* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Tuberculosis Record
Survey
Document related concepts
Transcript
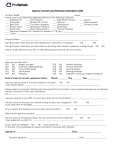
Tuberculosis Record Complete for client with suspect/active TB disease and/or TB infection For questions please call: 505-827-2471/2473/2500 Please fax this form with client demographics, H&P, Radiology & Lab reports to 505-827-0163 ECHO ID# 2. Nurse Case Manager 1. Date: Referred by: 5. Last name 3. BEHR/Medical Record # 6. First 11. Address 10. Phone(s) 16. Status 12. City 17. Race White Asian, Suspect Active TB Active TB TB Infection positive TST/ QFT/ T.Spot 18. Ethnicity & Sex Hispanic Non-Hispanic Pacific Islander Black American Indian Other NKDA Allergy List: _______________ _______________ _______________ _________ 22. Occupation: HCW Place of employment: Sex Male Female 4. Hospitalized Yes Where: 7. MI 8. DOB 13. State 19. Reason for Testing Public Health Symptoms/ diagnostic Contact to TB case Refugee Health Screen Immigration Work requirement Rheumatology Dialysis/ESRD Other: Specify:____________ Correctional Employee migrant/seasonal worker not employed 23. Diabetes 24. Substance Use 25. HIV Status 26. Lung Disease Yes No List DM Meds: _____________ _____________ _____________ _____________ ________ none injection drug use ________________ other drug use ________________ alcohol use Amount:_________ Date tested: _________ negative positive none pneumonia COPD other, specify: refused retired 27. GI/GU none CKD Dialysis Pregnancy Due Date: Date: 9. Age 14. ZIP 20. Residence Private residence Homeless Shelter Jail/prison Long Term Care Facility Substance Abuse Treatment center School Setting Other Testing by Private Provider No not seeking employment 15. County 21. Country of birth United States Mexico, specify State: Other, specify Date of entry to US Travel History: Bi-National other occupation unknown 28. Cancer/ Chemotherapy 29. Hepatitis 30. Medications none cancer immunosuppressive therapy other, Specify: none Hepatitis A Hepatitis B Hepatitis C other liver disease _______________ _____________ none steroids TNF α blockers See attached list tobacco use CLINICAL STATUS 31. TB Treatment 32. Symptoms None TB Infection no treatment TBI incomplete treatment TBI completed treatment Date:_________# months________ (Written documentation needed) TB Disease Treatment Date:_________# months________ (Written documentation needed) none cough >2-3 weeks weight loss:________lb hemoptysis night sweats fever Specimen IGRA/TST 36. TB Medications/Dosages Smear Result (TST in mm) No previous test (TST or IGRA) Previous positive test: Date________________ History of BCG lbs/kgs 35. Laboratory Diagnostics Date Date 34. Chest x-ray CXR Date: Normal Abnormal Infiltrates Cavity CT Scan: other ______________ Current wt: Current ht: BMI: Comments: 33. TB Test Results NAAT/PCR Culture Isoniazid (INH)__________ Rifampin (RIF)__________ Rifapentine:_____________ Pyrazinamide (PZA)______ Ethambutol (EMB)________ Pyridoxine (B6)___________ Moxifloxacin FAX radiology reports to TB Program @ 505.827.0163 37. Meds 38. Contact to TB Case Start date: Relation to Case:_____________ Date of last contact:___________ Sputum Smear results of case: positive negative Duration: GENType: Matches: 39. Stopped Therapy 40. Length on Therapy Completed treatment Stop date: Refused Active TB Months on therapy Moved Doses given: Adverse reaction:_______ Lost Reported by: Died Provider decision to stop Other Date: Nurse/Doctor evaluating patient: Comments: Facility/Phone: Yes No 41. Tuberculosis Classification 0 Not exposed, not infected 1 Exposed, not infected 2 LTBI 3 Active TB pulmonary extra pulmonary 4 Inactive tuberculosis 5 TB suspect 6 NTM, specify 7 Unclassified INSTRUCTIONS 1. The DOH assigned facility code for the public health office submitting the TB011 2. The name of the nurse that is responsible for the coordination of care of this patient. (Other nurse may complete related activities in the absence of the RN case manager). 3. The medical record number assigned to the patient in NM DOHs billing and electronic medical record (BEHR) system. 4. Check if the patient was hospitalized or not, write where they were hospitalized if “yes”, and the dates of hospitalization. 5. Patient’s last name, if patient has two last names be sure to include both in the correct order. 6. Patient’s first, or given, name. 7. Patient’s middle initial. 8. Patients date of birth, in format dd/mm/yyyy 9. Patient’s age, accurately reflecting their date of birth. 10. Patient’s phone number, including area code. 11. Patient’s street address. 12. The city in which the patient resides. 13. The state in which the patient resides. 14. The zip code in which the patient resides. 15. The county in which the patient resides. 16. Patient’s TB status: check the box that best fits the patient’s current status in terms of TB diagnosis at the time the TB011 is submitted. 17. Check the patient’s “race”-always ask the patient, do not make assumptions about what you believe their race is. 18. Check the patient’s ethnicity- always ask the patient, do not make assumptions about what you believe their ethnicity is. Check if the patient’s gender is male or female. 19. Check the reason the patient is being tested for TB, note the distinction between public health & private provider reasons for testing. For private providers, the patient should come with TST/IGRA results, and CXR in hand to be evaluated for TB, and/or to start LTBI treatment. 20. Check the box that best describes the patient’s place of residence. 21. Check the box indicating the country the patient was born in. For Mexico, also ask the state they were born in (i.e. Chihuahua, Oaxaca, Zacatecas, etc.) not the city. If they were born in a country other than the US or Mexico, please specify. If they recently traveled to a TB endemic country, note the country in travel history. If the patient and/or their immediate family are binational, please also check this box. 22. Check the box that best describes the patient’s occupation, and document the place if they are employed at the time the TB011 is submitted. 23. Check if the patient has been diagnosed with diabetes, and note any medication they are taking for diabetes if the answer is yes. 24. Check the box(s) that best describe substances the patient admits to using, if any. 25. Check the patient’s HIV test result for positive or negative; include the date the test was done. If test refused check the indicated box. All TB disease and LTBI patients should be offered HIV testing. 26. Check if the patient has any other lung disease diagnose(s), specify the type if other. 28. Check if the patient has been diagnosed with cancer and/or are taking chemotherapy for cancer or other conditions. 29. Check if the patient has been diagnosed with Hepatitis. If the patient admits to injection drug use, they should be tested for hepatitis B and C, with appropriate f/u depending on results. 30. Check the box that best responds to the patient’s current use of medications, allergies to medications, or other medication-related information that could affect TB care. 31. Check the box that best describes the patient’s history of TB or LTBI treatment, include the date and months treated based on written documentation of such treatment. Fax to TB program previous treatment documentation with TB Record. ( or scan into BEHR???) 32. Check all boxes for symptoms the patient had at the time the TB011 was submitted include the current weight, height and BMI. 33. Document the date(s) of any TST that was placed, or IGRA drawn, and the result. If TST documented, note the result in millimeters. If an IGRA, note positive, negative, or indeterminate. Also check the boxes about previous testing, and history of BCG vaccine. 34. Note the date a chest x-ray (CXR) was done in relation to the patient’s referral to DOH (if applicable), note the date a DOH CXR was done, and check the box that best indicates the CXR results. Be sure to fax any CXR reports related to this patient to the TB Program. 35. For any laboratory testing that was done for this patient related to TB, note the date it was done (dd/mm/yyyy), the specimen it was done on (i.e. sputum, BAL, urine or any other source) the results of the acid fast bacilli (AFB) smear (i.e. negative, 1+, 2+, 3+, 4+), results of the nucleic acid amplification (NAA) test if done, and culture results. 36. Check the box(s) indicating which TB medications the patient is being given and the dose on the line following the medication options. If other than the standard regimen, use blank space to write other medications. Include current weight in pounds here as well. 37. Indicate the date medications were started, if they were not recommended or patient refused- these are only an option for LTBI patients, and check the box to indicate the anticipated duration of treatment at the time the TB011 was submitted. 38. If the patient is a contact to an active TB case, note the cases relationship to the patient, the RVCT number (if known- otherwise the TB Program will document), the active cases smear results, date the patient had last contact with the case, and/or other case exposure information in the line provided. 39. Check the box that best describes the reason the patient stopped therapy. If other, please specify in the blank space. 40. Note the date that therapy was stopped, the number of months the patient completed, the number of doses given under directly observed therapy (DOT), the name of the person that reported the information, and the date they noted length of therapy. 41. Check the box that best describes the TB classification for the patient being evaluated and reported. COMMENTS: Please use this space for any comments you wish to report that do not fit in another section. Be as concise and clear as possible. NURSE/DOCTOR please include the name of the nurse or physician evaluating the patient FACILITY PHONE: please be sure to include the phone number (with area code) to your health office. EVALUATION DATE: please be sure to include the date that the patient was initially evaluated.