* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Managing low cardiac output syndrome after congenital heart surgery
Cardiovascular disease wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Electrocardiography wikipedia , lookup
Heart failure wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
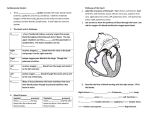
Managing low cardiac output syndrome after congenital heart surgery David L. Wessel, MD P atients with congenital or acquired heart disease comprise a major diagnostic category for admissions in large pediatric intensive care units (ICUs) across the country, compromising 30% to 40% or more of admissions in many centers. Obviously, assessment and treatment of low cardiac output states among patients with heart disease can be life saving. Although some causes of low cardiac output after cardiopulmonary bypass (CPB) are attributable to residual or undiagnosed structural lesions, progressive low cardiac output states do occur (1). A number of factors have been implicated in the development of myocardial dysfunction after CPB, including the following: 1) the inflammatory response associated with CPB; 2) the effects of myocardial ischemia from aortic crossclamping; 3) hypothermia; 4) reperfusion injury; 5) inadequate myocardial protection; and 6) ventriculotomy (when performed). The expression and prevention of reperfusion injury after aortic crossclamping on CPB is currently the subject of intense investigation. Figure 1 shows the typical decrease in cardiac index in newborns after an arterial switch operation. In this group of 122 newborns, the median maximal decrease in cardiac index, which occurred typically 6-12 hrs after separation from CPB, was 32% (2). A quarter of all these newborns reached a nadir of cardiac index that was ⬍2 From Cardiac Intensive Care, Children’s Hospital, and Harvard Medical School, Boston, MA. Key Words: catecholamines; phosphodiesterase inhibitors; extracorporeal membrane oxygenation; cardiopulmonary bypass; milrinone; pulmonary hypertension Address requests for reprints to: David L. Wessel, MD, Director, CICU Office, Children’s Hospital, 300 Longwood Avenue, Boston, MA 02115. E-mail: [email protected] Copyright © 2001 by the Society of Critical Care Medicine S220 L/min/m 2 on the first postoperative night. Low cardiac output states do occur in the postoperative patient, but appropriate anticipation and intervention can do much to avert morbidity or the need for mechanical support (Table 1). Volume Adjustments After CPB, the factors that influence cardiac output, preload, afterload, myocardial contractility, heart rate, and rhythm must be assessed and manipulated. Volume therapy (increased preload) is commonly necessary, followed by appropriate use of inotropic and afterloadreducing agents (3). Atrial pressure and the ventricular response to changes in atrial pressure must be evaluated. Ventricular response is judged by observing systemic arterial pressure and waveform, heart rate, skin color and peripheral extremity temperature, peripheral pulse magnitude, urine flow, core body temperature, and acid-base balance. Preserving and Creating Rightto-Left Shunts Selected children with low cardiac output may benefit from strategies that allow right-to-left shunting at the atrial level in the face of postoperative right ventricular dysfunction. A typical example is early repair of tetralogy of Fallot, when the moderately hypertrophied, noncompliant right ventricle has undergone a ventriculotomy and may be further compromised by an increased volume load from pulmonary regurgitation secondary to a transannular patch on the right ventricular outflow tract. In these children it is very useful to leave the foramen ovale patent to permit right-toleft shunting of blood, thus preserving cardiac output and oxygen delivery, despite the attendant transient cyanosis. If the foramen is not patent or is surgically closed, right ventricular dysfunction can lead to reduced left ventricular filling, low cardiac output, and ultimately, left ventricular dysfunction. In infants and neonates with repaired truncus arteriosus, the same concerns apply and may even be exaggerated if right ventricular afterload is elevated because of pulmonary artery hypertension (4). This concept has been extended to older patients with single-ventricle physiology who are at high risk for Fontan operations. The Fontan circulation relies on passive flow of blood through the pulmonary circulation, without benefit of a pulmonary ventricle. If an atrial septal communication or fenestration is left at the time of the Fontan procedure, the resulting right-toleft shunt helps to preserve cardiac output. These children have fewer postoperative complications (5). It is better to shunt blood right to left, accept some decrement in oxygen saturation, but maintain ventricular filling and cardiac output than to have high oxygen saturation but low blood pressure and cardiac output. Other Strategies Newer strategies to support low cardiac output associated with cardiac surgery in children include the use of atriobiventricular pacing for patients with complete heart block or prolonged interventricular conduction delays and asynchronous contraction. Appreciation of the hemodynamic effects of positive and negative pressure ventilation may facilitate cardiac output. Avoidance of hyperthermia and even induced hypothermia may provide end organ protection during periods of low cardiac output. Finally, anti-inflammatory agents including monoclonal antibodies, competitive receptor blockers, inhibitors of compliment activation, and preoperative preparation with steroids are being actively investiCrit Care Med 2001 Vol. 29, No. 10 (Suppl.) Table 1. Managing low cardiac output syndrome after congenital heart surgery Figure 1. Typical decrease in cardiac index in newborns after an arterial switch operation. gated in an effort to prevent and protect major organs from ischemic injury imposed by CPB and the reperfusion injury associated with the recovery period. Pharmacologic Support Catecholamines. Failure to improve cardiac output after volume adjustments requires the additional use of an inotropic drug (3, 6 –9). Table 2 lists commonly used vasoactive drugs and their actions. Many prefer to use dopamine first in doses of 3–10 g/kg/min. One rarely uses ⬎15 g/kg/min because of the known vasoconstrictor and chronotropic properties of dopamine at very high doses. However, extreme biologic variability in pharmacokinetics and pharmacodynamics defies placing narrow limits on recommended dosages. Dobutamine’s chronotropic and vasodilatory advantages recognized in adults with coronary artery disease have not always proved equally efficacious in clinical studies in children. In fact, dobutamine has fewer, or no, dopaminergic advantages for the kidney. This may be an especially important limitation in infants with excess total body water and interstitial edema. The significant chronotropic effect and increased oxygen consumption induced by isoproterenol have also increasingly limited its use in neonates and infants. Epinephrine is occasionally useful for short-term therapy when high systemic pressures are sought, provided the temporary increase in peripheral vascular resistance can be tolerated. High doses of epinephrine are occasionally necessary to increase pulmonary blood flow across significantly narrowed systemic-to-pulmonary artery shunts when oxygen saturations are low and falling. Arginine vasopressin has been advocated for states of refractory vasodilation associated with low circulating vasopressin levels as may rarely occur after CPB in children (10). Crit Care Med 2001 Vol. 29, No. 10 (Suppl.) I. Extent of the problem A. One quarter of newborns will decrease their cardiac index to ⬍2.0 L/min/m2 after CPB II. Exclude residual disease A. Transesophageal echocardiography and intracardiac catheters provide important anatomic and physiologic data for planning the need for reintervention III. Optimize preload A. Monitor filling pressure and interpret values in light of underlying cardiac disease IV. Enable R3L shunting for right heart failure A. Newborn after right ventriculotomy (TOF and truncus arteriosus) B. Baffle fenestration in patients undergoing a Fontan operation helps preserve cardiac output and oxygen delivery and reduces right atrial pressure C. Preserving a R3L shunt in patients with known elevation in pulmonary vascular resistance may preserve cardiac output during postoperative pulmonary hypertensive crises or during CPR V. Pharmacologic support A. Catecholamines 1. Dopamine (5–15 g/kg/min) supports cardiac output and preserves aortic perfusion pressure during weaning from CPB; dobutamine may reduce afterload 2. Prolonged high-dose epinephrine after CPB in neonates is associated with myocardial necrosis and marked diastolic dysfunction and is increasingly avoided B. Afterload reduction 1. Milrinone, a phosphodiesterase inhibitor, increases cardiac output and lowers filling pressures; nitrates are commonly employed as vasodilators 2. Phenoxybenzamine is a potent ␣-blocker and has been advocated as part of the postoperative management of patients with hypoplastic left heart syndrome but has a long duration of action 3. Nitric oxide is a selective pulmonary vasodilator that will reduce afterload on the right heart VI. Rhythm A. A-V sequential pacing is important for arrhythmias, such as JET or complete heart block B. Atrio-biventricular pacing may improve hemodynamics substantially in patients with complete right or left bundle branch block VII. Ventilation/cardiorespiratory interactions A. Positive pressure ventilation reduces left ventricular afterload but decreases preload and may raise pulmonary vascular resistance and RV afterload B. Negative pressure ventilation (Hayek oscillator) may augment R heart function VIII. Hypothermia A. There is renewed interest in lowering core body temperature to 34–35°C for patients in low cardiac output states in an effort to reduce oxygen consumption and to optimize oxygen delivery IX. Ischemia reperfusion injury A. Anti-inflammatory agents including monoclonal antibodies, competitive receptor blockers, inhibitors of compliment activation, and preoperative preparation with steroids are being actively investigated in an effort to prevent and protect major organs from ischemic injury imposed by cardiopulmonary bypass and the reperfusion injury associated with the recovery period X. Mechanical support A. Extracorporeal membrane oxygenation B. Ventricular assist device CPB, cardiopulmonary bypass; R, right; L, left; TOF, tetralogy of Fallot; CPR, cardiopulmonary resuscitation; A-V, atrioventricular; JET, junctional ectopic tachycardia; RV, right ventricular. In the past, the side effects of inotropic support of the heart with catecholamines seemed a lesser concern in children than in adults with an ischemic, noncompliant heart. Tachycardia, an increased enddiastolic pressure and afterload, or increased myocardial oxygen consumption, despite their undesirable side effects, was tolerated by most children in need of inotropic support after CPB. However, with increasing perioperative experience in neonates and young infants, the adverse effects of vasoactive drugs have become more ev- ident. The less compliant neonatal myocardium, like the ischemic adult heart, may raise its end-diastolic pressure during higher doses of dopamine infusion or may develop even more extreme noncompliance. Actual myocardial necrosis caused by high doses of epinephrine infusions has been identified in neonatal animal models after CPB (11, 12). Although these agents do increase the cardiac output, the concomitant increase in ventricular filling pressure is less well tolerated by the immature myocardium than it is in older chilS221 Table 2. Summary of selected vasoactive agents Agent Noncatecholamines Digoxin (total digitalizing dose) Doses (IV) Peripheral Vascular Effect Cardiac Effect Conduction System Effect Increases peripheral vascular resistance 1–2⫹; acts directly on vascular smooth muscle Inotropic effect 3–4⫹; acts directly on myocardium Slows sinus node slightly; decreases A-V conduction more Calcium chloride Calcium gluconate 20 g/kg premature 30 g/kg neonate (0–1 mo) 40 g/kg infant (⬍2 yrs) 30 g/kg child (2–5 yrs) 20 g/kg child (⬎5 yrs) 10–20 mg/kg/dose (slowly) 50–100 mg/kg/dose (slowly) Variable; age dependent; vasoconstrictor Inotropic effect 3⫹; depends on ionized Ca2⫹ Slows sinus node; decreases A-V conduction Nitroprusside 0.5–5 g/kg/min 0.5–10 /kg/min Amrinone 1–3 mg/kg loading dose 5–20 g/kg/min maintenance 50 g/kg loading dose 0.25–1.0 /kg/min maintenance 0.003–0.002 U/kg/min Indirectly increases cardiac output by decreasing afterload Decreases preload, may decrease afterload; reduces myocardial work related to change in wall stress Diastolic relaxation (lusitropy) Reflex tachycardia Nitroglycerin Donates nitric oxide group to relax smooth muscle and dilate pulmonary and systemic vessels Primarily venodilator; as a nitric oxide donor may cause pulmonary vasodilation and enhance coronary vasoreactivity after aortic cross-clamping Systemic and pulmonary vasodilator; thrombocytopenia As above; shorter half-life As above As above Potent vasoconstrictor No direct effect None known Milrinone Vasopressin Peripheral Vascular Effect Agent Dose Range Alpha Beta2 Delta Beta1 Beta2 Catecholamines Phenylephrine 0.1–0.5 g/kg/min 4⫹ 0 0 0 0 Isoproterenol 0.05–0.5 g/kg/min 0 4⫹ 0 4⫹ 4⫹ Norepinephrine 0.1–0.5 g/kg/min 4⫹ 0 0 2⫹ 0 Epinephrine 0.03–0.1 g/kg/min 0.2–0.5 g/kg/min 2⫹ 4⫹ 1–2⫹ 0 0 0 2–3⫹ 4⫹ 2⫹ 3⫹ Dopamine 2–4 g/kg/min 4–8 g/kg/min ⬎10 g/kg/min 2–10 g/kg/min 0 0 2–4⫹ 1⫹ 0 2⫹ 0 2⫹ 2⫹ 2⫹ 0 0 0 1–2⫹ 1–2⫹ 3–4⫹ 0 1⫹ 2⫹ 1–2⫹ Dobutamine Minimal Minimal tachycardia Cardiac Effect Comment Increases systemic resistance, no inotropy; may cause renal ischemia; useful for treatment of TOF spells Strong inotropic and chronotropic agent; peripheral vasodilator; reduces preload; pulmonary vasodilator; limited by tachycardia and oxygen consumption Increases systemic resistance; moderately inotropic; may cause renal ischemia Beta2 effect with lower doses; best for blood pressure in anaphylaxis and drug toxicity Splanchnic and renal vasodilator; may be used with isoproterenol; increasing doses produce increasing ␣-effect Less chronotropy and arrhythmias at lower doses; effects vary with dose similar to dopamine; chronotropic advantage compared with dopamine may not be apparent in neonates A-V, atrioventricular; TOF, tetralogy of Fallot. dren. Many of the complex corrective procedures performed in neonates and small infants are accompanied by transient postoperative arrhythmias that are either induced or exacerbated by catecholamines, which can have a profound adverse effect on the patient’s recovery after surgery. Diastolic function is crucial in older patients with single ventricles and can be adversely affected by catecholamines. Nevertheless, the predictable and often significant decrease in cardiac output documented by many investigators after CPB in infants and S222 older children continues to justify the practice of judiciously using inotropic agents to support the heart and circulation while weaning them from CPB and during the immediate postoperative period (6). Phosphodiesterase III Inhibitors. Amrinone and milrinone have emerged as important inotropic agents for use in children after open heart surgery. They are nonglycosidic, noncatecholamine inotropic agent with additional vasodilatory and lusitropic properties. They have been used extensively in adults for the treatment of chronic congestive heart failure and, more recently, introduced to pediatric practice (5, 13, 14). These drugs exert their principal effects by inhibiting phosphodiesterase, the enzyme that metabolizes cyclic adenosine monophosphate (cAMP). By increasing intracellular cAMP, calcium transport into the cell is favored, and the increased intracellular calcium stores enhance the contractile state of the myocyte. In addition, the reuptake of calcium is a cAMP-dependent process, and these agents may, therefore, Crit Care Med 2001 Vol. 29, No. 10 (Suppl.) enhance diastolic relaxation of the myocardium by increasing the rate of calcium re-uptake after systole (lusitropy). The drug also appears to work synergistically with low doses of ß-agonists and has fewer side effects than other catecholamine vasodilators, such as isoproterenol. Although the use of amrinone, beginning in the operating room, has become more commonplace in many cardiovascular centers (9, 15), the half-life of 2– 4 hrs rather than minutes and its potential toxicity in the face of hepatic and renal failure have discouraged some from using this drug more frequently. Milrinone has the advantage of a shorter halflife and may, therefore, be more titratable in the face of hemodynamic instability (16, 17). It also may have a lower incidence of thrombocytopenia and is preferable when longer term use of a phosphodiesterase inhibitor is indicated. Other Afterload-Reducing Agents. When systemic blood pressure is elevated and cardiac output appears low or normal, a primary vasodilator is indicated to normalize blood pressure and to decrease the afterload on the left ventricle. This is especially true for the newborn myocardium, which is especially sensitive to changes in afterload and tolerates elevated systemic resistances poorly. Although nitroprusside has no known direct inotropic effects, this potent vasodilator has the advantage of being readily titratable and possessing a short biologic half-life. Use of nitroglycerin avoids the toxic metabolites, cyanide and thiocyanate, associated with nitroprusside use (especially in hepatic and renal insufficiency), but its potency as a vasodilator is less than that of nitroprusside. Inhibitors of angiotensin-converting enzyme have proven to be important adjuvants to chronic anticongestive therapy in pediatric patients. Intravenous forms are available and may be useful in the treatment of systemic hypertension immediately after coarctation repair or when afterload reduction with these inhibitors would benefit patients unable to receive oral medications (18). control of right ventricular afterload (21– 24). Although it is understandable to presume that postoperative patients with pulmonary hypertension have active and reversible pulmonary vasoconstriction as the source of their pathophysiology, the critical care physician is obligated to explore anatomical causes of mechanical obstruction that impose a barrier to pulmonary blood flow. Elevated left atrial pressure, pulmonary venous obstruction, branch pulmonary artery stenosis, or surgically induced loss of the vascular tree all will raise right ventricular pressure and impose an unnecessary burden on the right heart. Similarly, a residual or undiagnosed left-to-right shunt will raise pulmonary artery pressure postoperatively and must be addressed surgically. Extended use of pulmonary vasodilator strategies will only augment residual or undiagnosed shunts and increase the volume load on the heart Several factors peculiar to CPB may raise pulmonary vascular resistance: microemboli, pulmonary leukosequestration, excess thromboxane production, atelectasis, hypoxic pulmonary vasoconstriction, and adrenergic events have all been suggested to play a role in postoperative pulmonary hypertension (23, 25). Postoperative pulmonary vascular reactivity has been related not only to the presence of preoperative pulmonary hypertension and left-toright shunts (19, 22, 26), but also to the duration of total CPB (27, 28). Treatment of postoperative pulmonary hypertensive crises has been partially addressed by surgery at earlier ages, pharmacologic intervention, and other postoperative management strategies (Table 3). However, recent developments in vascular biology offer new insights into the possible causes and cor- Pulmonary Hypertension 3. 4. 5. 6. 7. 8. 9. 10. Anatomical Considerations. Children with many forms of congenital heart disease are prone to develop perioperative elevations in pulmonary vascular resistance (19, 20). This may complicate the postoperative course, when transient myocardial dysfunction requires optimal Crit Care Med 2001 Vol. 29, No. 10 (Suppl.) rection of post-CPB pulmonary hypertension. Pulmonary Vasodilators. Success with vasodilators for the treatment of pulmonary hypertension caused by pulmonary vasoconstriction has had mixed results because of systemic vasodilating effects that may predominate and limit effectiveness. Tolazine, prostaglandin E1, and prostacyclin have all been suggested as useful pharmacologic treatments for this condition (Table 4) (29 –32). Nitric oxide (NO) is a selective pulmonary vasodilator that can be breathed as a gas and distributed across the alveoli to the pulmonary vascular smooth muscle. Nitric oxide is formed by the endothelium from L arginine and molecular oxygen in a reaction catalyzed by NO synthase. It then diffuses to the adjacent vascular smooth muscle cells where it induces vasodilation through a cyclic guanosine monophosphate-dependent pathway (33–37). Because NO exists as a gas it can be delivered by inhalation to the alveoli and then to the blood vessels that lie in close proximity to the ventilated lung. Because of its rapid inactivation by hemoglobin, inhaled NO may achieve selective pulmonary vasodilation when pulmonary vasoconstriction exists. It has advantages over intravenously administered vasodilators that cause systemic hypotension and increase intrapulmonary shunting. Inhaled NO lowers pulmonary artery pressure in a number of diseases without the unwanted effect of systemic hypotension. This is especially dramatic in children with cardiovascular disorders and postoperative patients with pulmonary hypertensive crises. Pulmonary vascular endothelial dysfunction may be a contributing factor in post-CPB pulmonary hypertension. Structural damage to the pulmonary endothelium is demonstrable after CPB, Table 3. Critical care strategies for treatment of pulmonary hypertension Encourage 1. 2. Anatomic investigation Opportunities for right-to-left shunt as “pop off” in right heart failure Sedation/anesthesia Moderate hyperventilation Moderate alkalosis Adequate inspired oxygen Normal lung volumes Optimal hematocrit Inotropic support Vasodilators Avoid 1. Residual anatomic disease 2. Intact atrial septum in right heart 3. 4. 5. 6. 7. 8. 9. 10. Agitation/pain Respiratory acidosis Metabolic acidosis Alveolar hypoxia Atelectasis or overdistention Excessive hematocrit Low output and coronary perfusion Vasoconstrictors/increased afterload See text for explanation and detail. S223 Table 4. Pharmacologic agents available as pulmonary vasodilators during acute illness Drug Class Advantages Nitrates Easily titratable, rapid onset and offset ␣-Antagonists Powerful, dense blockade Angiotensin converting enzyme inhibitors Calcium channel blockers Orally active, facilitates myocardial remodeling Prostaglandins (e.g., prostacyclin) Good afterload reduction, increases cardiac output, some pulmonary selectivity, titratable, long-term benefit for remodeling, antiplatelet, and cytoprotective effect Effective for disease states with high endothelin levels; may be tailored to have some pulmonary specificity Increases cardiac output, titratable Endothelin receptor blockers -Agonists Phosphodiesterase inhibitors type III Phosphodiesterase inhibitors type V Inhaled nitric oxide Orally active, best defined role in primary pulmonary hypertension Increases contractile function, reduces afterload, lowers filling pressures, acts synergistically with catecholamines, not arrhythmogenic Orally active, acts synergistically with inhaled nitric oxide to raise cGMP, attenuates withdrawal response to nitric oxide, may have utility as single-agent pulmonary vasodilator Selective potent pulmonary vasodilator, rapid onset, improves intrapulmonary shunt, no myocardial depression, may have benefit from selected longterm applications Disadvantages Nonspecific, tachycardia, tachyphylaxis, cyanide toxicity Nonspecific, very long duration of action, serious systemic hypotension Little effect on pulmonary circulation Myocardial depression, raises end-diastolic pressure, bradycardia, sudden death, hypotension in infants Systemic hypotension, increases intrapulmonary shunt, value in acute illness unproven, longterm administration, requires central vascular access, expensive Clinical experience is preliminary, range of applicable disease states may be limited Nonspecific, tachycardia, increases myocardial oxygen demand, maldistribution of cardiac output, arrhythmogenic Nonspecific, hypotension at high doses for refractory pulmonary hypertension, slightly long duration of action (1–3 hrs) Clinical experience is preliminary, may be nonspecific vasodilator, longer acting oral or intravenous forms under development, concomitant nitrate therapy contraindicated (hypotension) Methemoglobin, nitrogen dioxide, complex delivery, rebound effects, short acting, expensive cGMP, cyclic guanine monophosphate. and the degree of pulmonary hypertension is correlated with the extent of endothelial damage after CPB (27, 28). The decreased pulmonary blood flow on CPB may result in postoperative impairment of endothelial function and the inability to release nitric oxide. Transient pulmonary vascular endothelial cell dysfunction has been demonstrated in neonates and older children by documenting the transient loss of endothelium-dependent vasodilation immediately after CPB (38). NO production measured by exhaled NO is reduced postoperatively (39). This and other evidence provides a theoretical basis for administering NO after surgery. Therapeutic uses of inhaled NO in children with congenital heart disease abound. For example, newborns with total anomalous pulmonary venous connection (TAPVC) frequently have obstruction of the pulmonary venous pathway as it connects anomalously to the systemic venous circulation. When pulmonary venous return is obstructed preoperatively, pulmonary hypertension is severe and demands urgent surgical relief. Increased neonatal pulmonary vasoreactivity, endoS224 thelial injury induced by CPB, and intrauterine anatomical changes in the pulmonary vascular bed in this disease (40) contribute to postoperative pulmonary hypertension. In one study, 20 infants presenting with isolated TAPVC were monitored for pulmonary hypertension. A mean percentage decrease of 42% in pulmonary vascular resistance and 32% in mean pulmonary artery pressure was demonstrated with 80 ppm of NO. There was no significant change in heart rate, systemic blood pressure, or vascular resistance (41). Inhaled NO can also be used diagnostically in neonates with right ventricular hypertension after cardiac surgery to discern those with reversible vasoconstriction. Failure of the postoperative newborn with pulmonary hypertension to respond to NO successfully discriminated anatomical obstruction to pulmonary blood flow from pulmonary vasoconstriction (42). Failure of the postoperative newborn to respond to NO should be regarded as strong evidence of anatomical and possibly surgically remediable obstruction. Patients with TAPVC, congenital mitral stenosis, and other pulmonary venous hypertensive disorders associated with low cardiac output appear to be among the most responsive to NO. These infants are born with significantly increased amounts of smooth muscle in their pulmonary veins. Histologic evidence of muscularized pulmonary veins as well as pulmonary arteries suggest the presence of vascular tone and capacity for change in resistance at both the arterial and venous sites. The increased responsiveness seen in younger patients with pulmonary venous hypertension to NO may result from pulmonary vasorelaxation at a combination of pre- and postcapillary vessels. Successful use of inhaled NO in a variety of congenital heart defects after cardiac surgery has been reported by several groups (43– 46). It may be especially helpful when administered during a pulmonary hypertensive crisis. Descriptions of use after Fontan procedures (47) and after ventricular septal defect repair have been reported, along with a variety of other anatomical lesions. Very young inCrit Care Med 2001 Vol. 29, No. 10 (Suppl.) fants who are excessively cyanotic after a bidirectional Glenn anastomosis do not generally improve oxygen saturation in response to inhaled NO. At the relatively low levels of NO used therapeutically (1– 80 ppm), the metabolic fate of inhaled NO is an accumulation of nitrate and nitrite in plasma, a small increase in methemoglobin but little detectable nitrosylhemoglobin (48). Possible toxicities of inhaled NO include methemoglobinemia because of the intravascular binding to hemoglobin (49), cytotoxic effects in the lung resulting from free radical formation, development of excess nitrogen dioxide, peroxynitrite production, or injury to the pulmonary surfactant system (50). Carcinogenic and teratogenic potential of inhaled NO exist, as well as effects on glutathione metabolism, unknown effects on the immature or immunocompromised lung, potential interaction with other heme containing proteins, and effects on platelet function and hemostasis. Caution should be exercised when administering NO to patients with severe left ventricular dysfunction and pulmonary hypertension. In adults with ischemic cardiomyopathy, sudden pulmonary vasodilation may occasionally unload the right ventricle sufficiently to increase pulmonary blood flow and harmfully augment preload in a compromised left ventricle (51, 52). The attendant rise in left atrial pressure may produce pulmonary edema (53). This is not likely to arise from any negative inotropic effect of NO (54) and may be ameliorated with vasodilators or diuretics. Clinicians should be cognizant of this potential adverse effect during acute testing of unstable patients during cardiac catheterization, even though it has not been reported to occur in children with congenital heart disease. Abrupt withdrawal effects of NO or even rebound pulmonary hypertension are important issues. Appreciation of the transient characteristics of withdrawal of NO may facilitate weaning from NO and has important implications for patients with persistent pulmonary hypertensive disorders when interruption of NO is necessary (41, 55). If the underlying pulmonary hypertensive process has not resolved, then the tendency for an abrupt increase in pulmonary artery pressure may be hazardous when NO therapy is withdrawn or interrupted (56, 57). If withdrawal of NO is necessary before resolution of the pathologic process, hemodynamic instability may be expected. If a Crit Care Med 2001 Vol. 29, No. 10 (Suppl.) labile patient with pulmonary hypertension is stabilized with NO before transfer to a specialized center for further management, NO should be available during patient transport. Recent work suggests that the withdrawal response to inhaled NO can be attenuated by pretreatment with the type V phosphodiesterase inhibitor, sildenafil (Viagra) (58). Diastolic Dysfunction Occasionally, there is an alteration of ventricular relaxation, an active energydependent process, which reduces ventricular compliance. This is particularly problematic in patients with a hypertrophied ventricle undergoing surgical repair, e.g., tetralogy of Fallot, and after CPB in some neonates when myocardial edema may significantly restrict diastolic function (i.e., “restrictive physiology”). The ventricular cavity size is small, and the stroke volume is decreased. ßAdrenergic antagonists and calcium channel blockers add little to the treatment of this condition. In fact, hypotension or myocardial depression produced by these agents frequently outweighs any gain from slowing the heart rate. Calcium channel blockers are relatively contraindicated in neonates and small infants because of their dependence on transsarcolemmal flux of calcium both to initiate and sustain contraction. A gradual increase in intravascular volume to augment ventricular capacity, in addition to the use of low doses of inotropic agents, has proven to provide a modest benefit in patients with diastolic dysfunction. Tachycardia must be avoided to optimize diastolic filling time and to decrease myocardial oxygen demands. If low cardiac output continues despite the above-outlined treatment, therapy with vasodilators can be attempted to alter systolic wall tension (afterload) and, thus, decrease the impediment to ventricular ejection. Although, intuitively, one may hesitate to use vasodilators in the presence of marginal systemic arterial blood pressure because blood pressure is the product of cardiac output and systemic vascular resistance, a decrease in systemic vascular resistance could increase flow with no undesirable changes in pressure (3). Because the capacity of the vascular bed increases after vasodilation, simultaneous volume replacement is indicated. Amrinone, milrinone, or enoximone are useful under these circumstances because these agents are non-catecholamine so-called inodilators with vasodilating and lusitropic (improved diastolic state) properties, in contrast to other inotropic agents (59 – 64). Mechanical Support For more refractory but potentially reversible ventricular dysfunction, ventricular assist devices may be useful when gas exchange appears satisfactory (65). Although this technique offers potential advantages for selected patients over extracorporeal membrane oxygenation (ECMO), ECMO is indicated when pulmonary function is also significantly impaired (66, 67). It is also more reliable therapy for biventricular dysfunction. In our experience, which is similar to many other centers, mechanical support is necessary in ⬍2% of all patients who undergo CPB (68). The availability of extracorporeal cardiorespiratory support for children with congenital heart disease has had a dramatic impact on a broad range of issues in the ICU (66, 69 –78). Prolonging intraoperative CPB for cardiac surgical patients returning to the ICU was an early and obvious extension of CPB technology. The effect on hospital mortality is unequivocal and even more obvious when used as rescue therapy during cardiopulmonary resuscitation (CPR) (79, 80). However, the impact is felt across many disciplines, including medicine, surgery, nursing, pharmacy, and respiratory therapy, and involves cardiovascular surgeons, cardiologists, intensivists, anesthesiologists, neonatologists, and ECMO specialists. Extracorporeal cardiorespiratory support has expanded our options for supporting reversible heart failure and utilizing organ transplantation (81, 82). It has enabled us to perform difficult catheter interventions in unstable patients and allowed treatment of lifethreatening arrhythmias with catheter ablation techniques. It has altered the way intensive care physicians select patients for intervention and conduct CPR, and it has made clinicians confront practical issues of informed consent for starting and stopping potentially life-saving treatment. This in turn has challenged the medical ethicists to opine on study designs involving ECMO and the important issues of parental input and consent. The technology has confused the clergy by introducing ambiguities about the temporal domains of life and death in the ICU. It has put extraordinary demands on S225 administrators and ECMO specialists to provide more time and personnel during an era of cost reduction. The care of these patients provides intellectual challenges in understanding unique pathophysiology and requires expertise that physicians and other healthcare professionals seek to obtain. The intensity and experience associated with using the ultimate resuscitative tool to achieve sudden shifts from near certain death to dramatic recovery is highly motivating and enormously gratifying. Tables 5 and 6 show the cumulative activity through 1999 in the Extracorporeal Life Support Organization registry with survival by diagnostic category. With the advent of high-frequency oscillatory ventilation, use of surfactant, inhaled NO, and other advances in critical care of the newborn, the need for ECMO for hypoxemic respiratory failure has declined since its peak in 1992. Cardiac ECMO (including adults) seems to have declined more recently as adult use of ventricular assist devices (including implantable) has gained acceptance. In contrast, the proportion of children who received ECMO support for congenital or acquired heart disease at Children’s Hospital (Boston, MA) has steadily increased; this is typical of the pediatric experience in many large cardiac centers. More than half of all ECMO runs in our institution are now for cardiovascular support rather than respiratory support. Survival for patients on ECMO after cardiac surgery has also steadily improved but has not reached the survival rates of neonates on ECMO for respiratory failure (Table 6). Substantial institutional variability in patient selection for ECMO makes comparison with published experience difficult. Even within institutions, practice has substantially evolved, and this confounds the interpretation of trends over time. Overall, one can propose that the use of ECMO for cardiovascular support is increasing, and results are improving; however, there is room for further progress (83). Refinement of ECMO personnel and organization to include an in-hospital team for rapid resuscitation may improve outcome (80). During the past year at Children’s Hospital, Boston, ⬎20 patients have been cannulated for cardiovascular support during resuscitation for cardiac arrest; hospital survival exceeds 60%. Survivors among neonates has dramatically improved to 70%, including those patients with hypoplastic left heart synS226 Table 5. Cumulative Extracorporeal Life Support Organization (ELSO) registry data through 1999 Neonatal Respiratory Cardiac Pediatric Respiratory Cardiac Adult Respiratory Cardiac Total Patients Survived ECMO, % Survived to Discharge, % 14,543 1,085 84 55 79 40 1,711 1,642 62 52 55 39 483 244 52 36 49 32 ECMO, extracorporeal membrane oxygenation. Table 6. Cumulative Extracorporeal Life Support Organization registry data through 1999 for neonatal respiratory failure by diagnostic category MAS CD hernia Sepsis PPHN/PFC RDS Pneumonia Other Total Runs Average Run Time Percent Survived 5177 3132 2088 2065 1268 151 740 127 216 138 137 132 216 164 94 55 76 80 80 55 68 MAS, meconium aspiration syndrome; CD, congenital diaphragmatic; PPHN/PFC, persistent pulmonary hypertension of newborn/persistent fetal circulation; RDS, respiratory distress syndrome. drome who have undergone a Norwood operation. Indications for ECMO. General indications for the use of mechanical support in patients with heart disease include inadequate oxygen delivery or a requirement for temporary support during cardiac catheterization interventions. Inadequate oxygen delivery is caused most commonly by low cardiac output, profound cyanosis with intracardiac shunting and cardiovascular collapse, or profound hypoxemia from associate lung disease (Table 7). The most common cause of inadequate oxygen delivery in a pediatric cardiac ICU stems from low cardiac output, which is usually a result of myocardial dysfunction. Ventricular dysfunction may occur as a component of chronic cardiomyopathy or from other causes of congestive heart failure. It may occur more dramatically with acute decompensation, typified by acute fulminant viral myocarditis. Patients who fail to wean from CPB may be converted to an ECMO circuit in the operating room and brought to the ICU in hopes of recovering myocardial function (84). These children typically have poorer survival rates for multifactorial reasons, including severity and complexity of disease, as well as increased bleeding. Other children have progressive myocardial failure after successful weaning from CPB. This typically occurs during the first 24 hrs after cardiac surgery, and subsequent survival may be better in this group of patients after a period of myocardial rest and decompression. Pulmonary hypertensive crises after CPB may be refractory to therapy and necessitate mechanical support of the right heart. These patients are notoriously difficult to resuscitate after cardiac arrest if they have advanced pulmonary vascular obstructive disease. Resuscitation is facilitated if a small right-to-left communication is created or left in place at the time of surgical intervention. Refractory arrhythmias are occasionally controlled only after the heart has been decompressed on ECMO and sufficient time has been gained to achieve adequate pharmacologic control of the arrhythmia. Cardiac arrest may occur suddenly in the postoperative period, without substantial warning. It may also occur as the culmination of progressive postoperative myocardial dysfunction, resistant to therapy. Although anticipation of this event with timely preparation for ECMO is preferable, cannulation during CPR is not uncommon (83). Crit Care Med 2001 Vol. 29, No. 10 (Suppl.) Table 7. Indications and relative contraindications for extracorporeal membrane oxygenation (ECMO) Typical indications for ECMO I. Inadequate oxygen delivery A. Low cardiac output 1. Chronic (cardiomyopathy) 2. Acute (myocarditis) 3. Weaning from CPB 4. Progressive postoperative failure 5. Pulmonary hypertension 6. Refractory arrhythmias 7. Cardiac arrest B. Profound cyanosis 1. Intracardiac shunting and cardiovascular collapse C. Profound hypoxemia 1. Child a) pneumonia or acute respiratory failure exaggerated by underlying heart disease 2. Newborn b) CHD, complicated by other newborn indications for ECMO, such as meconium aspiration syndrome, PPHN, pneumonia, sepsis, respiratory distress syndrome, etc. II. Support for intervention during cardiac catheterization A. Ablation B. Dilation C. Device closure Relative contraindications for ECMO I. End-stage, irreversible, or inoperable disease II. Family, patient directives to limit resuscitation III. Significant neurologic impairment IV. Uncontrolled bleeding within major organs V. Extremes of size and weight VI. Inaccessible vessels during CPR VII. Residual, operable, anatomic lesion (reoperation rather than ECMO) CPB, cardiopulmonary bypass; CHD, congestive heart disease; PPHN, persistent pulmonary hypertension of newborn; CPR, cardiopulmonary resuscitation. Relative Contraindications to ECMO. Although there may be few structural heart defects that preclude the use of ECMO, there are some potentially important contraindications that should be considered (Table 7). Obviously, if the underlying disease is felt to be irreversible or inoperable, common sense may dictate that mechanical support of the circulation merely prolongs a terminal illness that is destined to have a fatal outcome in the near future. However, perspective on the term “inoperable” may vary among healthcare professionals and is closely tied to the parents’ perception of the likelihood of survival and the quality of life during survival. Significant central nervous system disease or injury may also preclude the use of ECMO. Chromosomal abnormalities associated with central nervous system impairment may complicate the assessment of patients and affect predictions about the quality of life. Generally speaking, the presence of Trisomy 21 has not been considered recently to be a contraindication to ECMO after cardiac surgery. However, most families and practitioners believe that the severe limitation in cognitive function and predicted life span associated with Trisomy Crit Care Med 2001 Vol. 29, No. 10 (Suppl.) 13 or 18 would not be consistent with the guideline that the underlying disease or diseases must be reversible to merit consideration for ECMO. Active bleeding from relatively inaccessible locations such as the brain or abdominal structures before initiation of ECMO may also present a relative contraindication, because heparinization would in all likelihood aggravate previously existing disease. Extremes of size and weight may pose limitations on ECMO technology, but those limits expand each year. Unattainable vascular access may deter ECMO cannulation during CPR. Occasionally, a child with congenital heart disease will have had surgery many weeks or months before an in-hospital cardiopulmonary arrest that would otherwise prompt consideration for ECMO as part of the resuscitative maneuvers. However, if the jugular veins or superior vena cava are known to be obstructed from previous interventions and there are anatomical limitations (size or previous procedures) to cannulating through the groin, then the notion of continuing CPR through a prolonged procedure to reopen the sternum through extensive scar tissue may be inadvisable. A ggressive identification and treatment of low car- diac output conditions after cardiac surgery is central to the critical care of children with congenital heart disease. Finally, if progressive myocardial dysfunction characterizes the postoperative course of a patient who is identified as having significant residual anatomical disease, then the temptation to support the child with ECMO must be balanced against the more prudent need to return to the operating room and to address directly the residual anatomical lesion. Identifying Residual Disease. The importance of identifying residual or previously undiagnosed anatomical disease in the postoperative patient with progressive myocardial dysfunction and low cardiac output cannot be underestimated. This is one of the prime responsibilities of those who participate in postoperative management (85, 86). Intracardiac catheters to measure pressure and to sample blood for oxygen saturation will help assess the adequacy of diagnosis and repair. Transthoracic and transesophageal echocardiography are valuable in the postoperative evaluation of the child with low cardiac output. When acoustic windows are limited with echocardiography, the patient may benefit from cardiac catheterization, including physiologic assessment and angiographic imaging. Aggressive diagnostic intervention is a critical component in the assessment of low cardiac output in the postoperative patient. This is especially appealing if suspected residual lesions can be addressed with interventional catheterization techniques. Optimizing Cardiac Output Before and After Mechanical Support. Physicians in the ICU bare the responsibility of anticipating changes in cardiac output after cardiac surgery, excluding residual disease as a causative factor and optimizing physiologic conditions that will achieve optimal cardiac output. The need S227 for mechanical support of the circulation can often be averted by an experienced appreciation of therapeutic modalities to support oxygen delivery short of ECMO (85, 87). However, even if these therapies are inadequate to sustain the patient before invoking ECMO, they must again be thoughtfully applied in the effort to wean the patient from mechanical support as soon as possible after myocardial function has returned and adequate organ perfusion can be guaranteed (Table 1). Institution of Mechanical Circulatory Support. Initiation of ECMO requires the prompt and coordinated efforts of the entire mechanical support team. Algorithms for action to proceed will vary among institutions. In the authors’ experience, the decision to proceed with ECMO is usually made at the bedside by those attending the patient: cardiac surgeon, cardiac intensivist, bedside nurse, and nurse in charge. Cross-trained personnel, such as ECMO specialists who are also respiratory therapy staff, facilitate communication and streamline personnel requirements. As the ECMO specialist is notified, the transfusion service is contacted and a blood prime is planned. The operating room nursing staff are called, and a scrub nurse is made available whenever possible. The precise moment of the procedure start time may vary according to the availability of personnel and necessary components when resuscitation is not impending or under way. Rapid-Deployment ECMO for Resuscitation. When ECMO is utilized during an ongoing resuscitation, the goal is to have a circuit ready in 15 mins and cannulation complete in ⬍30 mins after cardiac arrest. Since 1996, we have utilized an in-hospital rapid deployment team to respond to an emergency need for ECMO cannulation during cardiopulmonary arrest and resuscitation at a variety of locations throughout the hospital (80). These include the ICU, cardiac catheterization laboratory, emergency department, inpatient wards (rarely), and noncardiac operating rooms. Hospital survival of pulseless patients resuscitated with ECMO now exceeds 60%. Obviously, the effectiveness of ECMO as a tool to achieve successful resuscitation of cardiac patients will depend on the nature of the underlying disease and the efficiency of the technique. Typically, we now wait only 5 mins (or one round of medication administration) before determining that return of cardiovascular stability during CPR is unlikely S228 and the ECMO circuit should be primed. A circuit prepared and primed with crystalloid but unused can be maintained in readiness for 24 hrs but will usually be discarded after that time. Delay in cannulation during CPR is rarely the result of prolonged circuit preparation time. A parallel consideration involves the decision process for determining suitability for ECMO. This must occur before cardiac arrest whenever possible. Institutions may adopt general philosophies about rapid resuscitation ECMO for broad categories of patients in the ICU. For example, infants with two ventricles and uncomplicated repair of congenital heart disease who have no other underlying disease may all be candidates for ECMO should they have a sudden, unexpected cardiac arrest in the early postoperative period. In contrast, it may be generally inadvisable to impose ECMO on an older patient with end-stage heart disease or severe neurologic disease who declines or is not otherwise a candidate for transplantation but has an acute decompensation and cardiac arrest. In between these extremes is an area that requires discussion and individualization of care plans that must be accomplished before any anticipated or unanticipated decompensation. Thus, daily patient rounds in the ICU must now incorporate a dialogue among physicians, nurses, family, and support staff that addresses the patient’s suitability for ECMO. The moment after cardiac arrest is not the time to initiate discussions about the appropriateness of invasive, potentially life-prolonging technology. Addressing these issues during rounds and fully discussing the appropriate limitation of technology is an important new responsibility. SUMMARY Aggressive identification and treatment of low cardiac output conditions after cardiac surgery are central to the critical care of children with congenital heart disease. Successful application of these strategies has undoubtedly contributed to the remarkable decline in mortality associated with congenital heart surgery in the past two decades. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. REFERENCES 1. Wernovsky G, Giglia TM, Jonas RA, et al: Course in the intensive care unit after preparatory pulmonary artery banding and aortopulmonary shunt placement for transposition of the great arteries with low left 16. ventricular pressure. Circulation 1992; 86(Suppl II):II-133–II-139 Wernovsky G, Wypij D, Jonas RA, et al: Postoperative course and hemodynamic profile after the arterial switch operation in neonates and infants: A comparison of low-flow cardiopulmonary bypass versus circulatory arrest. Circulation 1995; 92:2226 –2235 Friedman WF, George BL: Treatment of congestive heart failure by altering loading conditions of the heart. J Pediatr 1985; 106:697 Hanley FL, Heinemann MK, Jonas RA, et al: Repair of truncus arteriosus in the neonate. J Thorac Cardiovasc Surg 1993; 105: 1047–1056 Berner M, Jaccard C, Oberhänsli I: Hemodynamic effects of amrinone in children after cardiac surgery. Intensive Care Med 1990; 16:85– 88 Bohn DJ, Poirer CS, Demonds JF: Efficacy of dopamine, dobutamine and epinephrine during emergence from cardiopulmonary bypass in children. Crit Care Med 1980; 8:367 Habib DM, Padbury JF, Anas NG: Dobutamine pharmacokinetics and pharmacodynamics in pediatric intensive care patients. Crit Care Med 1992; 20:601 Berg RA, Donnerstein RL, Padbury JF: Dobutamine infusions in stable, critically ill children: pharmacokinetics and hemodynamic actions. Crit Care Med 1993; 21: 678 – 686 Butterworth JF: Use of amrinone in cardiac surgery patients. J Cardiothorac Vasc Anesth 1993; 7(Suppl):1–7 Rosenzweig EB, Starc TJ, Chen JM, et al: Intravenous arginine-vasopresin in children with vasodilatory shock after cardiac surgery. Circulation 1999; 100:II182–II186 Caspi J, Coles JG, Benson LN, et al: Effects of high plasma epinephrine and Ca2⫹ concentrations on neonatal myocardial function after ischemia. J Thorac Cardiovasc Surg 1993; 105:59 – 67 Caspi J, Coles JG, Benson LN, et al: Agerelated response to epinephrine-induced myocardial stress: A functional and ulstrastructural study. Circulation 1991; 84(Suppl III):III-394 –III-399 Robinson BW, Gelband H, Mas MS: Selective pulmonary and systemic vasodilator effects of amrinone in children: New therapeutic implications. J Am Coll Cardiol 1993; 21: 1461–1465 Chang AC, Atz AM, Wernovsky G, et al: Milrinone: Systemic and pulmonary hemodynamic effects in neonates after cardiac surgery. Crit Care Med 1995; 23:1907–1914 Dupuis JY, Bondy R, Cattran C, et al: Amrinone and dobutamine as primary treatment of low cardiac output syndrome following coronary artery surgery: A comparison of their effects on hemodynamics and outcome. J Cardiothorac Vasc Anesth 1992; 6:542–553 Bailey JM, Miller BE, Lu W, et al: The pharmacokinetics of milrinone in pediatric patients after cardiac surgery. Anesthesiology 1999; 90:1012–1018 Crit Care Med 2001 Vol. 29, No. 10 (Suppl.) 17. Ramamoorthy C, Anderson GD, Williams GD, et al: Pharmacokinetics and side effects of milrinone in infants and children after open heart surgery. Anesth Analg 1998; 86: 283–289 18. Sluysmans T, Styns-Cailteux M, Tremouroux-Wattiez M, et al: Intravenous enalaprilat and oral enalapril in congestive heart failure secondary to ventricular septal defect in infancy. Am J Cardiol 1992; 70:959 –962 19. Hoffman JIE, Rudolph AM, Heymann MA: Pulmonary vascular disease with congenital heart lesions: Pathologic features and causes. Circulation 1981; 64:873– 877 20. Heath D, Edwards JE: The pathology of hypertensive pulmonary vascular disease: A description of six grades of structural changes in the pulmonary arteries with special reference to congenital cardiac septal defects. Circulation 1958; 28:533–547 21. Clapp S, Perry BL, Farooki ZQ, et al: Down’s syndrome, complete atrioventricular canal, and pulmonary vascular obstructive disease. J Thorac Cardiovasc Surg 1990; 100:115–121 22. Del Nido PJ, Williams WG, Villamater J, et al: Changes in pericardial surface pressure during pulmonary hypertensive crises after cardiac surgery. Circulation 1987; 76(Suppl III): III-93–III-96 23. Hickey PR, Hansen DD: Pulmonary hypertension in infants: Postoperative management. In: Annual of Cardiac Surgery. Yacoub M (Ed). London, Current Science, 1989, pp 16 –22 24. Wheller J, George BL, Mulder DG, et al: Diagnosis and management of postoperative pulmonary hypertensive crisis. Circulation 1979; 70:1640 –1644 25. Kirklin JW, Barratt-Boyes BG: Cardiac Surgery. New York, Wiley Medical, 1986, pp 29 – 82 26. Meyrick B, Reid L: Ultrastructural findings in lung biopsy material from children with congenital heart defects. Am J Pathol 1980; 101: 527–542 27. Koul B, Willen H, Sjöberg T, et al: Pulmonary sequelae of prolonged total venoarterial bypass: Evaluation with a new experimental model. Ann Thorac Surg 1991; 51:794 –799 28. Koul B, Wollmer P, Willen H, et al: Venoarterial extracorporeal membrane oxygenation: How safe is it? J Thorac Cardiovasc Surg 1992; 104:579 –584 29. Jones ODH, Shore DF, Rigby ML, et al: The use of tolazoline hydrochloride as a pulmonary vasodilator in potentially fatal episodes of pulmonary vasoconstriction after cardiac surgery in children. Circulation 1981; 64: 134 –139 30. Drummond WH, Gregory GA, Heymann MA, et al: The independent effects of hyperventilation, tolazoline, and dopamine on infants with persistent pulmonary hypertension. J Pediatr 1981; 98:603– 611 31. Bush A, Busst C, Knight WB, et al: Modification of pulmonary hypertension secondary to congenital heart disease by prostacyclin therapy. Am Rev Respir Dis 1987; 136:767–769 Crit Care Med 2001 Vol. 29, No. 10 (Suppl.) 32. Bush A, Busst C, Booth K, et al: Does prostacyclin enhance the selective pulmonary vasodilator effect of oxygen in children with congenital heart disease? Circulation 1986; 74:135–144 33. Furchgott RF: The role of endothelium in the responses of vascular smooth muscle to drugs. Ann Rev Pharmacol Toxicol 1984; 24: 175–197 34. Furchgott RF, Zawadzki JV: The obligatory role of endothelial cells in the relaxation of arterial smooth muscle by acetylcholine. Nature 1980; 288:373–376 35. Palmer RMJ, Ferrige AG, Moncada S: Nitric oxide release accounts for the biologic activity of endothelium-derived relaxing factor. Nature 1987; 327:524 –526 36. Ignarro LJ, Buga GM, Wood KS, et al: Endothelium-derived relaxing factor produced and released from artery and vein is nitric oxide. Proc Natl Acad Sci U S A 1987; 84: 9265–9269 37. Ignarro LJ, Harbison RG, Wood KS, et al: Activation of purified soluble guanylate cyclase by endothelium-derived relaxing factor from intrapulmonary artery and vein: Stimulation by acetylcholine, bradykinin and arachidonic acid. J Pharmacol Exp Ther 1986; 237:893–900 38. Wessel DL, Adatia I, Giglia TM, et al: Use of inhaled nitric oxide and acetylcholine in the evaluation of pulmonary hypertension and endothelial function after cardiopulmonary bypass. Circulation 1993; 88:2128 –2138 39. Beghetti M, Silkoff PE, Caramori M, et al: Decreased exhaled nitric oxide may be a marker of cardiopulmonary bypass-induced injury. Ann Thorac Surg 1998; 66:532–534 40. Haworth SG: Total anomalous pulmonary venous return: Prenatal damage to pulmonary vascular bed and extrapulmonary veins. Br Heart J 1982; 48:513–524 41. Atz AM, Adatia I, Wessel DL: Rebound pulmonary hypertension after inhalation of nitric oxide. Ann Thorac Surg 1996; 62: 1759 –1764 42. Adatia I, Atz AM, Jonas RA, et al: Diagnostic use of inhaled nitric oxide after neonatal cardiac operations. J Thorac Cardiovasc Surg 1996; 112:1403–1405 43. Journois D, Pouard P, Mauriat P, et al: Inhaled nitric oxide as a therapy for pulmonary hypertension after operations for congenital heart defects. J Thorac Cardiovasc Surg 1994; 107:1129 –1135 44. Luciani GB, Chang AC, Starnes VA: Surgical repair of transposition of the great arteries in neonates with persistent pulmonary hypertension. Ann Thorac Surg 1996; 61:800 – 805 45. Russell IA, Zwass MS, Fineman JR, et al: The effects of inhaled nitric oxide on postoperative pulmonary hypertension in infants and children undergoing surgical repair of congenital heart disease. Anesth Analg 1998; 87: 46 –51 46. Dukarm RC, Morin FC, Russell JA, et al: Pulmonary and systemic effects of the phosphodiesterase inhibitor dipyridamole in new- 47. 48. 49. 50. 51. 52. 53. 54. 55. 56. 57. 58. 59. 60. 61. 62. born lambs with persistent pulmonary hypertension. Pediatr Res 1998; 44:831– 837 Yahagi N, Kumon K, Tanigami H: Inhaled nitric oxide for the postoperative management of Fontan-type operations. Ann Thorac Surg 1994; 57:1371–1372 Young JD, Sear JW, Valvini EM: Kinetics of methaemoglobin and serum nitrogen oxide production during inhalation of nitric oxide in volunteers. Br J Anaesth 1996; 76: 652– 656 Rimar S, Gillis CN: Selective pulmonary vasodilation by inhaled nitric oxide is due to hemoglobin inactivation. Circulation 1993; 88:2884 –2887 Hallman M, Bry K, Lappalainen U: A mechanism of nitric oxide-induced surfactant dysfunction. J Appl Physiol 1996; 80:2035–2043 Semigran MJ, Cockrill BA, Kacmarek R, et al: Hemodynamic effects of inhaled nitric oxide in heart failure. J Am Coll Cardiol 1994; 24:982–988 Loh E, Stamler JS, Hare JM, et al: Cardiovascular effects of inhaled nitric oxide in patients with left ventricular dysfunction. Circulation 1994; 90:2780 –2785 Bocchi EA, Bacal F, Auler JOC, et al: Inhaled nitric oxide leading to pulmonary edema in stable severe heart failure. Am J Cardiol 1994; 74:70 –74 Hare JM, Shernan SK, Body SC, et al: Influence of inhaled nitric oxide on systemic flow and ventricular filling pressure in patients receiving mechanical circulatory assistance. Circulation 1997; 95:2250 –2253 Francoise M, Gouyon JB, Mercier JC: Hemodynamic and oxygenation changes induced by the discontinuation of low-dose inhalational nitric oxide in newborn infants. Intensive Care Med 1996; 22:477– 481 Lavoie A, Hall JB, Olson DM, et al: Lifethreatening effects of discontinuing inhaled nitric oxide in severe respiratory failure. Am J Resp Crit Care Med 1996; 153: 1985–1987 Miller OI, Tang SF, Keech A, et al: Rebound pulmonary hypertension on withdrawal from inhaled nitric oxide. Lancet 1995; 346:51–52 Atz AM, Wessel DL: Sildenafil ameliorates effects of inhaled nitric oxide withdrawal. Anesth 1999; 91:307–310 Brutsaert DL, Sys SU, Gillebert TC: Diastolic dysfunction in post-cardiac surgical management. J Cardiothorac Vasc Anesth 1993; 7:18 –20 Brecker SJ, Xiao HB, Mbaissouroum M, et al: Effects of intravenous milrinone on left ventricular function in ischemic and idiopathic dilated cardiomyopathy. Am J Cardiol 1993; 71:203–209 Feneck RO: Intravenous milrinone following cardiac surgery: I. Effects of bolus infusion followed by variable dose maintenance infusion. J Cardiothorac Vasc Anesth 1992; 6:554 –562 Feneck RO: Intravenous milrinone following cardiac surgery: II. Influence of baseline hemodynamics and patient factors on thera- S229 63. 64. 65. 66. 67. 68. 69. 70. 71. 72. peutic response. J Cardiothorac Vasc Anesth 1992; 6:563–567 Remme WJ: Inodilator therapy for heart failure: Early, late, or not at all? Circulation 1993; 87(Suppl IV):IV97–IV107 Vincent JL, Leon M, Berre J, et al: Addition of enoximone to adrenergic agents in the management of severe heart failure. Crit Care Med 1992; 29:1102–1106 Pae WE, Miller CA, Matthews Y: Ventricular assist devices for postcardiotomy cardiogenic shock. J Thorac Cardiovasc Surg 1992; 194: 541 Delius RE, Bove EL, Meliones JN: Use of extracorporeal life support in patients with congenital heart disease. Crit Care Med 1992; 20:1216 –1222 Moler FW, Custer JR, Bartlett RH: Extracorporeal life support for pediatric respiratory failure. Crit Care Med 1992; 20:1112 Duncan BW, Hraska V, Jonas RA: Mechanical circulatory support for pediatric cardiac patients. Circulation 1996; 94:173 Marx M, Salzer-Muhar U, Wimmer M: Extracorporeal life support in pediatric patients with heart failure. Artif Organs 1999; 23: 1001–1005 Bartlett RH, Roloff DW, Custer JR, et al: Extracorporeal life support: The University of Michigan experience. JAMA 2000; 283: 904 –908 Moler FW, Custer JR, Bartlett RH, et al: Extracorporeal life support for severe pediatric respiratory failure: An updated experience 1991-1993. J Pediatr 1994; 124:875– 880 Revenis ME, Glass P, Short BL: Mortality and morbidity rates among lower birth weight S230 73. 74. 75. 76. 77. 78. 79. infants (2000 to 2500 grams) treated with extracorporeal membrane oxygenation. J Pediatr 1992; 121:452– 458 Moler FW, Palmisano JM, Custer JR, et al: Alveolar-arterial oxygen gradients before extracorporeal life support for severe pediatric respiratory failure: Improved outcome for extracorporeal life support-managed patients? Crit Care Med 1994; 22:620 – 625 Meyer DM, Jessen ME, Extracorporeal Life Support Organization: Results of extracorporeal membrane oxygenation in neonates with sepsis. J Thorac Cardiovasc Surg 1995; 109: 419 – 427 UK Collaborative ECMO Trial Group: UK collaborative randomised trial of neonatal extracorporeal membrane oxygenation. Lancet 1996; 348:75– 82 Lai WW, Lipshultz SE, Easley KA, et al: Prevalence of congenital cardiovascular malformations in children of human immunodeficiency virus-infected women: The prospective P2C2 HIV multicenter study. J Am Coll Cardiol 1998; 32:1749 –1955 Kanto WP Jr: A decade of experience with neonatal extracorporeal membrane oxygenation. J Pediatr 1994; 124:335–347 Kulik TJ, Moler FW, Palmisano JM, et al: Outcome-associated factors in pediatric patients treated with extracorporeal membrane oxygenator after cardiac surgery. Circulation 1996; 94:II63–II68 Dalton HJ, Siewers RD, Fuhrman BP, et al: Extracorporeal membrane oxygenation for cardiac rescue in children with severe myocardial dysfunction. Crit Care Med 1993; 21: 1020 –1028 80. Duncan BW, Ibrahim AE, Hraska V, et al: Use of rapid-deployment extracorporeal membrane oxygenation for the resuscitation of pediatric patients with heart disease after cardiac arrest. J Thorac Cardiovasc Surg 1998; 116:305–311 81. Lee KJ, McCrindle BW, Bohn DJ, et al: Clinical outcomes of acute myocarditis in childhood. Heart 1999; 82:226 –233 82. Ibrahim AE, Duncan BW, Blume ED, et al: Long-term follow-up of pediatric cardiac patients requiring mechanical circulatory support. Ann Thorac Surg 2000; 69: 186 –192 83. Duncan BW, Hraska V, Jonas RA, et al: Mechanical circulatory support in children with cardiac disease. J Thorac Cardiovasc Surg 1999; 117:529 –542 84. Langley SM, Sheppard SV, Tsang VT, et al: When is extracorporeal life support wothwhile following repair of congenital heart disease in children? Eur J Cardiothorac Surg 1998; 13:520 –525 85. Wernovsky G, Chang AC, Wessel DL: Intensive Care. In: Heart Disease in Infants, Children, and Adolescents—Including the Fetus and Young Adult. Emmanouilides GC, Riemenschneider TA, Allen HD, et al (Eds). Baltimore, Williams & Wilkins, 2000, pp 398– 439 86. Chang AC, Hanley FL, Wernovsky G, et al: Pediatric Cardiac Intensive Care. Baltimore, Williams & Wilkins, 1998 87. Goldman AP, Delius RE, Deanfield JE, et al: Nitric oxide might reduce the need for extracorporeal support in children with crititcal postoperative pulmonary hypertension. Ann Thorac Surg 1996; 62:750 –755 Crit Care Med 2001 Vol. 29, No. 10 (Suppl.)