* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download ILD
Survey
Document related concepts
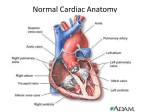
Transcript
Interstitial Lung Disease Organization of Interstitial Lung Disease (ILD) Over 100 separate disorders under the auspices of ILD Organized into subgroups of like disorders Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 2 Pathophysiology Primarily a disease of the interstium Repeated exposure to inflammatory agents or imperfect repair of damaged tissue leads to permanent damage. Increased interstitial tissue replaces normal structures Continuing injury or imperfect repair results in progressive damage and worsening impairment. Physiological impairment due to damage . . V/Q mismatch, shunt, ↓DLCO Increased WoB due to decreased CL These all lead to exercise intolerance. Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 3 Characteristics of ILD Clinical signs and symptoms of ILD • Exertional dyspnea and nonproductive cough Most common reason to seek medical care • May see increased: sputum production, hemoptysis, or wheezing • Nonrespiratory symptoms may help identify presence of connective tissue disorder. Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 4 Characteristics of ILD Physical examination On auscultation Most commonly, bibasilar fine inspiratory crackles In some disorders, will only hear diminished air entry • i.e., sarcoidosis Wheezing is uncommon and probably due to a comorbidity. Signs of right heart failure (late manifestation) Pedal edema, JVD May see features of underlying connective tissue disease Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 5 Characteristics of ILD (cont.) Chest radiographic features Considerable variability dependent on specific disorder Interstitial pulmonary fibrosis (IPF) has what is considered the classic ILD pattern. Reduced volume Bilateral, peripheral, basilar reticulonodular infiltrates End-stage ILD presents with cystic honeycomb lung. IPF is the second most common ILD (sarcoidosis first), and a number of other ILDs present in a similar manner. Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 6 Characteristics of ILD (cont.) Physiological features Restrictive impairment is most common finding. FEV1 and FVC decreased while the FEV1/FVC ratio is normal to increased Lung volumes and DLCO are reduced. CL resulting in small VT and increased WOB Less commonly, patients may have airflow obstruction. May be sarcoidosis or some other mixed disease Comorbidity with asthma or emphysema May result in normal PFTs, but decreased DLCO Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 7 ILD: Exposure Related Asbestos-related pulmonary disease following exposure to asbestos is associated with Pleural plaques, fibrosis, effusions, mesothelioma Atelectasis, parenchymal scarring, lung cancer Termed “asbestosis” if parenchymal fibrosis is present Presents with slowly evolving DOE, inspiratory crackles Shows typical PFTs, while chest radiograph often shows pleural change associated with asbestosis Only supportive therapy is available. Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 8 ILD: Exposure Related (cont.) Chronic silicosis (inhaled silica particles) Exposure: mining, sandblasting, and foundries Chest radiograph shows apical nodular opacities If these coalesce into large masses, it is called progressive massive fibrosis (PMF). If impaired, patients often have a mixed obstructive and restrictive picture with a low DLCO. Silicosis increases the odds of developing tuberculosis and lung cancer. Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 9 ILD: Exposure Related (cont.) Coal worker’s pneumoconiosis (CWP) Used to think due to inhalation of silica, now understood that it is from a distinct exposure Simple CWP asymptomatic, small nodules on radiograph Cough and SoB if progresses to PMF similar to that seen in silicosis No treatment for silicosis or CWP except stop exposure Steroids and 2-agonists for significant airway obstruction Exacerbations treated with steroids and antibiotics Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 10 Chapter 25 Pneumoconiosis Figure 25-1. Pneumoconiosis, illustrated here in a case of asbestosis (close-up of one alveolar unit). AF, Asbestos fiber; FIB, fibrosis; M, macrophage. Inset, Cross-section showing fibrotic thickening of the alveolus, a common secondary anatomic alteration of the lungs. Anatomic Alterations of the Lungs Destruction of the alveoli and adjacent pulmonary capillaries Fibrotic thickening of the respiratory bronchioles, alveolar ducts, and alveoli Cystlike structures (honeycomb appearance) Fibrocalcific pleural plaques (e.g., asbestosis) Airway obstruction caused by inflammation and excessive bronchial secretions Bronchospasm Bronchogenic carcinoma Mesothelioma (in asbestosis) Etiology Etiologic Determinants Size of inhaled particle 0.3 and 0.5 μm reach the alveoli Chemical nature of the particle Concentration of the particle Length of exposure The individual’s susceptibility Etiology Asbestosis Acoustic products Automobile undercoating Brake lining Cements Clutch casings Floor tiles Fire-fighting suits Fireproof paints Insulation Roofing materials Ropes Steam pipe material Etiology Coal Worker’s Pneumoconiosis The deposition and accumulation of large amounts of coal dust cause what is know as coal worker’s pneumoconiosis (CWP) Also called: Coal miner’s lung Black lung Black phthisis Miner’s phthisis Etiology Silicosis Tunneling Hard-rock mining Sandblasting Quarrying Stonecutting Foundry work Ceramics work Abrasive work Brick making Paint making Polishing Stone drilling Well drilling Etiology Berylliosis Beryllium is a steel-gray, lightweight metal found in: Certain plastics and ceramics Rocket fuels X-ray Etiology Other Forms of Pneumoconiosis Aluminum Baritosis (barium) Brick makers and potters Ceramics workers Siderosis (iron) Barite millers and miners Ceramics workers Kaolinosis (clay) Ammunition workers Welders Talcosis (certain talcs) Ceramics workers Plastic and rubber workers Overview of the Cardiopulmonary Clinical Manifestations Associated with PNEUMOCONIOSIS The following clinical manifestations result from the pathophysiologic mechanisms caused (or activated) by Increased Alveolar-Capillary membrane (see Figure 9-9), Bronchospasm (see Figure 9-10), and Excessive Bronchial Secretions (see Figure 9-11)—the major anatomic alterations of the lungs associated with chronic bronchitis (see Figure 25-1). Medications, Drugs, and Radiation Many drugs may cause ILD (see Box 24-1). There is no specific pattern to drug-induced ILD Diagnosis by known exposure to drug, subsequent development of ILD, and other causes are ruled out. Treatment is avoidance of drug, possibly steroids Cancer radiation therapy may result in ILD. Presentation within 6 months with ground-glass appearance on chest radiograph, often responds to short-course steroids Dyspnea presenting after 6 months, have dense fibrotic tissue, can only offer supportive therapy Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 20 Hypersensitivity Pneumonitis (HP) A cell-mediated immune response to inhaled antigens Patients must be sensitized by previous exposure. Acute HP: patient presents with acute SoB, chest pain, fever, chills, malaise, and cough (may be productive) Chronic HP: long-term antigen exposure leads to slow development over months to years Presents with severe impairment that is difficult to distinguish from IPF Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 21 Hypersensitivity Pneumonitis (cont.) Causative agents that can lead to HP Common organic antigens (bacteria and fungi) found in • Moldy hay (farmer’s lung) • Humidification systems (humidifier lung) • Bird feces (bird breeders lung) Inorganic antigens from paints and plastics Treatment Strict antigen identification and avoidance Corticosteroids for symptomatic patients with acute HP • Improves recovery but not lung function Chronic HP results in shorter survival and no known treatment Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 22 Systemic Disease Associated ILD is a complication of various connective tissue diseases, most commonly Scleroderma, rheumatoid arthritis, Sjögren’s syndrome, and systemic lupus erythematosus (SLE) Significant pulmonary impairment prior to detection due to disease imposed sedentary lifestyle Poor correlation between severity and pulmonary and nonpulmonary aspects of these diseases Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 23 Chapter 28 Chronic Interstitial Lung Diseases Figure 28-1. Chronic interstitial lung disease. Inset, Alveolar consolidation, a common secondary anatomic alteration of the lungs. Anatomic Alterations of the Lungs Fibrotic thickening of the respiratory bronchioles, alveolar ducts, and alveoli Granulomas Destruction of the alveoli and adjacent pulmonary capillaries Honeycombing and cavity formation Airway obstruction caused by inflammation and bronchial constriction Etiology More than 140 different disease processes are known to produce an interstitial lung disorder No specific etiologic agent can be identified in more than 65% of the cases In spite of the fact that a specific name may be attached to a particular disease entity Box 28-1 lists some of the more common interstitial lung disorders Box 28-1. Common Interstitial Lung Disorders. Box 28-1. Common Interstitial Lung Disorders, cont. Box 28-1. Common Interstitial Lung Disorders, cont. Table 28-3. Overview of the Cardiopulmonary Clinical Manifestations Associated with CHRONIC INTERSTITIAL LUNG DISEASES The following clinical manifestations result from the pathophysiologic mechanisms caused (or activated) by Increased Alveolar-Capillary Membrane Thickness (see Figure 9-9) and Bronchospasm (see Figure 9-10)—the major anatomic alterations of the lungs associated with chronic interstitial lung disease (see Figure 28-1) Systemic Disease Associated (cont.) Clinical manifestations vary Dyspnea and cough are common. Crackles, wheezes, and pleural rubs may be heard. Typically restrictive disease Depending on disease location, may be obstructive • Sjögren’s disease in particular ⇓DLCO Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 32 Systemic Disease Associated (cont.) HRCT results vary from normal to ground-glass appearance to noting reticular and fibrotic changes. NSIP is associated with ground-glass appearance. OP is associated with patchy consolidation with air bronchograms. UIP is associated with reticular opacities, honeycomb Treatment of systemic inflammatory diseases varies. Most common treatment for acute inflammation or rapid progression is prolonged immunosuppression. Typical agents: • Cyclophosphamide, azathioprine Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 33 Sarcoidosis Most common ILD in United States. Idiopathic multisystem inflammatory disease that forms granulomas in lungs but often follows benign course Most common sign is asymptomatic hilar adenopathy. If symptomatic: cough, chest pain, dyspnea, wheezing Physiology may be normal, restrictive, obstructive, mixed Steroids may be used for sickest symptomatic patients. Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 34 Interstitial Lung Diseases of Unknown Cause Idiopathic interstitial pneumonias (IIP) Most common is IPF, a progressive fibrotic lung disorder Mostly in older patients (>60 years of age) Present with chronic cough and DOE HRCT: bibasilar, peripheral reticular pattern, with cysts Lung biopsy shows UIP and is diagnostic. Most die within 4 years of progressive lung fibrosis. There is no effective treatment. • Oral steroids and azathioprine used but benefit few • Otherwise, supportive therapy Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 35 Idiopathic Interstitial Pneumonias Nonspecific interstitial pneumonia (NSIP) An IIP with diffuse inflammation on surgical lung biopsy most commonly tied to fibrosis forming fibrotic NSIP On average occurs 7–10 years prior to IPF Presents with chronic cough and dsypnea HRCT shows ground glass (NSIP) or fibrotic changes and ground glass (fibrotic NSIP). Prognosis is 7–10 years with immunosuppression (steroids and cytotoxic agents). Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 36 Idiopathic Interstitial Pneumonias (cont.) Cryptogenic organizing pneumonia (COP) Patients are younger than those with IPF A third have an antecedent viral illness. Present with acute or subacute cough and dsypnea HRCT findings typical for acute pneumonia, but patient failed to respond to several courses of antibiotics Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 37 Idiopathic Interstitial Pneumonias (cont.) Cryptogenic organizing pneumonia (COP) (cont.) Most improve with course of oral steroids Number relapse when steroids stopped A few develop progressive fibrosis despite aggressive immunosuppression Can offer lung transplantation Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 38 ILD With Distinct Pathology Lymphangioleiomyomatosis (LAM) Rare, occurs mostly in women Proliferation of smooth muscle around small airways leading to severe obstruction and destruction of alveoli Leads to formation of thin walled cysts Presents with DOE, obstructive impairment, ⇓DLCO Progression from hardly noticeable in older women to steadily progressive for middle-aged women Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 39 ILD With Distinct Pathology (cont.) Lymphangioleiomyomatosis (cont.) Pleurodesis is generally required for recurrent chylothorax Treatment: Inhaled 2-agonists and steroids Younger patients may at some point receive lung transplantation Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 40 ILD With Distinct Pathology (cont.) Pulmonary Langerhans’ cell histiocytosis (PLCH) ILD associated with adult smokers Present with DOE, cough, diffuse inspiratory crackles, airway obstruction, and ⇓DLCO HRCT: central mid-lung star-shaped nodules adjacent to thin-walled cysts Primary treatment: Stop ALL exposure to tobacco smoke If smoke avoidance fails to halt progression, can try • Oral steroids: no proven benefit May offer lung transplantation Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 41 General Management of Chronic Interstitial Lung Diseases Respiratory care treatment protocols Oxygen therapy protocol Aerosolized medication protocol Mechanical ventilation protocol General Management of Chronic Interstitial Lung Diseases Medications and procedures commonly prescribed by the physician Corticosteroids Other agents Cytotoxic agents are used to treat Wegener’s granulomatosis General Management of Chronic Interstitial Lung Diseases Other treatments Plasmapheresis Used to treat Goodpasture’s syndrome • Decreases the circulating anti-GBM antibodies Nonspecific Interstitial Lung Disease Therapies Oxygen therapy Hypoxemia is common in ILD. • Should be evaluated at rest and on exertion O2 via nasal cannula may improve resting hypoxemia and allow greater exertion before desaturation • May improve quality of life and avoid cor pulmonale Pulmonary rehabilitation and exercise therapy Not well studied Encourage for all ILD patients to improve aerobic fitness, maintain activities, improve quality of life Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 45 Nonspecific Interstitial Lung Disease Therapies (cont.) Vaccinations and infection avoidance CDC recommends annual pneumococcal and influenza vaccine. Patient should frequently wash hands. May need pneumocystis prophylaxis if immunocompromised. Transplantation Only therapy shown to prolong life in end-stage ILD Mortality is 10–25% at 1 year and 50–60% at 5 years. Age (>65) and comorbidities often disqualify patients. Mosby items and derived items © 2009 by Mosby, Inc., an affiliate of Elsevier Inc. 46