* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Gram Positive Bacteria - UAB School of Optometry
Germ theory of disease wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Human microbiota wikipedia , lookup
Methicillin-resistant Staphylococcus aureus wikipedia , lookup
Molecular mimicry wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Neonatal infection wikipedia , lookup
Urinary tract infection wikipedia , lookup
Triclocarban wikipedia , lookup
Anaerobic infection wikipedia , lookup
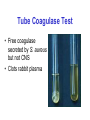
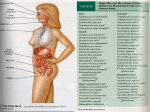
Gram Positive Cocci Dental Optometry Microbiology Ken B. Waites, M.D., F(AAM) Objectives • To review and discuss: • • • • • microbiological characteristics epidemiology virulence factors associated diseases laboratory detection of clinically important gram-positive cocci and grampositive bacilli. • Organisms to be discussed include: – – – – – – Staphylococcus Streptococcus Enterococcus Listeria Corynebacterium Bacillus Staphylococcus • Most important genus in Family Micrococcaceae • Other genera – Stomatococcus – Micrococcus Habitat • S. aureus – anterior nares 50-75% healthy people – skin & mucous membranes – hospital environment • S. epidermidis & others – resident skin flora, gut, upper respiratory tract • S. saprophyticus – Urinary tract in young women Lab Characteristics • Gram-positive cocci (1 m) in clusters • Culture - Aerobic • S. aureus is hemolytic • Coagulase • Catalase • Mannitol fermentation S. aureus blood agar mannitol salt agar Catalase Test for Distinguishing Staphylococci from Streptococci H2O2 catalase Strep. Negative O2 + H2O Bubbles Staph. positive Tube Coagulase Test • Free coagulase secreted by S. aureus but not CNS • Clots rabbit plasma Cell Wall of S. aureus Antigenic Structures & Virulence Factors of S. aureus • Cell wall peptidoglycan – – – – – elicits production of IL-1 and opsonic antibody PMN chemotaxis “pyogenic” induces sepsis activates complement teichoic acid binds fibronectin on host cells • Protein A - binds Fc of IgG • Capsule (some strains) antiphagocytic S. aureus Soluble Virulence Factors • • • • • • • • Catalase - reduce phagocyte killing - remove H2O2 Coagulase - clots plasma (free & bound) Hyaluronidase - destroys connective tissue Beta lactamase - destroys beta lactam drugs Altered Penicillin binding proteins (PBP2’) Fibrinolysin Lipases Nucleases S. aureus Soluble Virulence Factors • Cytotoxins & leukocidins – lyse white blood cells (Panton-Valentine) – release lysosomal enzymes damage tissue • Exfoliatin – interrupts intercellular skin junctions – “Scalded Skin Syndrome” • Toxic Shock Toxin – stimulates T cells cytokines, – endothelial damage rash – “Toxic Shock Syndrome” • Enterotoxins – stimulate vomiting by interaction with GI neural receptors (food poisoning) S. aureus Diseases Skin and soft tissue infections Furuncles Carbuncles Wound infections Cellulitis Impetigo Bacteremia Endocarditis CNS Infections Brain abscess Meningitis - rare Epidural abscess Impetigo S. aureus Diseases Pulmonary Infections embolic aspiration Musculoskeletal osteomyelitis septic arthritis Genitourinary Tract renal carbuncle lower UTI Toxin mediated diseases • scalded skin syndrome • food poisoning • toxic shock disease Toxic shock Scalded skin Treatment of Staph. Infections • Increase in oxacillin-resistant organisms that are resistant to most other antibiotics except vancomycin (MRSA) • Nosocomial infections • Recent emergence of virulent communityacquired MRSA in skin & soft tissue infection • First high-level vancomycin-resistant S. aureus reported July 2002 contains vanA gene from Enterococcus Coagulase negative staphylococci • Opportunistic infections – bacteremias – endocarditis – neutropenic patients – Neonates – UTIs (S. saprophyticus) Staphylococcus epidermidis on sheep blood agar White non-hemolytic colonies • Polysaccharide “slime” – protects bacteria – mediates attachment to catheters, etc. Streptococcaceae • Streptococcus • Enterococcus Staph Strep Gram stain of staph (clusters) and strep (chains) Streptococcus Classification • Hemolysis – beta – alpha – gamma • Lancefield Groups – (A-T- hemolytic) – group-specific cell wall polysaccharide • Species – phenotypic biochemical reactions Hemolytic Reactions Streptococcus Habitat • Skin, mucous membranes, respiratory tract and Gl/GU tracts, depending on species • 20% of children may carry GAS in their pharynx during winter months. • S. pneumoniae is commonly isolated from the respiratory tract of asymptomatic carriers. • Enterococci in gut flora are are important pathogens in hospitals where they are selected by high antibiotic usage. • Organisms spread by droplets, direct contact and fomites. Lab Characteristics • Morphology and Gram stain – Gram-pos. cocci 0.7 - 0.9 m – pairs or chains • Catalase-negative • Most grow on sheep blood agar • Aerobic or anaerobic • Enhanced by CO2 • Antigenic grouping • Biochemical identification S. pyogenes in blood S. pneumoniae in sputum Antigenic Structure & Virulence Factors of S. pyogenes • Hyaluronic acid capsule - antiphagocytic • Hyaluronidase - tissue penetration • Group specific cell wall antigen distinguishes from B,C,D,F,G, etc. • Beta hemolytic Antigenic Structure & Virulence Factors of S. pyogenes • M Protein – Virulence factor present on pilus with teichoic acid – Organisms lacking it are readily opsonized and phagocytized – Binds fibrinogen, fibrin & degradation products forming dense coating on the organism's surface, blocking complement – Antibody against M protein is an important protective mechanism, but repeated infections with strains possessing one of over 80 different serotypes can occur – Autoantibody target-Acute Rheumatic Fever Antigenic Structure & Virulence Factors of S. pyogenes • Erythrogenic Toxin “Scarlet Fever” • Streptokinases – transform plasminogen to plasmin – digest fibrin • DNAase – depolymerizes DNA antibody used to follow pyoderma • Hemolysins “Streptolysins” – Important immunogens – Antibody against streptolysin O used to follow course of pyoderma – Streptolysin S - hemolysis Strep. cellulitis Antigenic Structure & Virulence Factors of S. pyogenes • Protein F - facilitates attachment by binding fibronectin • Protein G - binds Fc portion of antibody • Diphosphopyridine nucleotidase (DPNase) – enzyme kills WBCs • C5a peptidase Erysipelas S. agalactiae “Group B” • Pathogen of newborns & older debilitated adults • Antibody against typespecific capsular antigen is protective • CAMP Test - interaction of CAMP factor (sphingomyelinase) with hemolysin of S. aureus to potentiate hemolytic activity • Hippurate hydrolysis S. aureus GBS Diseases Due to Hemolytic Streptococci Group Species Disease A S. pyogenes Pharyngitis, impetigo, cellulitis, erysipelas, scarlet fever, necrotizing faciitis, rheumatic fever, glomerulonephritis S. agalactiae Neonatal sepsis, pneumonia, meningitis, OB/GYN infections, Bacteremia, UTI B C S. equi, S. dysgalactiae, Bacteremia, & others pneumonia, endocarditis, abscesses, pharyngitis, wound infections D S. bovis Endocarditis, bacteremia in cancer patients F S .anginosus Cervicofacial abscesses, bacteremia, osteomyelitis S. pneumoniae • Asymptomatic carriage • Colonization precedes disease • Most common cause of: – community acquired pneumonia (bacteremia) – otitis media (children) – meningitis • Species-specific C polysaccharide • No Lancefield antigen • 90 capsular serotypes • Alpha hemolytic • Bile soluble, optochin susceptible • Often require CO2 for growth Optochin test S. pneumoniae Virulence Factors • • • • Antiphagocytic capsule – immunogen PspA: inhibits opsonization Autolysin – release cell components Pneumolysin • • • • • • • • • Cytotoxic – inhibit cilia, wbcs lyses RBCs activates classic complement path. stimulates cytokines tissue damage & purulent inflammation sputum - pneumonia Hydrogen peroxide - tissue damage Surface protein adhesins Neuraminidase IgA protease Peptidoglycan – activate alternate complement – cytokine release • Transformation– antibiotic resistance • Intracellular invasion Capsule Quellung Reaction Fatal Pneumococcal Meningitis Pneumococcal Vaccine • 23 valent polysaccharide vaccine - adults • 7 valent conjugate vaccine - children Viridans streptococci • Most human strains are commensals of the oral cavity & upper respiratory tract • Alpha hemolysis • Do not have Lancefield group antigens • Differentiate species biochemically • Usually of low pathogenicity • Important causes of endocarditis • Dental caries (S. mutans) dextran from glucose Enterococcus • • • • At least 12 species Usually non-hemolytic E. faecalis most common Distinguish from streptococci by: – esculin hydrolysis – growth in 6.5% NaCl – PYR hydrolysis (Group A strep. are +) • • • • • Enteric flora Opportunist - nosocomial pathogen Intrinsic antimicrobial resistance E. faecium - vancomycin-resistance Abscesses, urinary tract, endocarditis, abdominal/pelvic, bacteremia, wound infections