* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download ADRENAL GLAND Medulla
Survey
Document related concepts
Transcript
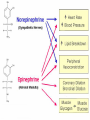
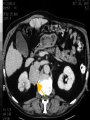
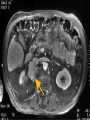
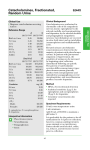
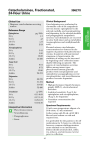
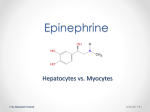
ADRENAL GLAND Medulla Objectives: • Adrenal medulla anatomy and Embryology. • Gross structures, histology, and innervations. • Adrenal medulla hormones: – Synthesis, release, and uptake. – Regulation. – Actions. • Diagnosis of Pheochromocytoma. Embryology of the Adrenal Gland • • • The cortex develops before the medulla. Cortexes develop from coelomic epithelium. (appear in the 6th week) Neural crest cells migrate into the centre of the cortexes to develop the medulla. The cells differentiate in to sympathetic nerve cells. – By the 10th week of fetal life, the adrenal glands show evidence of catecholamine production. – During fetal life, the chromaffine cells secrete only nor-epinephrine but just before birth, some cells begin to synthesize epinephrine. ADRENAL CORTEX Innervations • The principal hormones of the adrenal medulla are catecholamine: – 80 % Epinephrine – 20 % Norepinephrine • Sympathetic nerve (nervous system) endings produce only Norepinephrine. • Each Chromaffine cell is innervated by cholinergic pre-sympathetic neurone, which release acetylcholine. • Synapses are the termination of fibers whose cells bodies lie mainly between T3 and L3 in the spinal cord. Hormonal Synthesis Regulation of synthesis: •First step: through tyrosine hydroxlase (rate-limiting ). –Regulation is under negative feedback by NEpi and Epi. •Last step: conversion from NorEpi to Epi through (Phenylthanolamine N-methyltransferase) –Requires high concentration of glucocorticoids in the central vein of the medulla. Hormonal Release and Regulation. Hormonal Actions. • Alpha 1 (eye, vessels of skeletal muscles, heart ) – Epinephrine, Norepinephrine – Increased free calcium • Vasoconstriction, medriasis, increase bladder sphincter tone • Alpha 2 (CNS, platelets, pancreas and fat cell ) – Epinephrine, Norepinephrine – Decreased cyclic AMP • Inhabit NE. release, and insulin release, increase lipolysis. • Beta 2 (lung, vessels of skeletal muscles, liver ) – Epinephrine – Increase cyclic AMP • Vasodilatation, bronchodilatation, increase glycogenolysis and increase glucagon release. uterine relaxation. • Beta 1 (heart) – Epinephrine, Norepinephrine – Increased cyclic AMP • Tachycardia, and increase myocardial contractility • About 70% of the norepinephrine and epinephrine are conjugated to sulfate (inactive) ?? function. • Normal plasma level of free norepinephrine is about 300 pg/mL (1.8 nmol/L). On standing, the level increases 50-100%. free epinephrine level, is normally about 30 pg/mL (0.16 nmol/L). • The catecholamines half-life is about 2 minutes in the circulation. levels in human venous blood in various physiologic and pathologic states. In each case, the vertical dashed line identifies the threshold plasma concentration at which detectable physiologic changes are observed. (Modified and reproduced, with permission, from Cryer PE: Physiology and pathophysiology of the human sympathoadrenal neuroendocrine system. N Engl J Med 1980;303:436.) Circulatory changes produced in humans by the slow intravenous infusion Hormonal Uptake Fate of Catecholamine • Uptake-1 “mainly Norepinephrine” – (post-ganglionic sympathetic nerve terminals) – De-aminated by monoamine oxidase in mitochondria then enters to the vesicle (store). – Become available for re-use. – Sites of drug action (e.g.. cocaine and antidepressants) • Uptake-2 “Mainly Epinephrine” – (non-neuronal tissues) – Inactivated by O-methylation by catechol-O- methyl transferase (COMT) – Metpolised to inactive end-products mainly metanephrine and normetanephrine and VMA. Secreted Catecholamines (urine) • 50% appear in the urine as free or conjugated metanephrine and normetanephrine. • 35% as VMA. • Small amounts of free norepinephrine and epinephrine. • After adrenalectomy – The plasma norepinephrine level is generally unchanged. – Free epinephrine level, falls to essentially zero. • Adrenal medulla failure: – Hypoglycemia and hypotension. – Hormones of the cortex are way more important in this regard. – No need to replace adrenal medulla hormones. PHEOCHROMOCYTOMA DIAGNOSIS Clinical presentation Pheochromocytoma • Usually suggested by: – Symptoms: • Classic triad episodic headache (90%), sweating (60%), and tachycardia, paroxysmal hypertension (50%). – Incidental adrenal mass: – Family history in a patient with familial disease: • MEN 2A: pheo. (B/L), medullary carcinoma of the thyroid (MTC), primary parathyroid hyperplasia. • MEN 2B: pheo. (B/L), MTC, mucosal neuromas, thickened corneal nerves, intestinal ganglio-neuromatosis, and marfanoid body. • von Hippel-Lindau disease: pheo.(B/L) paraganglioma, retinal angiomas, cerebellar hemangioblastoma, epididymal cystadenoma, renal and pancreatic cysts, and renal cell carcinoma. Diagnosis of Pheochromocytoma • Among patients suspected to have Pheochromocytoma, the diagnosis is rarely confirmed. – Diagnosis confirmed in 1 of 300 patients evaluated for pheochromocytoma • Fogarty, J, Engel, C, Russo, J, et al. Hypertension and pheochromocytoma testing: The association with anxiety disorders. Arch Fam Med 1994; 3:55. • Methods of evaluation: 1. Biochemical evaluation. 2. Radiological evaluation. Biochemical evaluation • Interferences with plasma/urine catecholamine measurements – False increase: • Alpha1 blocker, beta-blocker, vasodilators “Hydralazine, Nitro, Minoxidile”, CCB (short term), Methyldopa. Phenothiazin. • Tricyclic antidepressants, psychoactive agents, nicotine, Amphetamine. • Theophylline & Aminophylline, Epinephrine & epinephrine like drugs “nasal drops, cough and sinus medications. • Ampicillin, Quinidine, Tetracycline. • Vit. B complex, withdrawal (Etoh and clonidine). – False decrease: • ASA, alpha 2 agonist, bromocriptine, CCB (long term), cimetidine, clonidine, delay in the separation of RBCs from plasma(5 min) Avoid medications for at least 2 weeks before the test Multi-center cohort study in Netherlands that included 214 patients with confirmed pheochromocytoma and 644 patients who were not . Test performed Sensitivity Specificity Fractionated plasma free 99 % metanephrines 89 % Urinary fractionated metanephrines 97 % 69 % Urinary catecholamines 86 % 88 % Plasma catecholamines 84 % 81 % Urinary total metanephrines 77 % 93 % Urinary VMA 64 % 95 % Lenders JW; Pacak K; Walther MM; Linehan WM; Mannelli M; Friberg P; Keiser HR; Goldstein DS; Eisenhofer G SOJAMA 2002 Mar 20;287(11):1427-34. 349 patients tested for pheochromocytoma at Mayo Clinic Rochester from January 1, 1999, until November 27, 2000. “tumors were histologically proven ” Fractionated plasma metanephrine 24-hr urinary metanephrines (metanephrine+normetanephri ne) in combination with urinary catecholamines Sensitivity 97 % 90 % Specificity 85 % 96 % likelihood ratio for a positive test 6.3 58.9 likelihood ratios for a negative test 0.04 0.10 Sawka AM; Jaeschke R; Singh RJ; Young WF Jr SOJ Clin Endocrinol Metab 2003 Feb;88(2):553-8 Systematic review and meta-analysis from Hamilton, Ontario, of Fractionated plasma free metanephrines including 3 studies of 56 patients with and 445 subjects without pheochromocytoma Sensitivity 97 to 100 % Specificity 82 to 100 % Positive likelihood ratio 5.77 Negative likelihood ratio 0.02 Very useful to rule out pheochromocytoma Sawka AM; Prebtani AP; Thabane L; Gafni A; Levine M; Young WF Jr SOBMC Endocr Disord. 2004 Jun 29;4(1):2. Normal values • Urine Catecholamines (measured by HPLC) – Norepinephrine (15-80 micrograms/day) – Epinephrine (0-20 micrograms/day) • Urine Deconjugated Fractionated Metanephrines (measured by HPLC) – Normetanephrine-sulfate (44-540 micrograms/day) – Metanephrine-sulfate (26-230 micrograms/day) • • • Urine Deconjugated Total Metanephrines (measured by Spectrofluorimetry) (0-1.2 milligrams/day) (Sum of free plus sulfate conjugated metanephrine & normetanephrine) Urine VMA (measured by Spectrofluorimetry) (0-7.9 milligrams/day) Plasma Catecholamines (measured by HPLC) – Norepinephrine (80-498 picograms/milliliter) – Epinephrine (4-83 picograms/milliliter) • Plasma Free Metanephrines (measured by HPLC) – Normetanephrine (18-112 picograms/milliliter) – Metanephrine (12-61 picograms/milliliter) • Plasma Deconjugated Metanephrines (measured by HPLC) – Normetanephrine-sulfate (610-3170 picograms/milliliter) – Metanephrine-sulfate (316-1706 picograms/milliliter) • Clonidine suppression test : – Suppresses the release of catecholamines from neurons but not from pheochromocytoma tissues. – 0.3 mg PO, then plasma catecholamines or/and metanephrines are measured before and 3 hours after . • Plasma catecholamine concentrations decrease by >50 %. • Plasma normetanephrine decrease by >40 %. Suggest Essential HTN. • If remain increased suggest pheochromocytoma. – The test is 92 % accurate • Sjoberg RJ; Simcic KJ; Kidd GS Arch Intern Med 1992 Jun;152(6):1193-7. • Eisenhofer G; Goldstein DS; Walther MM; Friberg P; Lenders JW; Keiser HR; Pacak K J Clin Endocrinol Metab 2003 Jun;88(6):2656-66. What I am going to order • Fractionated plasma free metanephrines. • 24-hr urinary metanephrines, urinary catecholamines and Urinary VMA. Radiological evaluation • About 10 percent of the tumors are extra-adrenal, and 95 % are within the abdomen and pelvis. – Bravo EL Endocr Rev 1994 Jun;15(3):356-68. • Abdominal paraaortic areas (75 %), the urinary bladder (10 %), the thorax (10 %), and the head, neck, and pelvis (5 %) – Whalen RK; Althausen AF; Daniels GH J Urol 1992 Jan;147(1):1-10. CT Scan MRI Radiation exposure High None risk of exacerbate HTN due to contrast agent High “can be prevented by pretreatment with alpha-adrenergic blockade” None Expense less more Distinguish Unable to differentiate pheochromocytoma from other adrenal masses 1. 2. pheochromocytomas appear hyperintense and other adrenal tumors isointense, as compared with the liver Both have high sensitivity (98 to 100 %), but are only about 70 percent Low specificity (70%) ?adrenal "incidentalomas." Radiological evaluation • 123-I-metaiodobenzylguanidine “MIBG” scan: – If CT or MRI is negative in the presence of clinical and biochemical evidence of pheochromocytoma, – Multiple tumors when CT or MRI is positive. • Octreoscan, total body MRI, and PET scanning: – Detect a tumor in an unusual location (heart) when the other techniques have failed. • Positron emission tomography (PET) scan: – Identifying sites of metastatic disease. THANKS