* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 24.03.15 - irishtimes.com - Second opinion
Dirofilaria immitis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Whooping cough wikipedia , lookup
Methicillin-resistant Staphylococcus aureus wikipedia , lookup
Tuberculosis wikipedia , lookup
Anaerobic infection wikipedia , lookup
Pathogenic Escherichia coli wikipedia , lookup
Gastroenteritis wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
Neonatal infection wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
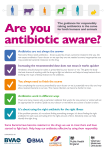
www.irishtimes.com (http://www.irishtimes.com/life-and-style/health-family/second-opinion-as-superbugs-get-smarter-wecannot-be-complacent-about-antibiotics-1.2144323) Second Opinion: As superbugs get smarter, we cannot be complacent about antibiotics Very few new types of antibiotic are being developed, leaving us in danger of antibiotic extinction Fidelma Fitzpatrick Tue, Mar 24, 2015 Now that spring is here, many of us will be out in our gardens, preparing for summer. You may often have cut yourself while gardening and sometimes these cuts get infected so you go to your doctor for an antibiotic prescription. Most of us presume that the antibiotics will do their job and we can get back to the garden that week. However, 100 years ago, before antibiotics were discovered, skin infection as a result of simple cuts frequently killed people, as did common infections such as pneumonia or tuberculosis. It is sobering to remember how much antibiotics have revolutionised medical practice in the past 75 years and saved millions of lives since their discovery. Early descriptions of the use of penicillin in the 1940s are dramatic: common infections that used to kill people could be treated for the first time. Antibiotics were quickly recognised as miracle drugs, and the possibilities they offered seemed endless. In the 30 years after the discovery of penicillin, new antibiotics were rapidly developed but, because antibiotic resistance was little understood, “superbugs” were yet to be described, and the pipeline of new antibiotics seemed endless, there was no attempt to use these agents wisely. This was the era when it was thought that antibiotics were a limitless resource and, as soon as resistance to one antibiotic emerged, the pharmaceutical industry produced newer, more effective antibiotics. By preventing and/or treating infections, antibiotics also facilitated many of the advances in medical practice that we now take for granted, such as orthopaedic surgery, chemotherapy and organ transplantation. Antibiotics are prescribed very commonly: for example, to one in three hospital patients and one in 10 long-term care residents in Ireland. We consume more antibiotics than our Scandinavian neighbours, though fewer than the Mediterranean countries. In parallel, our antibiotic resistance rates are higher than Scandinavia though lower than the Mediterranean. We have got so used to antibiotics saving lives that it is difficult to remember a time when we did not have them. However, we can no longer be complacent. Because of increasing reports of antibiotic resistance (the “superbugs”), we may be returning to a time where simple infections are no longer treatable with antibiotics. Antibiotics are very specific medications designed to work on infections caused by bacteria (for example, skin or kidney infections) and do not work on infections caused by other agents such as viruses (for example, the common cold or flu) or fungi (for example, those that can cause thrush). Antibiotic resistance is a fact of life. Bacteria have existed for billions of years and are very adept at survival. They can figure out rapidly how to protect themselves against antibiotics that are designed to kill them, particularly in situations where antibiotics are overused or if not taken exactly as prescribed. This is called antimicrobial resistance (AMR). Using antibiotics when they are not needed, or not taking an antibiotic course exactly as prescribed, gives bacteria a chance to get used to the antibiotics and to adapt so that the bacteria can’t be killed any more. These antibiotic-resistant superbugs can then go on to cause serious illness and perhaps death. Many different superbugs have been discovered and include methicillinresistantStaphylococcus (MRSA) and carbapenem-resistant Enterobacteriaceae (CRE). While antibiotic use and antibiotic resistance continues to increase, very few new types of antibiotic are now being developed, which means that we run the danger of antibiotic extinction, so we must make sure that the ones we have remain effective against infections for the sake of future generations. Though the threat of a return to the pre-antibiotic era may appear alarmist, it has been predicted that if antibiotic resistance continues to rise at current rates, by 2050 antibiotic resistance would cost US$100 trillion (€94.3 trillion); 10 million more people would die every year than if resistance rates remained at current level; and gross domestic product would reduce by between 2 per cent and 3.5 per cent. However, these studies do not take into account the dramatic social and healthcare costs of antibiotic resistance. If somebody develops an infection that antibiotics cannot kill because it has built up resistance to the treatment, then that person will become very unwell and may die. This person could have been cured if the infection had not become resistant to antibiotics. Most people who undergo surgery receive antibiotics to prevent postoperative infection, but without effective antibiotics, surgery that is now routine will become much more risky. Cancer patients receive chemotherapy treatments and transplant patients take antirejection medications that weaken their immune systems, making them much more vulnerable to infections. Without effective antibiotics to prevent and treat infections, chemotherapy and transplantation would be incredibly risky and potentially impossible. So what can be done? Clearly national and international policymakers have a role, but everybody can play a part in minimising the emergence and spread of antibiotic resistance: Firstly, you can reduce your risk of infection by living a healthy lifestyle with a good diet and exercise, getting vaccinations to prevent infectious diseases if indicated and integrating good hygienic practices (for example, food hygiene) as part of your daily routine. If you do develop an infection, practise good hygiene: use a tissue to cover your mouth when you sneeze or cough, and wash your hands afterwards. Don’t assume you need an antibiotic from your GP: if it is a viral illness, rest and time may be the solution. Use antibiotics wisely: if you are prescribed one, take it exactly as prescribed and finish the course. Don’t save antibiotics for later and don’t share them with others. The website undertheweather.ie gives sensible practical information on a range of common conditions such as colds, flu, earaches, sore throats and tummy bugs. It tells you how long they should last, what to expect, and what you can do to cope with, and recover from, these illnesses. The site includes a series of videos featuring GPs and pharmacists who offer their expertise on dealing with these common illnesses, practical remedies, and advice on when to seek medical help. Dr Fidelma Fitzpatrick is a senior lecturer at the Royal College of Surgeons in Ireland(RCSI) and consultant microbiologist at Beaumont Hospital in Dublin. Dr Fitzpatrick and Dr Nuala O’Connell of the Irish College of General Practitioners will discuss the topic of superbugs and antibiotic resistance at the RCSI MiniMed lecture tomorrow from 7-9pm at RCSI, 123 St Stephen’s Green, Dublin 2. To register for this free event, see rcsi.ie/minimed. You can join the conversation on Twitter at #RCSIMiniMed