* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Types of Anxiety Disorders
Psychedelic therapy wikipedia , lookup
Drug design wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Pharmacognosy wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Serotonin syndrome wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Drug interaction wikipedia , lookup
Neuropharmacology wikipedia , lookup
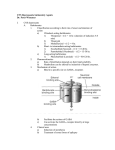
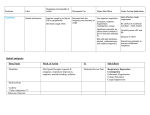
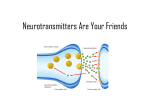
Types of Anxiety Disorders Situational anxiety: anxiety experienced by people faced with a stressful environment o Beneficial because it motivates people to accomplish tasks in a prompt manner; May be intense o Patients often learn coping mechanisms o Generalized anxiety disorder (GAD) difficult to control, excessive anxiety that lasts 6 months or more Focuses on a variety of life events or activities, and interferes with normal day-to-day functions Most common; most frequently encountered by the nurse Symptoms = restlessness, fatigues, muscle tension, nervousness, inability to focus or concentrate, overwhelming sense of dread, sleep disturbances, elevated BP, heart palpitations, respiratory change, dry mouth, abdominal cramping, diarrhea, urinary urgency Women are slightly more likely to experience GAD o Panic disorder: characterized by an intense feeling of immediate apprehension, fearfulness, terror, or impending doom, accompanied by increase autonomic nervous system activity o Phobias: fearful feelings attached to situations or objects Common phobias include fear of snakes, spiders, crowds, and heights Social anxiety = fear of crowds Performance anxiety: performers may experience feelings of dread, nervousness, or apprehension before a performance Phobias compel a patient to avoid the fearful stimulus entirely to the point that his or her behavior is unnatural o Obsessive-compulsive disorder (OCD): an unnatural behavior, that involves recurrent, intrusive thoughts or repetitive behaviors that interfere with normal activities or relationships Fear of germs or repetitive hand washing o Post-traumatic stress disorder (PTSD): a type of situational anxiety that develops in response to re-experiencing a previous life event Traumatic life events such as war, physical or sexual abuse, natural disasters, or murder may lead to a sense of helplessness and reexperiencing of the event Specific Regions of the Brain Responsible for Anxiety and Wakefulness Limbic system: an area in the middle of the brain responsible for emotional expression, learning and memory o Signals routed through the limbic system ultimately connect with the hypothalamus o Anxiety, fear, anger, aggression, remorse, depression, sexual drive, and euphoria Hypothalamus – an important center responsible for unconscious response to extreme stress such as high BP, elevated respiratory rate, and dilated pupils Responses associated with fight-or-flight response o Connects with the reticular formation o reticular formation: a network of neurons found along the entire length of the brainstem stimulation causes heightened alertness and arousal inhibition causes general drowsiness and the induction of sleep Area responsible for Sleep and Wakefulness reticular activating system (RAS) – larger area in which the reticular formation is found; connects the brainstem to the thalamus o responsible for sleeping and wakefulness o performs an alerting function for the entire cerebral cortex o helps a person focus attention on individual tasks by transmitting information to higher brain centers if signals are prevented from passing through the RAS, no emotion-related signals are sent to the brain, resulting in a reduction in general brain activity Anxiety Management through Pharmacologic most productive way to manage stress = anxiolytics stress is often a symptom of an underlying disorder more productive to treat the cause of anxiety rather than just the symptoms with medication Anxiolytics: drugs having the ability to relieve anxiety; provide treatment for phobias, PTSD, GAD, OCD, and panic attacks o Antidepressants o CNS depressants (drugs for seizures) o Emotional & mood disorder drugs o Antihypertensive drugs o Antidysrhythmic drugs Indication for the need of pharmacotherapy in patient with anxiety Assess intensity and duration of symptoms Identify precipitating factors Identify coping mechanisms Assess for sleep disorders Obtain a drug history o Hypersensitivity o Use of alcohol & other CNS depressants o Drug abuse & dependence Use caution for certain clients o Those who are elderly o Those with suicidal potential o Those with impaired renal or liver function Table 14.1 Stages of Sleep Stage Description NREM Stage 1 NREM Stage 2 NREM Stage 3 NREM Stage 4 REM Sleep At the onset of sleep, the patient is in a stage of drowsiness for about 1 to 7 minutes patient can be easily awakened lasts for about 4% to 5% of total sleep time. The patient can still be easily awakened This stage constitutes the greatest amount of total sleep time, 45% to 55%. The patient may move into or out of a deeper sleep HR & BP fall GI activity rises lasts for about 4% to 6% of total sleep time. The deepest stage of sleep, 12% to 15% of total sleep time nightmares occur in children Sleepwalking is also a common behavior for this stage HR & BP remain low GI activity remains high. This stage is characterized by eye movement and a loss of muscle tone Eye movement occurs in burst of activity. Dreaming takes place in this stage The mind is very active and resembles a normal waking state. Treating Anxiety & Insomnia with CNS Agents Have an ability to reduce anxiety symptoms by altering levels of norepinephrine and serotonin Restoration of neurotransmitter imbalances may reduce symptoms associated with depression, panic, OCD, and phobia Typical antidepressants o Tricyclic antidepressants (TCAs) o Selective serotonin reuptake inhibitors (SSRIs) o Monoamine oxidase inhibitors (MAOIs) Categorized into 2 classes = Benzodiazepines & Barbiturates Other CNS depressants that have a calming effect in the body include the opioids and ethyl alcohol Should be viewed as a continuum ranging from relaxation to sedation, to the induction of sleep and anesthesia Coma and death are the end stages of CNS depression Can cause physical or psychological dependence Sedatives: medications that depress the CNS because of their ability to sedate or relax a patient Hypnotics: at higher does, sedatives are called hypnotics because of their high ability to induce sleep Sedative-Hypnotic: term used to describe a drug with the ability to produce a calming effect at lower doses and the ability to induce sleep at high doses Tranquilizer: an older term, sometimes used to describe a drug that produces a calm or tranquil effect Withdrawal Syndrome o for some CNS depressants can cause life threatening neurologic reactions o fever, psychosis, seizures o increased heart rate o lowered blood pressure o loss of appetite o muscle cramps o impairment of memory, concentration, and orientation o abnormal sounds in the ears and blurred vision o insomnia, agitation, anxiety, and panic Table 14.3 SSRIs – Fluoxetine (Prozac) Adverse Effects Stevens-Johnson Syndrome Abnormal bleeding Extreme mania/hypomania Extreme psychomotor disturbances Suicidality (especially in children) Seizures Autonomic instability with possible rapid fluctuations of vital signs Severe hyperthermia Serotonin syndrome Antidepressants → treat major depression and anxiety conditions including GAD, OCD, panic, phobia, and PTSD Mechanism of action – increase availability of serotonin at specific postsynaptic receptor sites located within the CNS o Adverse Effects – dizziness, nausea, insomnia, somnolence, confusion, seizures MAOIs (monoamine oxidase inhibitors) o Avoid foods containing tyramine, a form of the amino acid tyrosine, to avoid a hypertensive crisis o Refrain from caffeine intake o MAOIs potentiate the effects of insulin and other diabetic drugs o Adverse Effects – orthostatic hypotension, headache, diarrhea o Rarely used because of the potential for serious adverse effects Prototype Drug Escitalopram Action and Uses – selective serotonin reuptake inhibitor (SSRI) o Increases the availability of serotonin at specific postsynaptic receptor sites located within the CNS o Selective inhibition of serotonin reuptake results in antidepressant activity without production of symptoms of sympathomimetics or anticholinergic activity o This medication is indicated for conditions of generalized anxiety and depression o Unlabeled uses include the treatment of panic disorder Drug-Drug Interactions o Should be avoided dur to serotonin syndrome, marked by autonomic hyperactivity, hyperthermia, rigidity, diaphoresis, and neuroleptic malignant syndrome o Combination with MAOIs can result in hypertensive crisis, hyperthermia, and autonomic instability o Will increase plasma levels of metoprolol and cometidine o Concurrent use of alcohol and other CNS depressants may enhance CNS depressant effects Treating Anxiety and insomnia with benzodiazepines Withdrawal Effect? Why are they the drug of choice? o Drug of choice for short-term treatment of insomnia caused by anxiety o They have replaced barbiturates because of their greater safety margin o Shorten the length of time it takes to fall asleep o Reduce the frequency of interrupted sleep Table 14.4 Clonazepam (Klonopin) Adverse Effects Acute hyperexcited states increased Muscle spasticity Hallucinations Renal impairment Congenital defects among women who are pregnant Respiratory impairment due to hypersalivation Respiratory depression Laryngospasm Cardiovascular collapse Table 14.4 Lorazepam (Ativan) Adverse effect Drowsiness and sedation When given in higher doses or by the IV route, more severe effects may be observed o Amnesia o Blood pressure changes o Weakness o Blurred vision o Disorientation o Double vision o Ataxia o Nausea o Sleep disturbance o Vomiting Should be monitored carefully due to rapid onset of CNS effects and potential respiratory depression with adjunctive therapies Drug of choice for short-term treatment of insomnia cause by anxiety Barbiturates (Why are they not the drug of choice?) Drugs derived from barbituric acid Powerful CNS depressants prescribed for their sedative, hypnotic, and antiseizure effects Rarely used because of significant adverse effects High Risk of psychologic and physical dependence – Schedule II drugs Withdrawal syndrome is extremely severe and can be fatal Overdose results in profound respiratory depression, hypotension, and shock Capable of depression CNS function at all levels Intensify the effects of GABA throughout the brain by binding to GABA receptorchloride channel molecules o low doses = reduce anxiety and cause drowsiness o moderate doses = inhibit seizure activity and promote sleep by inhibiting brain impulses traveling through the limbic system & the RAS o high doses = can induce anesthesia tolerance can develop with repeated use Table 14.5 Barbiturates for Sedation & Insomnia Adverse Effects of Antiseizure Medication o Short acting = Respiratory depression, laryngospasm, & apnea o Intermediate acting = agranulocytosis, angioedema, Stevens-Johnson syndrome, respiratory depression, circulatory collapse, apnea, laryngospasm o Long Acting = agranulocytosis, respiratory depression, Stevens-Johnson syndrome, exfoliative dermatitis (rare), CNS depression, coma & death Other CNS depressants for anxiety and sleep disorders Chemically unrelated to either benzodiazepines or barbiturates Antiseizure medication valporate Beta blocker propanolol and Atenolol Drugs used mainly for insomnia therapy include the newest of all nonbenzodiazepines CNS depressants o Zaleplon o Eszopiclone – used for hypnotic effects o Zolpidem – used for hypnotic effects Older CNS depressants include o Paraldehyde o Chloral hydrate Buspirone and zolpidem are commonly prescribed for anxiolytic effects Buspirone mechanism of action is unclear o Appears to be related to D2 dopamine receptors in the brain o Has agonist effects on presynaptic dopamine receptors and a high affinity for serotonin receptors o Less likely to affects cognitive and motor performance o Rarely interacts with other CNS depressants o Adverse effects = dizziness, headache, drowsiness o Dependence and withdrawal problems are less of a concern Zolpidem – Schedule IV controlled substance o Limited to short-term treatment of insomnia o Highly specific to GABA receptors o Produces muscle relaxation and anticonvulsant effects only at doses much higher than the hypnotic dose o Used cautiously in patients with respiratory impairment, older adults, and when used concurrently with other CNS depressants o Because it is metabolized in the liver and excreted by the kidneys, impaired liver or kidney function can increase serum drug levels o Adverse Effects = mild nausea, dizziness, diarrhea, daytime drowsiness, rebound insomnia may occur with discontinued use, amnesia, sleepwalking Prototype drug Zolpidem (Ambien) Adverse effects o Daytime sedation o Dizziness o Confusion o Depression o Amnesia o Nausea vomiting Drug-Drug Interaction – drug interactions include an increase in sedation when used concurrently with other CNS depressants, including alcohol o Phenothiazines augment CNS depression Herbal & Food Interaction – when taken with food, absorption is slowed significantly, and the onset of action may be delayed Nursing implications Assessment Potential nursing diagnoses o Risk for injury o Knowledge deficit related to drug therapy o Ineffective individual coping Reason for the drug, Monitoring vital signs, Cautions and contraindications Possible drug interactions o Completing health history o Drug history o Evaluation of lab reports Planning → client will o Experience therapeutic effects depending on drug o Be free of adverse effects o Demonstrate an understanding of the drugs activity o Accurately describe drug side effects and precautions o Demonstrate proper self-administration technique Implementation o Interventions & rationales o Administration of drugs o Observe for adverse effects o Client education and discharge planning Evaluation o Effectiveness of Drug therapy o Evaluate the achievement of the goals & expected outcomes