* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Case Study: Failure to Thrive
Quantium Medical Cardiac Output wikipedia , lookup
Myocardial infarction wikipedia , lookup
Drug-eluting stent wikipedia , lookup
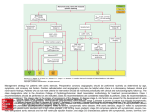
Management of acute coronary syndrome wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
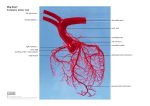
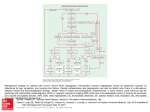
Aortic Stenosis Clinical Case Study Ema Thake University of Utah June 8, 2012 Aortic Stenosis As the aortic valve becomes more narrow, the pressure increases inside the left heart ventricle. causes the left heart ventricle to become thicker, decreasing blood flow Can lead to chest pain and shortness of breath. Severe forms of aortic stenosis prevent enough blood from reaching the brain and rest of the body. This can cause light-headedness and fainting Aortic Stenosis. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001230/ Aortic Stenosis Symptoms Breathlessness Chest pain Fainting, dizziness Treatment Stop smoking Treatment for high cholesterol Surgery to replace or repair the valve Medications Diuretics Nitrates Beta blockers Patient GH 71 year old male Admitting diagnosis: for pre-op consultation for Aortic stenosis with aortic root dilation and ascending aorta dilation, with coronary artery disease On admit: Wt: 113.2 kg; Height: 173 cm BMI: 37.82 (obese – grade II) Extensive medical history Medical/Nutritional History PAST MEDICAL HISTORY: Aortic stenosis with bicuspid aortic valve. Aortic root and ascending aorta dilation Coronary artery disease, status post CABG in 2001 Type 2 diabetes, non-insulin dependent. COPD Hypertension Hyperlipidemia Renal insufficiency Lung disease The patient complains of irregular heartbeats or palpitation Peripheral vascular disease Obstructive sleep apnea, for which he does not use a CPAP machine GERD Osteoarthritis in his shoulders Chronic low back pain, status post fusion. Pancreatitis Non-union of his sternum with broken sternal wires Medical/Nutrition History PAST SURGICAL HISTORY: Coronary artery bypass grafts in 2001 Angioplasty x 3 with stents to his circumflex Cholecystectomy Right knee surgery Lower back fusions in 1999 Medical/Nutrition History FAMILY HISTORY: Significant for coronary artery disease. Father died from an MI at the age of 52. The patient has 3 brothers, who have had coronary artery bypass grafts in the past. Another sister had coronary disease, who is now deceased. SOCIAL HISTORY: The patient reports approximately 50-pack-year smoking history. The patient quit 1-1/2 years ago. The patient quit using alcohol 2 years ago and denies any drug history. The patient is married, lives with his wife in Green River, Wyoming and is retired. Anthropometrics Biochemical Piper and Kaplan, 2012 Medications Furosemide Atorvastatin Metaprolol Metformin Omeprazole Warfarin Sitagliptin Potassium Chloride Clinical No apparent skin breakdown Edema on legs caused some broken skin No pressure ulcers Swallowing Evaluations POD #12 - First attempt failed by patient POD #19 – Passed eval., advanced to dysphagia 3 diet Nutrition Diagnosis Inadequate oral intake related to intubation and sedation as evidenced by need for nutrition support. Obesity as evidenced by BMI 37.82. Nutrition Intervention DHT placed 5/6 – trophic feeds 5/7 – Promote @ 75 ml/hr 5/10 – Promote @ 90 ml/hr 5/15 – DHT accidentally pulled out 5/16 – Promote @ 25 ml/hr after DHT replacement 5/18 – Promote @ 90 ml/hr – resp. failure, intubated again 5/19 – Promote @ 40 ml/hr 5/20 – Promote @ 75 ml/hr – IDC indicated underfeeding 5/25 – DHT accidentally pulled out, diet advanced to dysphagia 3 Nutrition Intervention Tube feed initiated - Promote Adjusted based on needs Estimated needs and IDC 2025-2430 kcal/day (25-30 kcal/kg AdjBW) 97-122 g protein/day (1.2-1.5 g/kg AdjBW) SLP evaluation Advanced diet Monitoring & Evaluation IDC to monitor adequacy of the tube feeds Calorie counts to assess oral intake when diet was advanced Notes Percentage of meals eaten Reflection/Personal Assessment I had the opportunity to assist in the placement of a DHT in this patient. I found that experience to be very valuable. It was good to see the patient through each stage of recovery. Would have liked to gain more information about the education he received for discharge diet. Questions? References Svagzdiene M, Sirvinskas E, Benetis R, Raliene L, Simatoniene V. Atrial fibrillation and changes in serum and urinary electrolyte levels after coronary artery bypass grafting surgery. Medicina (Kaunas). 2009;45(12):960-70. Piper GL, Kaplan LJ. Fluid and electrolyte management for the surgical patient. Surg Clin North Am. 2012 Apr;92(2):189-205, vii. Epub 2012 Feb 9 Atrial Fibrillation/Flutter. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001236/ Aortic Stenosis. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001230/