* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiac Arrest
Survey
Document related concepts
History of invasive and interventional cardiology wikipedia , lookup
Electrocardiography wikipedia , lookup
Myocardial infarction wikipedia , lookup
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Jatene procedure wikipedia , lookup
Transcript
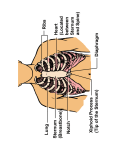
ACLS Notes CPR Physiology: CPR produces 10-20% of CO, up to BP of 100mmHg Systolic Changes in thoracic AP diameter keep blood moving (not heart compression) Compression/Decompression (toilet plunger theory) more effective Myocardial Perfusion: Aortic root pressure: coronary a.’s hi pressure is good (ie Adr) RAP: coronary sinus empties into RA, low pressure is good) Tone of coronary a.’s: dilated/constricted, fixed stenosis/dilatable Ventric wall tension: coronary capillaries constrict during systole, ischaemia ventric wall tension Brain Death due to 02 O2 Stores: Lungs = 400ml Hb = 8-900ml Total = 12-1300ml O2 Consumption 250ml/min (140ml/min/m2) 1200/250 = 4-5 mins If you can CIRCULATE the O2 in body you’ll prolong survival Neuronal damage: Hypoxia – anaerobic metab – CO2 + H+ buildup – cerebral/lactic acidosis – neuronal damage due to cell memb damage & influx of H20 – cell swelling - ICP - cerebral perfusion ONLY STOP CPR FOR: Defibrillation Intubation Recovery Checks To remove patient/self from danger Cardiac Arrest Definition of Cardiac Arrest: Life threatening sudden loss of cardiac output Causes of Cardiac Arrest: * Ventricular Arrhythmias: VF, VT or Asystole * In Children: BRADYCARDIA WITH OR WITHOUT PULSE * EMD/PEA Signs/Symptoms: UNCONSCIOUS + NO PULSE Often assoc. with resp arrest (ie cardiac arrest 2o to resp arrest) Sudden unconsciousness Absent major pulse/BP/Heart sounds Absence of breathing, or agonal breathing Pallor or cyanosis (late sign) Dilated pupils after 45secs Management of Cardiac Arrest: FIRST STEP: Check for danger: water on floor, electrical, body fluids NOTE TIME CALL FOR HELP PUT ON GLOVES If Unconscious: Left lat position: protects airway, stomach on left PREGNANT: gets them off IVC Clear Airway: suction/finger Head tilt, jaw support Turn face slightly down, mouth open Check Breathing: if breathing – leave in left lat position, apply O2, observe ABC Position: on firm flat surface (remember backboard) Exposure: expose abdomen & chest Conscious state: Shake, call name, tactile stimulus Airway: visual inspection, leave well-fitting dentures in, otherwise remove, insert Guedels’s airway, connect bag/mask to high flow O2 Respiration: look listen feel Circulation: check major pulse (carotid/femoral) for at least 5 secs Simultaneously Think about establishing a precipitating cause What happened to Pt just prior to arrest, ie drugs, in previous hour,…etc What pre-existing illnesses do they have? When were they last seen alive? Then: Connect O2 at highest flow (Bag/Mask initially) Cease all IV infusions Connect N.Saline or Dextrose line Prepare drugs: Adr/Atropine/Lignocaine Airway Management Clear airway (as described) Head tilt, jaw thrust, “sniffing” position Guedels/Nasopharyngeal airways Guedels: unconscious patients Size: corner of mouth to earlobe (size 2 in most adults) Use tongue depressor to assist if difficult (esp children) Nasopharyngeal: alternative to oropharyngeal Not in suspected fracture B.O.S. Size: patients little finger (small-med=6-7, med/large=7-9) Lubricate, right nostril, flange medially, rotate Breathing Management Give 5 breaths in 10 secs, (to restore FRC) then reassess breathing Mouth to Mouth (infection, poisoning risks) Mouth to Mask (can connect O2 to mask) Bag/Mask (alone = 21% O2, + O2 supply at 10-12l/min = 50% O2, + reservoir bag + O2 at 12-15l/min = 90-100% O2) EAR: Head tilt Jaw support Adult Yes Yes Child (1-8 yr) Infant (0-1yr) Slight Yes No Yes Assessment of effectiveness: Resistance felt Chest rise/fall Feel/hear air escape Colour improvement Complications: Gastric distension/rupture Regurgitation/aspiration Hyperventilation – pneumothorax No of Breaths 1 every 4secs 1 every 3secs 1 every 3secs Cycles 20/min Breath Strength Full (chest rise) Gentle 20/min Cheek puffs 15/min C-spine trauma Broken teeth Ineffective If patient vomits: StopCPR/EAR turn on left side, clear airway Recheck airway patency/position of hands on sternum Insert NGT (head forward) to empty stomach Circulation Management ie No pulse after 5-10 secs palpation: Infants: carotid not palable – use brachial Pregnant: PUT PT FLAT WITH PELVIS IN LEFT LAT TILT CPR Hand Position: Lower half sternum START GENTLY CPR In Children Indication = BRADYCARDIA + other Syx/Signs of arrest (ie unconscious, apnoea, pallor, floppy, in extremis) Infant (1month-1year) – PR < 80 Young Child (1-8 years) – PR < 60 OlderChild (9-14 years) – PR < 40 Site Use Depth Compressions: Breaths 1 operator Compressions: Breaths 2 operator Effective pulse rate Adult Lower ½ sternum 2 hands 4-5 cm 15:2 in 15 secs 4 cycles/min Young Child Lower ½ sternum Heel of 1 hand 3cm 5:1 in 5 secs 12 cycles/min Infant Lower ½ sternum 2 finger 2cm 5:1 in 5 secs 12 cycles/min 5:1 in 5 secs 12 cycles/min 5:1 in 5 secs 12 cycles/min 5:1 in 5 secs 12 cycles/min 60-80 80-100 80-100 Effectiveness: Pulse/ECG artefact coincides with compression Colour improvement Patient wakes up! Complications: Bruising Fracture rib, xiphoid, sternum, flail segment Lacerated liver, spleen, lung – pneumothorax Ineffective Assess for ROSC after 1 min then every 2 mins If at any time Pt makes a purposeful movement – STOP! And assess Pt Care of Patient Post Arrest Reassure/explain Find Cause Full physical examination Mx Other Syx: CP, SOB, N&V, UO Monitor vitals, neuro obs, IV infusion (espec of drugs that helped correct any arrhythmias) Side effects of drugs, fluid overload If intubated, only extubate when able to: Lift head off pillow Touch nose with finger Maintain ABG’s Ix: ECG, ABG, FBE, U&E, Glucose, CE’s, +/- CxR ? Transfer – ICU/other hospital Notify next of kin Documentation Causes Of Unconsciousness Other Than Cardiac Arrest: A Anaesthetics, alcohol V O M I T Vascular – bleeding (incl intracranial), PE, arrhythmias OD: intentional/accidental poisoning, envonomation Metabolic: ARF, DKA, or Na+, hepatic encephalopathy, Infection: septicaemia, (+/- shock), meningitis/encephalitis/brain abcess Trauma: head injury, haemorrhage/hypovolaemia S H E E T Syncope: postural BP Hypoxia +/- hypercarbia Epilepsy: post-ictal Endocrine: thyrotoxic, myxoedema, or glucose, HONC Tumor: cerebral Airway Obstruction: Partial Breathing is: Noisy Laboured Wheezy Stridor ie air movement present but limited NB: quieter noise = narrower airway! Mx: Reassure patient – instruct them how to breathe Allow Pt to adopt their own position Complete Breathing: Visual breathing effort, intercostals recession, tracheal tug BUT No sound of breathing or air movement in or out of lungs Mx: Clear airway/make patent Commence EAR if indicated Indications for EAR: Unconscious No air movement Pulse present/absent If EAR not successful (ie no ventilation with first breath): Children: invert child – pick up by legs Back blows Lateral chest thrust Adult: Back blows Lateral chest thrust If unsuccessful – cricothyroidotomy / emergency tracheostomy