* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
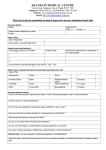
Download vaccination requirements and malaria chemoprophylaxis for un staff
Sociality and disease transmission wikipedia , lookup
Infection control wikipedia , lookup
Neonatal infection wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Gastroenteritis wikipedia , lookup
Poliomyelitis eradication wikipedia , lookup
Herd immunity wikipedia , lookup
Germ theory of disease wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Hepatitis B wikipedia , lookup
Typhoid fever wikipedia , lookup
Immunocontraception wikipedia , lookup
Whooping cough wikipedia , lookup
Globalization and disease wikipedia , lookup
Meningococcal disease wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Non-specific effect of vaccines wikipedia , lookup
Vaccination policy wikipedia , lookup
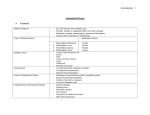
VACCINATION REQUIREMENTS AND MALARIA CHEMOPROPHYLAXIS FOR UN STAFF AND HUMANITARIAN WORKERS TRAVELLING TO CENTRAL ASIA UPDATE NO 1 October 2001 Routine vaccinations recommended - check vaccination history to ensure immunisations are up to date Diphtheria Tetanus Polio Hepatitis A Hepatitis B Typhoid fever IM Recommendations on additional vaccines Meningococcal disease Meningococcal vaccine is recommended. The tetravalent vaccine (A,C,Y & W135) can be used if available (one case of serogroup W135 disease has been confirmed in Pakistan following the Haj this year). If tetravalent vaccine is not available, bivalent (A&C) vaccine should be adequate as over recent years documented outbreaks of meningococcal disease in Central Asia have been associated with serogroup A. Rabies Rabies vaccine is recommended. 2,000 – 10,000 cases reported in Pakistan annually. Potential for delay in accessing health care in event of exposure due to security situation puts UN workers at high risk. Important to consider stockpiles of post exposure therapy and evacuation plan. Measles Majority of adult population have protective immunity due to measles infection or vaccination in childhood. Check vaccination history - if no history of measles infection or measles vaccination, measles vaccine may be given. Cholera Cholera vaccine is NOT recommended. Priority is prevention measures - safe water, cooked food Cholera season in Central Asia is from March to October In event of a confirmed cholera epidemic, the recommendations regarding oral cholera vaccine will be reconsidered. Note: A yellow fever vaccination certificate is required from travellers coming from infected areas. Malaria chemoprophylaxis Pakistan, Afghanistan, Iran – chloroquine plus proguanil Tajikistan – chloroquine Uzbekistan, Turkmenistan – prophylaxis not recommended If more than one country is visited: follow the advice for the most endemic country. Update no 1 October 2001 Combine with protection against mosquito bites, especially between dusk and dawn. Malaria Chemoprophylaxis: Afghanistan Season: May – November in areas below 1500 m Recommended: Chloroquine 300mg weekly in combination with proguanil 200 mg daily. Alternatively, chloroquine can be taken as 600mg per week, divided over 6 daily doses, in combination with daily proguanil1. Iran Limited risk–exclusively in the benign (P. vivax) form–exists in some areas north of the Zagros mountains and in western and south-western regions during the summer months. Malaria risk in the malignant (P. falciparum) form exists from March through November in rural areas of the provinces of Hormozgan, Kerman (tropical part) and Sistan-Baluchestan. Recommended in P.falciparum risk areas: chloroquine 300mg weekly in combination with proguanil 200 mg daily. Alternatively, chloroquine can be taken as 600mg per week, divided over 6 daily doses, in combination with daily proguanil. Pakistan Season: mainly from April to December. Year-round transmission in the southern part of the country Recommended: chloroquine 300mg weekly in combination with proguanil 200 mg daily. Alternatively, chloroquine can be taken as 600mg per week, divided over 6 daily doses, in combination with daily proguanil. Tajikistan Season: May - October. Malaria risk exists particularly in the southern part of the country (Khatlon region) and to a lesser extent in some central, western and northern areas. Recommended: Chloroquine 300mg weekly. Alternatively, chloroquine can be taken as 600mg per week, divided over 6 daily doses. Turkmenistan No malaria chemoprophylaxis necessary. Uzbekistan No malaria chemoprophylaxis necessary. Alternative chemoprophylaxis options: mefloquine (250mg weekly) or doxycycline (100 mg daily) Chloroquine and mefloquine should be started at least a week before arrival or before the beginning of the transmission season; proguanil and doxycycline should be started 1 In several countries a combination tablet containing 100mg chloroquine base plus 200 mg proguanil hydrochloride (common trade name: Savarine) is available, which may improve compliance. Update no 1 October 2001 the day before. The drugs should be continued for 4 weeks after departure from the endemic area. Malaria Emergency Standby Treatment: Chemoprophylaxis can not offer 100% protection. In case of a breakthrough, suspected malaria infections can be treated with quinine, given as 8 mg base/kg bodyweight 3 times daily for 7 days, or with mefloquine, taken as 15 mg base/kg bodyweight in a single dose, i.e., 4 tablets for an adult (only when not taking mefloquine prophylaxis). Urgent medical attention should be sought to confirm the diagnosis and adjust the treatment, and to exclude other causes of fever. Source: International Travel and Health 2001 – vaccination requirements and health advice. WHO Geneva, 2001. http://www.who.int/ith Update no 1 October 2001 Updates of this protocol may become necessary in case of epidemics, and when new data on drug resistance and transmission become available. Update no 1 October 2001