out Goblet: mucous typically protective, but excess secretion may occlude airway Basal & endocrine cells also present Mucosamuscularissubmucosa (w/glands)cartilagenous layeradventitia c-shaped cartilage replaced by irregular plates of hyaline cartilage of ↓ size Bronchioles o 1 mm or less in diameter o 10 more generations of branching o Characterized by: Thin walls (relative) No cartilage No submucosal glands More smooth muscle (relative) o Epithelium: Simple columnar ciliated simple cuboidal ciliated Goblet cells replaced by Clara Cells (CC) Clara Cells (nonciliated bronchiolar cells) Dome-shaped apical margin Typical protein-secretory cell morphology o rER o Golgi o Secretory granules Fxn: o Secrete substances to break down noxious material o Secrete component of surfactant (prevents luminal adhesion) o Make CC16 Clara Cell protein Measurable pulmonary marker o Involved in Cl- transport into lumen Water follows Aids in moistening luminal surface Clinical Correlation: lack of Cl- transport is a factor in Cystic Fibrosis o Lamina Propria contains elastic fibers o Muscularis Mucosa Increases Surrounded by Adventitia CT No glands No cartilage o o Terminations Terminal Bronchiole Smallest branch of conducting pthwy Defines pulmonary lobule Divides into 3 generations or respiratory bronchioles (& associated alveolar ducts) Respiratory Bronchiole is a termination in the respiratory pathway (see below) Respiratory (lower) Respiratory Bronchiole (pulmonary acinus) Smallest fxn’l unit of lung -- 1st site of gas XΔ Form in groups of 2 or more by terminal bronchiole division Cuboidal w/ mostly Clara Cells (occasionally ciliated) Alveoli (few) appear as dicerticula of the bronchiole LP contains elastic fibers o Vulnerable to destruction by elastases & proteases o Elasticity loss = emphysema o CT surrounded by circumferential smooth mm layer Alveolar ducts, sacs & alveoli (gas XΔ b/w air & blood) Aveolar Ducts o Thin-walled tubes lined w/ bronchiolar cells o External wall Fibroelastic CT Intermittent bundles of smooth muscle o Termination: Branch to 2 to 4 chambers (atria) Atria branch into Alveoli cluster = alveolar sac (double door) Alveoli (single door) Alveoli o Termainal air space o Site of gas XΔ b/w air & blood Alveolar Lining Cells (lines interalveolar septae & alveolar membrane) o Squamous Alveolar Cells a.k.a. Type I alveolar cells or Type I pneumocytes Form lining of alveolus Freely permeable to gases Covers 95% of the surface (very thin cytoplasm) o Great Alveolar Cells – no active role in gas XΔ a.k.a. Type II alveolar cells or Type II pneumocytes Intermingled w/ small alveolar cells & joined by O.Z. Same # of cells as Type I, but cover 5% of surface Able to proliferate & give rise to both Type I & II Lamellar body secretions: Surfactant components: o Multilamellar bodies or (10%) Rich in phospholipids Discharged into lumen Fxns in surfactant system o Choline (40%) Reduces tension Essential for maintaining patency of alveoli o Cholesterol (50%) Four Proteins (SP-A, SP-B, SP-C & SP-D) o Stabilize surfactant/immune fxn Clinical Correlation Atelactasis o Collapsed alveoli Due to surfactnat deficiency in premature infants Complicated by seepage of fibrin and other proteins from the capillaries into are spaces, forming a hyaline membrane Other Cells o Dust Cells (alveolar macrophages) Highly phagoscytic Very motile Within interaveolar septum & migrating on surface Continuously prduce lysosomal enzymes Many become multinucleate giant cells Usually repopulate from monocytes Can migrate up the respiratory tree, to ultimately be swallowed or may re-enter the CT of the interalveolar septum o Fibroblasts – a few in the septum produce collagenous and elastic fibers Interalveolar Septae (internal walls) o Delicate CT Collagen Elastic Reticular fibers o Capillaries (major structural element - scaffolding) 2 layers of epithelium w/ BM’s enmeshed in elastin & fine collagen fibers o Alveolar pores (pores of Kohn) Allow air to pass b/w alveoli Equalization of pressure b/w alveoli Provide collateral air circulation if another bronchiole becomes obstructed Alveoli Membrane (external walls) o Gas XΔ occurs at thinnest portion: Surfactant Type I alveolar cell BL of Type I (sometimes fused) BL of capillary endothelial cell (sometimes fused) Capillary endothelial cell Pleura, blood vessels & lymphatics: o Pleura – mesothelium covering lungs o Arteries: Pulmonary & bronchial arteries accompany the branches of the bronchial tree Arteries give rise to capillary plexus at level of alveolar duct o Veins course in the septae o Lymphatic vessels also present