* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Sickle Cell Anemia (SCA) - Clayton State University
Survey
Document related concepts
Transcript
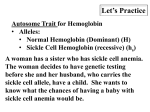
Sickle Cell Anemia Jenny Pham Protein Structure & Function Spring 2015 Outline I. Normal Adult Hemoglobin (Hb A) a. Function: Deoxygenated v. Oxygenated II. Mutation in Hb A a. Sickle Cell Hemoglobin (Hb S) III. Sickle Cell Anemia a. Background b. Medical/Biological Nature c. Biochemical Nature (Pathophysiology) d. Treatment Introduction Hemoglobin (Hb A) • Function: Transport oxygen and other gases throughout the body via erythrocytes (red blood cells, or RBCs). • Quaternary Structure: 4 Chains (Domains) – 2 α + 2 β Chains Each chain is comprised of 8 α helices connected by 7 loop regions. • No β strands. Heme molecule bound within pocket created by the α helices of each chain. PDB: 1HHO Method: X-Ray Diffraction Resolution: 2.10 Å Ligand: Heme Group • Heterocyclic Ring Structure: Protoporphyrin IX – 4 Pyrroles Surrounding the Fe2+ Ion • Location of O2 binding Hemoglobin Binding to Oxygen Close Up of Oxygen Binding to the Heme Group in Hemoglobin • Deoxygenated Hemoglobin (Left: 2HHB) • Oxygenated Hemoglobin (Right: 1HHO) Mutation: Hemoglobin S (Hb S) • Results from a point mutation of a thymine to a adenine at the 17th nucleotide in the βglobin gene on chromosome 11. – Causing for the 6th amino acid on the β- chains to change from glutamic acid (red) to valine (green). Hb A vs. Hb S Normal Adult Hemoglobin PDB: 2HHB Method: X-Ray Diffraction Resolution: 1.74 Å Hemoglobin S (Sickle) PDB: 2HBS Method: X-Ray Diffraction Resolution: 2.05 Å • Point mutation responsible for the distortion of normal RBCs into sickle-shaped RBCs. – Normal RBCs: pliable, biconcave discs – Sickled RBCs: stiff, sticky • Deoxygenated Hb S causes for hemoglobin polymers to form, disrupting the cytoskeleton of the RBC that forms protrusions (sickle shape). – Interruption of the membrane attachment to the cytoskeleton leads to the exposure of negatively charged glycolipids, resulting in the blockage of blood circulation. Sickle Cell Anemia (SCA) • It’s an autosomal recessive disorder that is characterized by the homozygous inheritance of the βs allele (HbSS). – Must inherit sickle cell trait from both parents. • Most common type of sickle cell disease. Prevalence for SCA • Most Common Genetic Disorder in US – Affecting 70,000 – 100,000 Individuals – Primarily African Americans = 1 in 500 • Common in People from Africa, South and Central America, Caribbean Islands, Mediterranean Islands, India, and Saudi Arabia – Distribution of HbS allele correlated to the distribution of malaria – parasites that thrive in normal RBCs cannot survive in sickled RBCs. Medical/Biological Nature of SCA • SCA is present at birth but does not manifest until 4 months after birth. • Early diagnosis at birth can lengthen lifespan with blood test. – Using amniotic fluid or placenta tissue can be used to diagnose SCA before birth. • Signs & Symptoms Vary – can range from mild to severe – Linked to Anemia and Pain • Numerous Complications – Examples: Increased Risk of Infections, Splenic Crisis, Acute Chest Syndrome, Multiple Organ Failure Biochemical Nature of SCA Common Treatments • Hydroxycarbamide (Hydroxyurea) • Blood Transfusions • Allogeneic HSCT – only cure for SCA Emerging Treatments References 1. Rees, D., Williams, T., & Gladwin, M. (2010). Sickle-cell disease. The Lancet, 376(9757), 2018-2031. 2. Gong, L., Parikh, S., Rosenthal, P., & Greenhouse, B. (2013). Biochemical and immunological mechanisms by which sickle cell trait protects against malaria. Malaria Journal, 12(317). 3. Bender MA, Douthitt Seibel G. Sickle Cell Disease. 2003 Sep 15 [Updated 2014 Oct 23]. In: Pagon RA, Adam MP, Ardinger HH, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2015. 4. Ashley-Koch, A., Yang, Q., & Olney, R. S. (2000). Sickle Hemoglobin (Hb S) Allele and Sickle Cell Disease: A HuGE Review. American Journal of Epidemiology, 151(9), 839-845. 5. Frenette, P., & Atweh, G. (2007). Sickle Cell Disease: Old Discoveries, New Concepts, and Future Promise. Journal of Clinical Investigation, 117(4), 850-858. 6. Chakravorty, S., & Williams, T. (2014). Sickle cell disease: A neglected chronic disease of increasing global health importance. Archives of Disease in Childhood, 100(1), 48-53. 7. George, S., Mitchell, E., Mitchell, N., Eason, T., Fuh, B., & von der Embse, N. (2014). Sickle Cell Disease. Science Scope, 38(4), 33-38. 8. Harrington, D., Adachi, K., & Royer, W. (1997). The high resolution crystal structure of deoxyhemoglobin S. Journal of Molecular Biology, 272(3), 398-407. 9. Dutta, S., & Goodsell, D. (2003). Hemoglobin. Retrieved March 1, 2015, from http://www.rcsb.org/pdb/101/motm.do?momID=41 10. The high resolution crystal structure of deoxyhemoglobin S. (1997). Retrieved March 1, 2015, from http://www.rcsb.org/pdb/explore/explore.do?structureId=2hbs 11. The crystal structure of human deoxyhaemoglobin at 1.74 A resolution. (1984). Retrieved March 1, 2015, from http://www.rcsb.org/pdb/explore.do?structureId=2HHB 12. Structure of human oxyhaemoglobin at 2.1 A resolution. (1983). Retrieved March 1, 2015, from http://www.rcsb.org/pdb/explore/explore.do?structureId=1hho