* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Advances in EP Cardiology - For Medical Professionals
Heart failure wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Electrocardiography wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Coronary artery disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
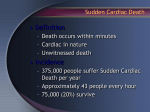
Electrophysiology 2011 Taresh Taneja, MD, FACC Assistant Professor of Medicine Texas A & M HSC COM Scott & White Hospital “The more things change, the more they stay the same.” Jean-Baptiste Alphonse Karr EP 2011 Sudden Cardiac Death Cardiac Resynchronization Therapy Syncope Atrial Fibrillation Case Vignette • A 74-year-old man with a history of hypertension and myocardial infarction that occurred 5 years previously presents with breathlessness on exertion. • His current medications include a statin and aspirin. • On examination, his pulse is 76 beats per minute and regular, and his blood pressure is 121/74 mm Hg. • There is jugular venous distention, lateral displacement of the apex beat, and edema in his lower limbs. • The lung examination is normal. • An echocardiogram shows left ventricular dilatation, globally reduced contractility, and an ejection fraction of 33%. • How should his case be managed? Pathophysiology of Systolic Heart Failure McMurray J. N Engl J Med 2010;362:228-238 Clinical Classifications of Heart Failure Severity McMurray J. N Engl J Med 2010;362:228-238 Treatment Algorithm for Systolic Heart Failure McMurray J. N Engl J Med 2010;362:228-238 Telemetry Strip Showing Pause-Independent Polymorphic Ventricular Tachycardia. Britton KA et al. N Engl J Med 2010;362:1721-1726. Sudden Cardiac Death (SCD) Death from unexpected circulatory arrest, usually due to cardiac arrhythmia occurring within an hour of the onset of symptoms. Sudden Cardiac Arrest (SCA)- Episode of resuscitated SCD Sudden Cardiac Death Estimates range 200,000 - 450, 000 SCD’s annually depending on the definition used. 13% of all natural deaths are SCD using the 1 hour definition. 50% of all CHD deaths are sudden. Overall incidence of SCD 1 to 2/1000 population. 36 cc Implantable Cardioverter Defibrillator (ICD) Secondary Prevention- Multiple studies have shown a 50% relative-risk reduction in arrhythmic death and a 25% relativerisk reduction in all-cause mortality. Patients who die once are more likely to die again. Primary Prevention of SCD • Patients with a history of myocardial infarction and a reduced ejection fraction are at increased risk for life-threatening ventricular arrhythmias. • Which of these patients are the most appropriate candidates for implantable cardioverter–defibrillator (ICD) therapy is unclear. Summary of Major Randomized Trials of ICD Therapy for Primary Prevention of Sudden Death after Myocardial Infarction Myerburg R. N Engl J Med 2008;359:2245-2253 Amiodarone or an Implantable CardioverterDefibrillator for Congestive Heart Failure Gust H. Bardy, M.D., Kerry L. Lee, Ph.D., Daniel B. Mark, M.D., Jeanne E. Poole, M.D., Douglas L. Packer, M.D., Robin Boineau, M.D., Michael Domanski, M.D., Charles Troutman, R.N., Jill Anderson, R.N., George Johnson, B.S.E.E., Steven E. McNulty, M.S., Nancy Clapp-Channing, R.N., M.P.H., Linda D. Davidson-Ray, M.A., Elizabeth S. Fraulo, R.N., Daniel P. Fishbein, M.D., Richard M. Luceri, M.D., John H. Ip, M.D. and the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators N Engl J Med Volume 352;3:225-237 January 20, 2005 Study Overview This placebo-controlled study compared the effect of amiodarone and an implantable cardioverter-defibrillator (ICD) on mortality in patients with New York Heart Association class II or III congestive heart failure (CHF) Amiodarone had no benefit overall and slightly increased mortality among patients with class III CHF ICD therapy reduced mortality overall, but the benefit appeared to be restricted to patients with class II CHF These important results will broaden the use of ICD therapy SCD-HeFT Protocol DCM + CAD and CHF EF < 35% NYHA Class II or III 6-Minute Walk, Holter R Placebo N = 847 Amiodarone N = 845 2521 Patients ICD Implant N = 829 Minimum of 2.5 years follow-up required 45 months average follow-up Optimized B, ACE-I, Diuretics Bardy GH. N Engl J Med. 2005;352:225-237. Kaplan-Meier Estimates of Death from Any Cause Bardy, G. et al. N Engl J Med 2005;352:225-237 Kaplan-Meier Estimates of Death from Any Cause for the Prespecified Subgroups of Ischemic CHF (Panel A) and Nonischemic CHF (Panel B) Bardy, G. et al. N Engl J Med 2005;352:225-237 Kaplan-Meier Estimates of Death from Any Cause for the Prespecified Subgroups of NYHA Class II (Panel A) and Class III (Panel B) Bardy, G. et al. N Engl J Med 2005;352:225-237 Hazard Ratios for the Comparison of Amiodarone and ICD Therapy with Placebo in Various Subgroups of Interest Bardy, G. et al. N Engl J Med 2005;352:225-237 Conclusions In patients with NYHA class II or III CHF and LVEF of 35 percent or less, amiodarone has no favorable effect on survival, whereas single-lead, shock-only ICD therapy reduces overall mortality by 23 percent Incremental Cost-Effectiveness Cardiovascular Interventions Incremental Cost per Life-Year Saved $200,000 Economically Unattractive $150,000 $135,000 $120,000 Expensive $67,000 Borderline Cost-Effective $40,750 Cost-Effective $17,701 Highly Cost-Effective $8,461 PTCA Hypertension CABG (chronic CAD, Therapy (chronic severe angina (diastolic CAD 1 VD) 95 - 104 mild angina, mmHg) 3 VD) End Stage Renal Disease Treatment Exercise SPECT (atypical angina who can walk on treadmill) Lovastatin (chol. = 290 mg/dL, 50 yrs old, male, no risk factors) Carotid Disease Screening (65 yrs old, male, no symptoms) Routine Coronary Angiography (35 - 84 yrs old, low risk MI, has CHF) Incremental Cost per Life-Year Saved Incremental Cost-Effectiveness ICD, CRT, and CRT-D Therapies Economically Unattractive Expensive $67,000 $50,000 $28,000 $33,000 Borderline Cost-Effective $38,200 Cost-Effective Highly Cost-Effective COMPANION CRT1 1 Feldman AM. SCD-HeFT ICD2 COMPANION CRT-D1 www.theheart.org. ACC News. March 16, 2005. Mark DB. www.theheart.org. AHA News. November 11, 2004. 3 Ak-Khatib S. Ann Intern Med. 2005;142:593-600. 4 Larsen G. Circulation. 2002;105:2049-2057. 2 MADIT-II ICD3 AVID ICD4 Original Article Defibrillator Implantation Early after Myocardial Infarction Gerhard Steinbeck, M.D., Dietrich Andresen, M.D., Karlheinz Seidl, M.D., Johannes Brachmann, M.D., Ellen Hoffmann, M.D., Dariusz Wojciechowski, M.D., Zdzisława Kornacewicz-Jach, M.D., Beata Sredniawa, M.D., Géza Lupkovics, M.D., Franz Hofgärtner, M.D., Andrzej Lubinski, M.D., Mårten Rosenqvist, M.D., Alphonsus Habets, Ph.D., Karl Wegscheider, Ph.D., Jochen Senges, M.D., for the IRIS Investigators N Engl J Med Volume 361(15):1427-1436 October 8, 2009 Study Overview • Implantation of a defibrillator early after myocardial infarction (MI) in high-risk patients reduced the risk of sudden cardiac death, but there was a reciprocal increase in the risk of nonsudden cardiac death • Overall mortality was not affected by early defibrillator implantation, and therefore this intervention cannot be recommended after MI in high-risk patients Baseline Demographic and Clinical Characteristics of the Patients, According to Study Group Steinbeck G et al. N Engl J Med 2009;361:1427-1436 Cumulative Risk of Death from Any Cause According to Study Group Steinbeck G et al. N Engl J Med 2009;361:1427-1436 Cumulative Risk of Cardiac Death, According to Study Group Steinbeck G et al. N Engl J Med 2009;361:1427-1436 Conclusion Prophylactic ICD therapy did not reduce overall mortality among patients with acute myocardial infarction and clinical features that placed them at increased risk ICD implantation Post Acute MI Acute MI-Sudden Cardiac Death paradox firmly established SCD post-MI may not be due to arrhythmia alone Potential deleterious effect of ICD implantation and testing ? Sudden cardiac death after myocardial infarction in patients with type 2 diabetes M. Juhani Junttila, MD, Petra Barthel, MD, Robert J. Myerburg, MD, Timo H. Mäkikallio, MD, Axel Bauer, MD, Kurt Ulm, PhD, Antti Kiviniemi, PhD, Mikko Tulppo, PhD, Juha S. Perkiömäki, MD, Georg Schmidt, MD and Heikki V. Huikuri, MD Heart Rhythm Volume 7, Issue 10, Pages 1396-1403 (October 2010) DOI: 10.1016/j.hrthm.2010.07.031 Sudden cardiac death after myocardial infarction in patients with type 2 diabetes Study population included enrollees in two prospective post-MI studies: Multiple Risk Factor Analysis Trial and Improved Stratification of Autonomic Regulation for Risk Prediction postinfarction survey program. 3276 acute MI patients Diabetic vs Non Diabetic patients: Mean Age 64 vs 59 years, 32 vs 22% females, LVEF 49% vs 52, 3 vs CAD 42 vs 30% Figure 1 Figure 2 Aggregate National Experience With the Wearable Cardioverter-Defibrillator: Event Rates, Compliance, and Survival Chung et al. JACC. 2010;56;194 3,569 patients Indications: ICD explants (23.4%), VT/VF (16.1%), LVEF ≤ 35% with Recent MI (12.5%), Post-CABG (8.9%), Nonischemic CM (20.0%), and LVEF> 35% with recent MI (3.8%) Actual WCD Use Chung, M. K. et al. J Am Coll Cardiol 2010;56:194-203 Copyright ©2010 American College of Cardiology Foundation. Restrictions may apply. Aggregate National Experience With the Wearable Events While Wearing the WCD Cardioverter-Defibrillator Chung, M. K. et al. J Am Coll Cardiol 2010;56:194-203 Copyright ©2010 American College of Cardiology Foundation. Restrictions may apply. Original Article An Entirely Subcutaneous Implantable Cardioverter-Defibrillator Gust H. Bardy, M.D., Warren M. Smith, M.B., Margaret A. Hood, M.B., Ian G. Crozier, M.B., Iain C. Melton, M.B., Luc Jordaens, M.D., Ph.D., Dominic Theuns, Ph.D., Robert E. Park, M.B., David J. Wright, M.D., Derek T. Connelly, M.D., Simon P. Fynn, M.D., Francis D. Murgatroyd, M.D., Johannes Sperzel, M.D., Jörg Neuzner, M.D., Stefan G. Spitzer, M.D., Andrey V. Ardashev, M.D., Ph.D., Amo Oduro, M.B., B.S., Lucas Boersma, M.D., Ph.D., Alexander H. Maass, M.D., Isabelle C. Van Gelder, M.D., Ph.D., Arthur A. Wilde, M.D., Ph.D., Pascal F. van Dessel, M.D., Reinoud E. Knops, M.D., Craig S. Barr, M.B., Pierpaolo Lupo, M.D., Riccardo Cappato, M.D., and Andrew A. Grace, M.B., Ph.D. N Engl J Med Volume 363(1):36-44 July 1, 2010 Locations of the Components of a Subcutaneous Implantable Cardioverter-Defibrillator In Situ Bardy GH et al. N Engl J Med 2010;363:36-44 Chest Radiographs and an Electrocardiogram in a Patient Who Underwent Placement and Testing of a Subcutaneous Implantable Cardioverter-Defibrillator (ICD) Bardy GH et al. N Engl J Med 2010;363:36-44 Cardiac Resynchronization Therapy Case Vignette A 55-year-old man who had had an anterior-wall myocardial infarction six months previously is admitted with an exacerbation of congestive heart failure. An electrocardiogram shows sinus rhythm with a left bundle-branch block; an echocardiogram demonstrates a left ventricular ejection fraction of 25 percent. He is treated with furosemide, lisinopril, and carvedilol. However, during an office visit three months later, he reports persistent shortness of breath with mild exertion. He is referred to a cardiologist, who recommends implantation of a biventricular pacemaker. The Cardiac Conduction System and Biventricular Pacing Jarcho J. N Engl J Med 2006;355:288-294 The Cardiac Conduction System and Biventricular Pacing In patients with a LBBB, conduction of the wave of depolarization in the left ventricle is markedly altered, proceeding from the anterior septum through the left ventricular myocardium to the inferior and lateral left ventricular walls- left ventricular contraction is dyssynchronous, mechanically inefficient with decreases in left ventricular ejection farction and cardiac output. CRT- The Evidence Trial Patients Age (yrs) LVEF MetaAnalysis 1,634 63-66 21-23% 37-69% 158-176 54-87% 23% 65 22% 158 COMPANION 1,520 CAD 56% QRS (ms) LBB 71% MR▼ 24% 1520 patients, NYHA III/ IV, QRS 120 ms, EF 35% RANDOMIZED Optimal medical therapy vs. OMT + cardiac resynchronization pacemaker vs. OMT + cardiac resynchronization defibrillator CRT Indications Class I- EF ≤ 35%, QRS ≥ 0.12 sec, SR, NYHA III/ Ambulatory Class IV + OMTCRT±ICD Class IIA- EF ≤ 35%, QRS ≥ 0.12 sec, AF, NYHA III/ Ambulatory Class IV + OMTCRT±ICD Original Article Cardiac-Resynchronization Therapy for the Prevention of Heart-Failure Events Arthur J. Moss, M.D., W. Jackson Hall, Ph.D., David S. Cannom, M.D., Helmut Klein, M.D., Mary W. Brown, M.S., James P. Daubert, M.D., N.A. Mark Estes, III, M.D., Elyse Foster, M.D., Henry Greenberg, M.D., Steven L. Higgins, M.D., Marc A. Pfeffer, M.D., Ph.D., Scott D. Solomon, M.D., David Wilber, M.D., Wojciech Zareba, M.D., Ph.D., for the MADIT-CRT Trial Investigators N Engl J Med Volume 361(14):1329-1338 October 1, 2009 Kaplan-Meier Estimates of the Probability of Survival Free of Heart Failure Moss AJ et al. N Engl J Med 2009;361:1329-1338 Conclusion CRT combined with ICD decreased the risk of heartfailure events in relatively asymptomatic patients with a low ejection fraction and wide QRS complex MADIT-CRT Editorial- Mariell Jessup, MD CRT benefit solely driven by a 41% reduction in risk of first heart failure event, since mortality not influenced. In CRT trials with symptomatic patients, 29 patients need to be treated for 6 months, 13 patients for 2 years and 9 patients for 3 years to prevent 1 death. MADIT CRT enrolled patients with stage C and NOT stage B (truly asymptomatic). MADIT CRT- treat 12 patients to prevent 1 heart failure hospitalization Cardiac Resynchronization- Effect of Bundle Branch Block Analyzed the results of MADIT-CRT 1820 patients, NYHA I/II, LVEF≤ 30%, QRS ≥130 ms, on optimal medical therapy 1281 LBBB, 228 RBBB, 308 IVCD Hazard ratios for the primary end-point of death or heart failure event were significantly lower in the LBBB patients than in the nonLBBB patient. Zareba et al. JACC 2011 Cardiac Resynchronization In Hypertrophic Obstructive Cardiomyopathy Biventricular pacing was attempted in 12 severely symptomatic HOCM patients and was successful in 9 patients. Functional capacity and QOL improved NYHA class decreased from 3.2±0.4 at baseline to 1.4±0.5 at 1 year with a reduction in the LV gradient from 74±23 mmHg at baseline to 28±17 mmHg at 1 year. Berruezo et al. Heart Rhythm 2011 US Registry of Sudden Death in Athletes Healthy young competitive athletes assembled over 27 years, 1,866 died suddenly (or survived cardiac arrest). Sudden death were due to cardiovascular disease in 56% and 82% occurred with physical exertion. HCM – 36% and congenital coronary anomalies- 17% Pre-participation screening with history, PE and EKG did not impact the rate of sudden death. Maron et al. Circ. 2009;119:1085 US Registry of Sudden Death in Athletes US Registry of Sudden Death in Athletes Pathophysiology of Commotio Cordis Maron B, Estes N. N Engl J Med 2010;362:917-927 Syncope Transient loss of consciousness due to transient global cerebral hypoperfusion characterized by rapid onset, short duration, and spontaneous complete recovery. www.escardio.org/guidelines www.escardio.org/guidelines www.escardio.org/guidelines www.escardio.org/guidelines Original Article Lenient versus Strict Rate Control in Patients with Atrial Fibrillation Isabelle C. Van Gelder, M.D., Hessel F. Groenveld, M.D., Harry J.G.M. Crijns, M.D., Ype S. Tuininga, M.D., Jan G.P. Tijssen, Ph.D., A. Marco Alings, M.D., Hans L. Hillege, M.D., Johanna A. Bergsma-Kadijk, M.Sc., Jan H. Cornel, M.D., Otto Kamp, M.D., Raymond Tukkie, M.D., Hans A. Bosker, M.D., Dirk J. Van Veldhuisen, M.D., Maarten P. Van den Berg, M.D., for the RACE II Investigators N Engl J Med Volume 362(15):1363-1373 April 15, 2010 Study Overview • This clinical trial of outcomes in patients with atrial fibrillation showed that lenient rate control (resting heart rate, <110 beats per minute) was not inferior to strict rate control (resting heart rate, <80 beats per minute) • On the basis of the results, strict rate control may be abandoned as a therapeutic strategy in many patients with permanent atrial fibrillation Cumulative Incidence of the Composite Primary Outcome and Its Components during the 3-Year Follow-up Period, According to Treatment Group Van Gelder IC et al. N Engl J Med 2010;362:1363-1373 Kaplan-Meier Estimates of the Cumulative Incidence of the Primary Outcome, According to Treatment Group Van Gelder IC et al. N Engl J Med 2010;362:1363-1373 Conclusion • In patients with permanent atrial fibrillation, lenient rate control is as effective as strict rate control and is easier to achieve Thromboemblic Risk in Atrial Fibrillation www.escardio.org/guidelines www.escardio.org/guidelines www.escardio.org/guidelines www.escardio.org/guidelines www.escardio.org/guidelines AF guidelines update 2011Dabigatran Class I Dabigatran is useful as an alternative to warfarin for the prevention of stroke and systemic thromboembolism in patients with paroxysmal to persistent AF and risk factors for stroke or systemic embolization who do not have a prosthetic heart valve or hemodynamically significant valve disease, severe renal failure (creatinine clearance < 15 ml/min) or advanced liver disease (impaired baseline clotting function). Level of evidence B www.escardio.org/guidelines Catheter ABlation versus ANtiarrhythmic Drug Therapy in Atrial Fibrillation (CABANA) Trial Mayo Clinic Rochester Duke Clinical Research Institute National Heart Lung and Blood Institute Future of AF--ATRIA Study Projected Number of Adults with AF in the U.S. 7 6 5 Upper scenarios based on sensitivity analyses Lower scenarios based on sensitivity analyses 4 Millions 3 2 1 0 1995 2000 2005 2010 2015 2020 2025 2030 2035 2040 2045 2050 Year Go et al: JAMA 285:2370, 2001 Impact of Atrial Fibrillation on Mortality in Framingham Study 55-74 Years Old 80 Dead (%) 60 Men AF Women AF Men no AF Women no AF 75-94 Years Old 80 60 40 40 20 20 0 0 0 1 2 3 4 5 6 7 8 9 10 Follow-up (yr) Benjamin et al: Circ 98:946, 1998 0 1 2 3 4 5 6 7 8 9 10 Follow-up (yr) CABANA Trial Inclusion Criteria Subjects must meet all of the following criteria • Have documented AF episodes 1 hour in duration; with 2 episodes over 4 months with ECG documentation of 1 episode or at least 1 episode of AF lasting >1 week • Warrant active therapy beyond simple ongoing observation • Be eligible for catheter ablation and 2 sequential rhythm control and/or 3 rate control drugs • Be 65 yr of age, or <65 yr with 1 of the following risk factors for stroke Hypertension Diabetes Congestive heart failure (including systolic or diastolic heart failure) Prior stroke or TIA LA size >5.0 cm (or volume index 40 cc/m2) EF 35 CABANA Trial Primary Objective and Hypothesis The treatment strategy of percutaneous left atrial catheter ablation for the purpose of eliminating atrial fibrillation (AF) is superior to current state-of-the-art medical therapy with either rate control or rhythm control drugs for reducing total mortality (primary endpoint) and decreasing the composite endpoint of total mortality, disabling stroke, serious bleeding, or cardiac arrest (key secondary endpoint) in patients with untreated or incompletely treated AF warranting therapy Design of the CABANA Study Atrial fibrillation Eligible for ablation and/or drug therapy 65 yr of age <65 yr w/ 1 CVA risk factor R Drug Rx & AC • Rate control • Rhythm Rx 1° ablation & AC • PV isolation • Adjunctive Follow-up 60 months Descriptive analysis • NSR vs AF impact • w/ w/o heart disease • AF type – (paroxysmal; persistent; long-standing persistent) • CT/MR image analysis • ECG/EGM analysis CABANA Sites International Approach Canada 10 UK 10 U.S. 90 Asia 5 Australia NZ 5 South Am 5 Europe 30