* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Practice Guidelines for Treatment of Children with LTBI
Survey
Document related concepts
Sexually transmitted infection wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Gastroenteritis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Onchocerciasis wikipedia , lookup
Tuberculosis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Hepatitis B wikipedia , lookup
Hepatitis C wikipedia , lookup
Schistosomiasis wikipedia , lookup
Transcript
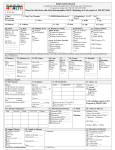
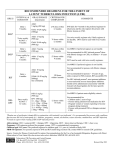
PRACTICE GUIDELINE FOR TREATMENT OF CHILDREN WITH LATENT TUBERCULOSIS INFECTION INITIAL VISIT Tuberculin skin test (TST): TST > 10 mm = positive TST > 5 mm = positive if immunosuppressed or history of exposure to active TB History: History of present illness and past medical history Possible TB exposure, sick contacts, or travel outside the United States BCG history Medications Diet Physical Examination: General physical Attention to pulmonary, lymphatic, and hepatic examination Lymph node inflammation and/or enlargement > 1 cm without other cause may indicate TB disease. Consultation with a pediatric TB or infectious disease specialist is recommended. Clinically rule out meningitis Laboratory: Chest Radiograph (CXR): PA and lateral Check specifically for: pulmonary infiltrates and/or hilar or peritracheal lymphadenopathy If abnormal the child may have TB disease. Consultation with a pediatric TB or infectious disease specialist is recommended. Liver function tests indicated only if: risk factors for hepatitis or signs or symptoms of hepatitis taking additional hepatotoxic medications (i.e. griseofulvin or anticonvulsants) Dilantin levels should be monitored if taking dilantin Public health: Report to the health department (some states require reporting of latent TB infection) If CXR is normal, child is not contagious, and may to return to school All household contacts should be skin tested Household members with positive TST should be referred to their PCP or to the health department for evaluation and CXR Treatment: Isoniazid (INH) 10-15 mg/kg/day x 9 months, daily Round to the nearest 50 mg, max dose 300 mg Tablets available as 100 mg or 300 mg, scored Liquid INH may cause diarrhea, so many experts do not use it If tablets cannot be swallowed whole, crush and dissolve in water, juice, or mix in other foods Directly observed preventive therapy (DOPT) is available through some local health departments and should be arranged if possible. Dose 20-40 mg/kg/dose (Max 900 mg/dose) given twice weekly for 9 months. Vitamin B6 supplementation is recommended for breast fed infants and children with poor nutrition (Dose: children: 25 mg tab/day; infants: 12 mg/day) Education: Provide educational information to the family regarding: Tuberculosis infection in children TB literature is available through the American Lung Association, the Centers for Disease Control and Prevention and many local health departments. Possible side effects of INH: The family should call if the child develops symptoms of toxicity, such as: nausea, loss of appetite, vomiting, diarrhea, abdominal pain that last more than a few days, jaundice, dark tea-colored urine, or a rash. FOLLOW UP VISITS: Every 4-6 weeks during therapy Review symptoms of hepatotoxicity or other problems General physical examination, specifically check for jaundice or liver enlargement If signs or symptoms of toxicity: hold medication send liver function tests (elevations of up to 3 times normal may be acceptable in asymptomatic patients) If taking dilantin, check dilantin levels and liver function tests for first 2-3 visits If taking other hepatotoxic medications, check liver function tests at first 2-3 visits If normal, can monitor clinically Medication adherence: Check bottle date and pill count Call pharmacy to verify amount dispensed if not clear Refill medication for 30-45 day supply Ask about TST results of family members and CXR results of those with positive TST If TB cultures available on source case for child’s infection, confirm sensitivity to INH Call and reschedule patients who miss follow up appointments For questions or problems call your local or state health department or a pediatric TB or infectious disease specialist for assistance. Completion of therapy: Give family documentation verifying completion of therapy. This should be kept with the child’s immunization record, as it may be needed for school or employment in the future. No tuberculin skin test ever again, as it will be positive for life. Repeat CXR only if child develops symptoms of pneumonia or has re-exposure to active TB. File completion report with the health department if required in your state.