* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Lab 8
Ascending cholangitis wikipedia , lookup
Plasmodium falciparum wikipedia , lookup
Marine microorganism wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
Disinfectant wikipedia , lookup
Neonatal infection wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Human microbiota wikipedia , lookup
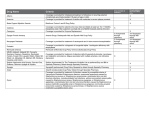
Lab 8 Identification of Staphylococci and Streptococci In this lab we will examine methods for identifying unknown pathogenic cultures. Organisms from the genus Staphylococcus and Streptococcus cause a number of diseases. Sometimes both are capable of causing the same disease. It is important to distinguish which organism you are dealing with, as the most effective treatment may vary depending on which one is causing the infection. Exercise 1: Catalase Test The Catalase test is used to differentiate between Staphylococci and Streptococci. This simple, and immediate, test identifies organisms that possess the enzyme catalase, which breaks down hydrogen peroxide into water and gaseous oxygen. When hydrogen peroxide is added to Staphylococci, which is catalase-positive, bubble form. Streptococci do not form bubbles since they do not have catalase. Note that this is just one way that you can differentiate staphylococci from streptococci. Another simple way that you have already learned is by Gram staining. Both are Gram-positive cocci, but staphylococci form clusters while streptococci are found in chains. Objective: To differentiate between Staphylococcus and Streptococcus by identifying the presence of the enzyme catalase. Materials: Staphylococcus aureus slant Streptococcus pyogenes slant Clean microscope slides Hydrogen peroxide Pipet Sharpie Procedure: 1. Label a microscope slide with the name of the organism. You can test both organisms on one slide by putting one culture on each end of the slide 2. Place a drop of hydrogen peroxide on each side of the slide 3. Aseptically transfer a small amount of bacteria to one of the hydrogen peroxide drops 4. Watch for the production of bubbles. This will happen very quickly 5. Aseptically transfer a small amount of the second bacteria to the other drop of hydrogen peroxide 6. Watch for the production of bubbles Results: 1. What does the catalase test differentiate? 2. How is the presence of catalase detected? 3. Give the formula for this reaction. 4. Which genus is catalase positive? 5. What are some other ways you can differentiate Staphylococcus from Steptococcus? Tests to determine the species of Staphylococci There are three major species of pathogenic Staphylococci; Staphylococcus aureus, Staphylococcus saprophyticus, and Staphylococcus epidermidis. While S. aureus is the main cause of infection among the Staphylococci, S. saprophyticus and S. epidermidis are the source of several infections of clinical importance. S. aureus infections include gastroenteritis, toxic shock syndrome (TSS), pneumonia, meningitis, osteomylelitis, bacteremia, urinary tract infections (UTI). S. saprophyticus is one of the leading causes of UTI’s in sexually active women. S. epidermidis is associated with infections of catheters, IV lines, and prosthetic devices. We will be looking at a number of ways of differentiating between these organisms in this lab. Exercise 2: Coagulase Coagulase is an enzyme used by S. aureus to cause the formation of blood plasma clots around themselves. This clots acts as a mechanism of evading the hosts’ immune defense. Because S. aureus produces coagulase and the other species of staphylococcus do not, inoculation of a tube containing rabbit plasma will give a positive indication of S. aureus. Objective: To identify a Staphylococcus aureus by identifying the presence of the enzyme coagulase. Materials: Staphylococcus aureus broth Staphylococcus epidermidis broth 2 tubes of rabbit plasma per group of 4 students Procedure: 1. Label the rabbit plasma tubes 2. Inoculate rabbit plasma with a heavy amount of each Staphylococcus 3. Place in your labs incubation bin for incubation at 37°C overnight Results: 1. What is coagulase? 2. What benefit might a bacterium gain by forming a plasma clot around itself? 3. What species of Staphylococcus produces coagulase? 4. What does a positive test for coagulase look like? Exercise 3: Mannitol Salt Agar (MSA) MSA contains mannitol (carbohydrate), 7.5% sodium chloride (salt), and phenol red (pH indicator). Because most bacteria cannot survive in a high salt environment, this media is selective for staphylococci. While all staphylococci can grow on this media, only the pathogenic forms (S. aureus) can ferment mannitol. Fermentation of mannitol produces acid, which causes the pH indicator phenol red to turn yellow (note: phenol red is yellow below pH 6.8, red at pH 7.4 to 8.4, and pink above pH 8.4) Objective: To determine if a bacterium is from the genus Staphylococcus (Selective property). To determine if a Staphylococcus is the mannitol fermenting Staphylococcus aureus (Differential property). Materials: Staphylococcus aureus broth Staphyloccus epidermidis broth Escherichia coli broth One MSA plate per group of 4 Inoculating loop Bunsen burner Procedure: 1. With a marker, divide the plate in thirds and thoroughly label the bottom of the plate 2. Inoculate one-third with a straight-line streak of Staphylococcus aureus, one-third with a straight-line streak of Staphylococcus epidermidis, and one-third with a straight-line streak of Escherichia coli. 3. Place upside down in your lab sections incubation bin 4. Incubate at 37°C overnight Results: 1. What makes MSA a selective media? 2. What does MSA select for? 3. How is a positive result for the selective property determined? 4. What makes MSA a differential media? 5. What does MSA differentiate between? 6. How is a positive result for the differential property determined? 7. Which bacteria did MSA select for? 8. Which bacteria fermented mannitol? Exercise 4: Novobiocin Sensitivity Test The novobiocin sensitivity test uses paper disks impregnated with the antibiotic novobiocin. A small amount of broth is spread over a portion of the plate and the novobiocin disk is place on this area. The antibiotic diffuses a known distance into the media. Bacteria that are susceptible to the antibiotic will not grow well, leaving an area known as a zone of inhibition around the antibiotic disk. Those that are resistant grow despite the presence of the antibiotic. S. saprophyticus is resistant to novobiocin, while S. aureus and S. epidermidis are susceptible. Objective: To differentiate Staphylococcus saprophyticus from the other Staphylococci based on its resistance to the antibiotic novobiocin. Materials: Staphylococcus aureus broth Staphylococcus epidermidis broth Staphylococcus saprophyticus broth 3 Sterile cotton swab 1 Blood agar plate per group of 4 Novobiocin disks Forceps Procedure: 1. Label and divide the blood agar plate in thirds with a sharpie 2. Dip the sterile cotton swab into one of the broths 3. Spread the culture in the appropriate section to create a square 4. Using the forceps, gently press a novobiocin disk in the center of your bacterial spread 5. Repeat steps 2 through 4 for the other two broth cultures 6. Place your plate upside down in your labs incubation bin to be incubated at 37°C overnight Results: 1. What is novobiocin? 2. Which species of Staphylococcus is resistant to novobiocin? 3. Should you see growth of this species in close proximity to the novobiocin disk? Why or why not? 4. Should you see growth of the susceptible species in close proximity to the novobiocin disk? Why or why not? Tests to determine the species of Streptococci We will be using several different organisms in this section; Streptococcus pyogenes, Streptococcus agalactiae, Enterococcus faecalis (note that E. faecalis was previously named Streptococcus faecalis) and Streptococcus pneumoniae. Streptococci can be classified in a couple of ways. One way is by the type of hemolysin, if any, it produces. Beta-hemolytic streptococci completely hydrolyze red blood cells. Alpha-hemolytic streptococci partially hydrolyze red blood cells. Non-hemolytic, or sometimes called gamma-hemolytic, are not hemolytic at all and do not affect the red blood cells. Another way to classify streptococci is based on a carbohydrate antigen present on the bacterial cell wall called the Lancefield antigen. Today’s organisms come from groups A (Streptococcus pyogenes), B (Streptococcus agalactiae), and D (Enterococcus faecalis). Streptococcus pneumoniae does not have surface carbohydrate antigens that fall into one group. Like the staphylococci, streptococci are the cause of many infections. Among the infections that Streptococcus pyogenes causes are cellulitis, pharyngitis, necrotizing fasciitis, scarlet fever, TSS, rheumatic fever, and post-streptococcal glomerulonephritis. Streptococcus agalactiae is responsible for several infections in newborns. S. agalactiae in the birth canal may be transferred to the fetus during a vaginal delivery and cause meningitis, pneumonia, or sepsis. Enterococcus faecalis is responsible for cases of UTI, biliary tract infections, and subacute bacterial endocarditis. Streptococcus pneumoniae causes pneumonia, otitis media, and meningitis. Exercise 5: Hemolysis Streptococci may produce an enzyme called hemolysin, which destroys or partially destroys red blood cells. We will use a blood agar plate to determine the type of hemolysin produced by the Streptococci. Both Streptococcus pyogenes and Streptococcus agalactiae are beta-hemolytic, which means they completely destroy red blood cells. Inoculation of a blood agar plate with either of these organisms will result in a clearing around the colonies. Enterococcus faecalis is either alpha- or gammahemolytic, depending on the strain. Alpha-hemolysis results in partial breakdown of the red blood cells and appears as a green coloration around the colonies due to a hemoglobin metabolite of the unlysed RBC’s. Non-hemolysis (gamma-hemolysis) will not cause a color change in the media, just growth of colonies. Streptococcus pneumoniae is alpha-hemolytic. Objective: To determine the type of hemolysis performed by different species of Streptococcus. Materials: Streptococcus pyogenes broth Streptococcus mitis broth Enterococcus faecalis broth 1 Blood agar plate per group of 4 Procedure: 1. Label and divide the blood agar plate in thirds with a sharpie. 2. Straight-line streak each section with the appropriate organism 3. Put your plate upside down in your labs incubation bin for incubation at 37°C overnight Results: 1. What appearance does an alpha-hemolytic bacterium produce? 2. What appearance does a gamma-hemolytic bacterium produce? 3. What species of Streptococcus are beta-hemolytic? Exercise 6: Bacitracin Sensitivity In the bacitracin sensitivity test, a paper disk impregnated with the antibiotic bacitracin is placed on a blood agar plate in an area in which you have spread a bacterial culture. If an organism is susceptible to bacitracin, a clear zone will form around the disc. Organisms resistant to bacitracin will grow around the disc. The test is useful in differentiating the beta-hemolytic group A strep (Streptococcus pyogenes is bacitracin susceptible) from other beta-hemolytic streptococci. Objective: To identify Streptococcus pyogenes based on its susceptibility to the antibiotic bacitracin. Materials: Streptococcus pyogene broth Streptococcus agalactiae broth 1 Blood agar plate per group of 4 2 Sterile cotton swabs Bacitracin discs Forceps Procedure: 1. Label and divide the blood agar plate in half with a sharpie. 2. Dip the sterile cotton swab into one of the broths 3. Spread the culture in the appropriate section to create a square 4. Using the forceps, gently press a bacitracin disk in the center of your bacterial spread 5. Repeat steps 2 through 4 for the other broth culture 6. Place your plate upside down in your labs incubation bin to be incubated at 37°C overnight Results: 1. What is bacitracin? 2. Which species of Streptococcus is susceptible to bacitracin? 3. Should you see growth of this species in close proximity to the bacitracin disk? Why or why not? 4. Should you see growth of the resistant species in close proximity to the bacitracin disk? Why or why not? Exercise 7: Bile Esculin Test Bile esculin agar is a media used to detect Group D streptococci and enterococci. This media contains bile, which inhibits the growth of organisms except Group D streptococci and enterococci. These organisms can hydrolyze esculin into glucose and esculetin. The glucose is used for energy metabolism and the esculetin reacts with iron salts in the media to form a black precipitate. This dark coloration indicates that you have a Group D strep or enterococci. Objective: To identify Enterococcus faecalis based on its ability to grow in the presence of bile and utilize esculetin as an energy source. Materials: Enterococcus faecalis broth Streptococcus pyogenes broth 1 bile esculin plate per group of 4 Procedure: 1. Label and divide the bile esculin agar plate in half with a sharpie. 2. Straight-line streak the surface of each half with the appropriate organism. 3. Put in your labs incubation rack to be incubated at 37°C overnight Results: 1. What makes this a selective media? 2. Explain the differential property of this media? 3. What types of bacteria will grow on the bile esculin media? 4. What does a positive test look like? These charts outline the “expected” results for each test. Make sure you know the expected results for each organism on each test for your practical (i.e. memorize these charts!) Catalase Coagulase DNase MSA Novobiocin S. aureus + + + beta susceptible S. saprophyticus + resistant Catalase Hemolysis S. pyogenes beta S. agalactiae beta S. Alpha Bacitracin Bile esculin sensitive - resistant - resistant - S. epidermidis + susceptible E. faecalis Alpha or gamma resistant +