* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Tubular reabsorption
Survey
Document related concepts
Transcript
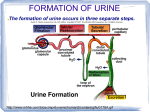
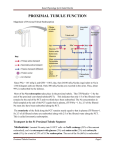
Tubular reabsorption • Tubular Reabsorption Is Selective and Quantitatively Large • The rate at which each of these substances is filtered is calculated as: • Filtration = Glomerular filtration rate x Plasma concentration • A 10 per cent decrease in tubular reabsorption, from 178.5 to 160.7 L/day, would increase urine volume from 1.5 to 19.3 L/day (almost a 13-fold increase) if the glomerular filtration rate (GFR) remained constant. Tubular Reabsorption Filtered substances are transferred from the tubular lumen to the peritubular capillaries This process is highly selective and variable. The return of substances to the blood is needed to maintain the composition of the ECF. Only excesses of materials are eliminated. Reabsorption rates are high: 124 of 125 ml of filtered fluid per minute, 99% for water 100% for glucose 99.5% for salt. 3 Tubular reabsorption involves transepithelial transport Reabsorbed substance must cross: 1. tubule wall 2. interstitial fluid, 3. wall of the peritubular capillaries thus entering the blood. The single layer of epithelial cells of the nephron tubule has: i. luminal membrane (facing tubule lumen) ii. basolateral membrane (facing the interstitial spaces between the tubule and peritubular capillaries) 4 Active transport A. Primary Active: Na-K, Hydrogen, H-K, and Calcium pumps. Sodium: on basolateral sides, Na-K pump, creates negatives inside increases Nainflux. B. Secondary active : Co-transport, countertransport . Na -Glcose , Na - a.a , Na - H+ C. Pinocytosis: Proteins. Basic mechanism for active transport of sodium through the tubular epithelial cell Involves a Na-K ion ATPase carrier in the tubular cell’s basolateral membrane This pump keeps sodium concentration low in the tubular cells and high in the lateral spaces outside the tubule. Water follows reabsorbed sodium by osmosis. Thus, sodium reabsorption has a main effect on blood volume and blood pressure. Aldosterone promotes Na+ retention by insertion of additional Na+ channels into the luminal membrane, and additional Na+/K+ ATPase into the basolateral membrane of the distal and collecting tubules. Reabsorption of Na+ Of the Na+ filtered, 99.5% is normally reabsorbed. Sodium is reabsorbed throughout the tubule with the exception of the descending limb of the loop of Henle Of the Na+ reabsorbed, on average • 67% in the proximal tubule (Plays an important role in the reabsorption of glucose, amino acids, water, chloride ions, and urea) • 25% in the loop of Henle (Plays a role in the production of varying concentrations and volumes of the urine) • 8% in the distal and collecting tubules (depends on hormonal control, and plays an important role in regulating ECF volume). Aldosterone (stimulated via renin system) increases Na+ reabsorption Atrial Natriuretic Peptide “ANP” (released from heart) decreases Na+ reabsorption 8 Mechanism of Aldosterone Action Mechanisms of secondary active transport Transport maximum for substances that are actively reabsorbed • Due saturation, when tubular load exceeds capacity of carrier and specific enzymes. • Transport maximums for substances actively reabsorbed: • Transport Maximums for Substances That Are Actively Secreted: – Creatinine 16 mg/min – Para-aminohippuric acid 80 mg/min • Tm Na+ in proximal tubule does not exist because it is referred as (gradient-time transport) the greater [Na+] the greater reabsorption . – Because the rate of transport depends on the electrochemical gradient and the time that the substance is in the tubule, which in turn depends on the tubular flow rate. Gradient-time Transport • Substances that are passively reabsorbed usually do not demonstrate a transport maximum because their rate of transport is determined by other factors such as: 1. Electrochemical gradient for diffusion of the substance across the membrane 2. Permeability of the membrane for the substance 3. Time that the fluid containing the substance remains within the tubule Splay Passive Water reabsorption • Passive water reabsorption by osmosis is coupled mainly to sodium reabsorption • When the interstitium is hypertonic: – large part through tight junctions and solvent drag some solute w/water . • Ascending and first part of distal tubule are impermeable for water • ADH ↑permeability in distal, and coll. tubule Chloride reabsorption • Na+ inside cells attracts (-) charge of chloride (paracellular) • Also Cl- passively after water influx [Cl-] out higher • Also secondary active transport Na+ - Cl- Urea reabsorption • Urea is passively reabsorbed from the tubule, but to a much lesser extent than chloride ions. • As water is reabsorbed from the tubules (by osmosis coupled to sodium reabsorption), urea concentration in the tubular lumen increases a concentration gradient favoring the reabsorption of urea. Reabsorption and Secretion Along Different Parts of the Nephron Proximal Tubular Reabsorption • Proximal Tubules Have a High Capacity for Active and Passive Reabsorption. • Special cellular characteristics. • Highly metabolic and have large numbers of mitochondria to support potent active transport processes. • Extensive brush border on the luminal membrane • In the first half of the proximal tubule, sodium is reabsorbed by co-transport along with glucose, amino acids, and other solutes. • In the second half of the proximal tubule, little glucose and amino acids remain to be reabsorbed. Instead, sodium is now reabsorbed mainly with chloride ions. Secretion of Organic Acids and Bases by the Proximal Tubule The proximal tubule is also an important site for secretion of organic acids and bases such as bile salts, oxalate, urate, and catecholamines. Concentrations of Solutes Along the Proximal Tubule Solute and Water Transport in the Loop of Henle • The loop of Henle consists of three functionally distinct segments: 1. the thin descending segment, 2. the thin ascending segment, 3. and the thick ascending segment. • The thick segment of the ascending loop of Henle is virtually impermeable to water. • There is a significant paracellular reabsorption of cations, such as Mg++, Ca++, Na+, and K+, in the thick ascending limb owing to the slight positive charge of the tubular lumen relative to the interstitial fluid. Mechanisms of sodium, chloride, and potassium transport in the thick ascending loop of Henle. In the thick ascending loop, movement of sodium across the luminal membrane is mediated primarily by a 1-sodium, 2-chloride, 1-potassium co-transporter Distal Tubule • The very first portion of the distal tubule forms part of the juxtaglomerular complex. • The next part of the distal tubule is highly convoluted and has many of the same reabsorptive characteristics of the thick segment of the ascending limb of the loop of Henle. • Reabsorbs most of the ions, including sodium, potassium, and chloride • Impermeable to water and urea. • Referred to as the diluting segment because it also dilutes the tubular fluid. Late distal tubule and collecting tubule Principal Cells Reabsorb Sodium and Secrete Potassium • Depend on the activity of a sodium-potassium ATPase pump in each cell’s basolateral membrane. • The principal cells are the primary sites of action of the potassium-sparing diuretics. • Aldosterone antagonists inhibit the stimulatory effects of aldosterone on sodium reabsorption and potassium secretion. • Sodium channel blockers directly inhibit the entry of sodium into the sodium channels of the luminal membranes and therefore reduce the amount of sodium that can be transported across the basolateral membranes by the sodium-potassium ATPase pump. Intercalated Cells Avidly Secrete Hydrogen and Reabsorb Bicarbonate and Potassium Ions • Hydrogen ion secretion by the intercalated cells is mediated by a hydrogen- ATPase transport mechanism. • Hydrogen is generated in this cell by the action of carbonic anhydrase on water and carbon dioxide to form carbonic acid, which then dissociates into hydrogen ions and bicarbonate ions. • The hydrogen ions are then secreted into the tubular lumen, and for each hydrogen ion secreted, a bicarbonate ion becomes available for reabsorption across the basolateral membrane. Medullary Collecting Duct • Reabsorb less than 10 per cent of the filtered water and sodium. • The final site for processing the urine. • Play an extremely important role in determining the final urine output of water and solutes. Characteristics of medullary collecting duct • Its permeability to water is controlled by the level of ADH. • Unlike the cortical collecting tubule, the medullary collecting duct is permeable to urea. Therefore, some of the tubular urea is reabsorbed into the medullary interstitium, helping to raise the osmolality in this region of the kidneys and contributing to the kidneys’ overall ability to form a concentrated urine. • The medullary collecting duct is capable of secreting hydrogen ions against a large concentration gradient, as also occurs in the cortical collecting tubule. Thus, the medullary collecting duct also plays a key role in regulating acid-base balance. Summary of Concentrations of Different Solutes in the Different Tubular Segments Regulation of Tubular Reabsorption It is essential to maintain a precise balance between tubular reabsorption and glomerular filtration. •Glomerulotubular Balance • Peritubular Physical Forces • Hormones - aldosterone - angiotensin II - antidiuretic hormone (ADH) - natriuretic hormones (ANF) - parathyroid hormone • Sympathetic Nervous System • Arterial Pressure (pressure natriuresis) • Osmotic factors. Glomerulotubular Balance: The Ability of the Tubules to Increase Reabsorption Rate in Response to Increased Tubular Load • If GFR↑ to 150 ml/min so in proximal tubule reabsorption ↑ from 81 ml/min to 97.5 ml/min. (65% of GFR) . To less extent in Loop of Henle. • Intrinsic ability of the tubules to increase their reabsorption rate in response to increased tubular load (increased tubular inflow). • The mechanisms for glomerulotubular balance can occur independently of hormones and can be demonstrated in completely isolated kidneys or even in completely isolated proximal tubular segments. • It helps to prevent overloading of the distal tubular segments when GFR increases. Peritubular capillary and interstitial fluid physical forces a. b. c. d. Hydrostatic pr. In capillary Pc opposes -13 Hydrostatic pr. In interstitium Pif favors 6 Colloid osmotic pr. in capillary πc favors 32 Colloid osmotic pr. In intrst. πif opposes -15 ____ Net reab. Pr. 10 mmHg Reabsorption = Kf x Net reabsorptive pr. 12.4 x 10 = 124 ml/min Peritubular Capillary and Renal Interstitial Fluid Physical Forces Reabsorption across the peritubular capillaries can be calculated as: Reabsorption = Kf x Net reabsorptive force A. Hydrostatic pr. depends on BP, and resistance of aff. And eff. Arterioles: ↑Arterial pr.↑ hydrostatic decreases reabsorption Change in the resistance of afferent and efferent: constriction decreases hydrostatic ↑ reabsorption. B. Colloid osm. Pr. depends: on [prot.]pl, and filtration fraction. - ↑Plasma colloid osmotic pr.↑ coll. In perit.↑ reabs. - ↑Filtration fraction ↑ [protein] ^reabsorption 2. Hormonal control : Aldosterone : Acts on the distal tubule and collecting ducts; Na Cl , H2O reabs. acts on principal calls of cortical coll. tubule and increases K+ secretion. Addison's disease : no aldosterone loss of Na+, accumulation of K+ Conn's syndrome : Na+ retention K+ depletion Aldosterone actions on late distal, cortical and medullary collecting tubules • Increases Na+ reabsorption - principal cells • Increases K+ secretion - principal cells • Increases H+ secretion - intercalated cells Angiotensin II Increases Na+ and Water Reabsorption • Stimulates aldosterone secretion • Directly increases Na+ reabsorption (proximal, loop, distal, collecting tubules) • Constricts efferent arterioles - decreases peritubular capillary hydrostatic pressure - increases filtration fraction, which increases peritubular colloid osmotic pressure) c. ADH : on distal and coll. duct ↑H2O reabsorption : - Binds V2 receptors form cyclic AMP increase aquaporin-2 on luminal, AQP3,4 on basolateral - When ADH decreased AQP back to cytoplasm Hormonal control d.Arterial natriuretic peptide : Decrease Na+ and H2O reabsorption in distal and collecting duct e. Parathyroid hormone : - in Prox. tubule: decreases PO4- reabsorption - in thick ascending of L.H, distal tubule ↑Ca++ reabsorption 3. Sympathetic N.S. - Sympathetic N.S. : Stimulation ↑Na+ and H2O reabs. by constricting afferent and efferent arterioles.