* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download ABSTRACT:
Coronary artery disease wikipedia , lookup
Artificial heart valve wikipedia , lookup
Cardiac surgery wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
DiGeorge syndrome wikipedia , lookup
Down syndrome wikipedia , lookup
Williams syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Mitral insufficiency wikipedia , lookup
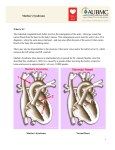
INTRODUCTION: Marfan syndrome is a genetic disorder of the connective tissue. This syndrome is inherited as a dominant trait, carried by the gene FBN1, which encodes the connective protein fibrillin-1. Marfan syndrome has a range of expressions, from mild to severe. The most serious complications are defects of the heart valves and aorta. It may also affect the lungs, the eyes, the dural sac surrounding the spinal cord, the skeleton and the hard palate. Patients with marfan syndrome are at risk for catastrophic aortic complications and mortality. We discuss a case of 26 years old male patient, presenting with acute chest pain and was diagnosed to be a case of marfan syndrome with severe AR with aortic dissection. This case is unique as the patient is on conservative treatment and doing well for last three years, the incidence of such cases reported is very limited. CASE REPORT: A 26 yrs old male presented to us with chief complaints of acute chest pain, of sudden onset, on left side while having his meals. This pain was tearing in nature and was radiating to the back. This pain was not associated with any vomiting or excessive sweating or any loss of consciousness. On examination, patient was tall in stature and thin in built. His BP was 140/70 mm Hg and pulse was 82/min. On general physical examination, long slender limbs were observed with long fingers and toes. He was having increased lower extremity to trunk ratio. There 1 was high arched palate, elongated hands and feet, hyperflexible joints and flat foot. On cardiac examination, early diastolic and decrescendo murmur was heard, which was best heard in the third left intercostal space and was radiating along the left sternal border. There was no evidence of mitral valve prolapse. On abdominal examination, renal bruit was also present. His routine laboratory investigations were in normal limit. His ECG was showing features of left ventricular hypertrophy. Chest X-Ray showed widening of the mediastinum (Fig1). X-Ray of hands and feet showed elongated fingers and toes, respectively (Fig 2). Patient was sent for echocardiography which showed evidence of severe aortic regurgitation. His cardiac MRI showed a flap in the posteromedial wall in the ascending aorta and in the upper abdominal aorta (Fig.3). Immediate surgery was advised but was refused by the patient. Patient is being managed on beta blockers for last 3 years now. DISCUSSION: Marfan syndrome (MFS) is a well-defined genetic defect with both a structural and functional propensity for aortic dissection. Severe elastic fiber degeneration occurs because mutant fibrillin is unable to bind calcium. Sinus dilatation and increased wall stiffness elevate pulse pressure on the structurally attenuated aortic wall. Impaired mechanotransduction (nitric oxide production) causes failure of flow-mediated vaso-dilation with increased wall stress and cardiac workload. 2 Marfan syndrome is a heritable disorder of the connective tissue with a prevalence of ≈1 in 3000 to 5000 individuals. Marfan syndrome affects males and females equally and the mutation shows no ethnic or geographical bias. Marfan syndrome is an autosomal dominant, multisystem disease characterized by long bone overgrowth and other skeletal abnormalities, dislocation of the ocular lens (ectopia lentis), pneumothorax, decreased skeletal muscle mass, mitral valve prolapse, and dilatation of the aortic root. Antoine Bernard-Jean Marfan first described the syndrome in 1896 in a young patient with peculiarly long and thin digits (subsequently termed arachnodactyly), elongated limbs (which he termed dolichostenomelia), and congenital contractures of multiple joints. The most common cardiovascular complication in patients with MFS is progressive aortic root enlargement initially occurring at the sinuses of valsalva. Cardiovascular manifestations in MFS also include valvular disease involving the mitral valve, aortic valve, or both. Mitral valve prolapse is the most prevalent valvular abnormality, affecting 35% to 100% of patients [1]. Other cardiovascular manifestations may include mitral annular calcification, pulmonary artery dilatation, tricuspid valve prolapse and branch vessel dilatation and dissection. Because of the varying symptoms and signs of aortic dissection depending on the initial intimal tear and the extent of the dissection, the proper diagnosis is sometimes difficult to make. 3 The diagnosis cannot always be made by history and physical signs alone. Often the diagnosis is made by visualization of the intimal flap on a diagnostic imaging test. The common tests used to diagnose an aortic dissection include a CT scan of the chest with iodinated contrast material and an aortogram or magnetic resonance angiogram (MRA) of the aorta. Trans-oesophageal echocardiography can also prove to be useful. Chest radiography may reveal widening of the mediastinum, obliteration of the aortic knob, depression of the left mainstem bronchus, loss of the paratracheal stripe, and tracheal deviation. A blood D-dimer level less than 500 mcg/mL may be able to rule out the diagnosis of aortic dissection alleviating the need for further imaging [2]. Prevention of aortic dissection is paramount for the marfan patient. Lifelong ßblockade and elective aortic root replacement (at 5.0 cm) transform the long-term outlook. The outlook for patients with marfan syndrome is transformed by elective aortic root replacement [3]. Aortic root dilatation begins in infancy with a maximal rate of diameter increase during the ages of 6–14 years. After this, root enlargement slows, but the increase in radius and decreased wall thickness causes mural stress to rise dramatically. Beta adrenergic blockade retards the rate of dilatation and risk of dissection by reducing wall stress. In those individuals who develop side effects and therefore cannot tolerate β-blockade, verapamil can be considered a second-line therapy 4 [4]. Other medications might be needed to further minimize blood pressure without slowing the heart rate, such as ACE inhibitors and angiotensin II receptor antagonists. The goal of treatment is to slow the progression of aortic dilation and damage to heart valves by eliminating arrythmias, minimizing the heart rate, and minimizing blood pressure. Exercise restriction represents a second approach to reduce hemodynamic stress in MFS [5]. If the dilation of the aorta progresses to a significant diameter aneurysm, causes a dissection or a rupture, or leads to failure of the aortic or other valve, then surgery (possibly a composite aortic valve graft or valve-sparing aortic root replacement) becomes necessary. The traditional threshold that prompts the consideration of prophylactic aortic root replacement in patients with MFS has been predicated on aortic size and recommended when the diameter reaches 5.0 cm. To conclude, since marfan syndrome is not curable, detailed lifelong medical and surgical treatment can greatly prolong life in marfan syndrome. REFERENCES : 1. Van Karnebeek CD, Naeff MS, Mulder BJ, Hennekam RC, Offringa M. Natural history of cardiovascular manifestations in Marfan syndrome.Arch Dis Child. 2001;84:129–37. 2. Shimony, A; Filion, KB, Mottillo, S, Dourian, T, Eisenberg, MJ (2011-0415). "Meta-analysis of usefulness of d-dimer to diagnose acute aortic dissection". The American journal of cardiology 107 (8): 1227–34. 5 3. Gott V.C., Pyeritz R.E., Cameron D.E., Green P.S., McKusick V.A. Composite graft repair of Marfan’s aneurysms of the ascending aorta: results in 100 patients. Ann Thorac Surg 1991;52:38-45. 4. Rossi-Foulkes R, Roman MJ, Rosen SE, Kramer-Fox R, Ehlers KH, O'Laughlin JE, Davis JG, Devereux RB. Phenotypic features and impact of beta blocker or calcium antagonist therapy on aortic lumen size in the Marfan syndrome. Am J Cardiol. 1999;83:1364–8. 5. Braverman AC. Exercise and the Marfan syndrome. Med Sci Sports Exerc. 1998;30:S387–95. 6