* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Blood histology Dr. Anshu Kacker
Cell culture wikipedia , lookup
Cell theory wikipedia , lookup
List of types of proteins wikipedia , lookup
Regeneration in humans wikipedia , lookup
Organ-on-a-chip wikipedia , lookup
Human embryogenesis wikipedia , lookup
Hematopoietic stem cell transplantation wikipedia , lookup
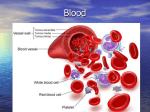
Hematopoietic stem cell wikipedia , lookup
Developmental biology wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
BLOOD 1 Functions • Transportation: – Dissolved or chemically bound matter (O2, CO2, nutrients, metabolites) – Maintenance of the body temperature • Regulation: – Transmission of signals (hormones) – Maintenance of homeostasis • Concentration of dissolved substances • Osmotic and oncotic pressure • Acid-base balance - buffering the body fluids (maintenance of pH) • Protection: – Defense against foreign agents (specific and non-specific immunity) – Prevention of hemorrhage – Hemostasis. 2 Composition of the blood • Blood is a specialized C.T. composed of an extracellular matrix (ECM) called plasma, and formed elements (blood cells and platelets). • Blood plasma (55%) - noncellular portion of the blood. • Formed elements (45%) – Red blood cells (erythrocytes) – Platelets (thrombocytes) – White blood cells (leukocytes) 3 Hematocrit (PCV) • • • • Is the fraction of the blood volume made up of the formed elements (mainly RBC). Is determined by the centrifuging heparinised blood ( blood mixed with anticoagulant) in a standard calibrated tube of a small diameter. After centrifugation the column of the RBCs and plasma can be measured. Three layers are seen: – Supernatant plasma – Buffy coat – leukocytes and platelets – RBC 4 Hematocrit (PCV) • Values: The hematocrit is measure of the percent of RBC’s in blood. – Males: 40 – 54 vol% – Females: 38 – 46 vol% • ↑ in persons living at high altitudes, in dehydrated state, polycythemia etc. • ↓ in anemia, leukemia, bone marrow failure • Importance: – Determines blood viscosity. – ↑ Htc → ↑ resistance to blood flow. 5 Plasma • Plasma is the liquid part of blood that remains after the cells have been removed, but which still contains clotting elements. • Serum is blood from which the cells and clotting elements have been removed. • Serum = Plasma - Clotting factors 6 Plasma protein • Plasma is a pale-yellow fluid containing 90% water, 9% organic compounds (proteins, hormones etc), & 1% inorganic salts. Its principal proteins are: – Albumin: most abundant plasma protein; responsible for 80% of the total osmotic pressure of the plasma; synthesized in the liver. – Globulins: • Alpha globulins: transport bilirubin and steroids. • Beta globulins: transport iron and copper. • Gamma-globulins: these are immunoglobulins, or antibodies, synthesized by plasma cells. – Fibrinogens: synthesized in the liver; act in blood-clotting; responsible for most of the viscosity of plasma. – Complement proteins: Coagulation (blood clotting) is a cascade of chemical reactions mediated by complement proteins, resulting in the conversion of fibrinogen into fibrin. 7 Albumin • Albumin have the smallest molecular mass whereas fibrinogen is the largest. • Albumin is the serum protein responsible for the maintenance of colloid osmotic pressure. • A decrease in osmotic pressure can result from increased protein loss or decreased protein synthesis. • Increased albumin Loss: – Nephrotic Syndrome • Reduced albumin synthesis: – Cirrhosis – Protein malnutrition 8 II. Formed Elements • Blood cells are produced and replaced in blood-forming organs (mostly bone marrow, in the adult), do not develop or replicate in the circulation, and have a limited lifespan. • RBCs and platelets function within the blood vasculature. • With the exception of the basophil, WBCs exit the vessels and exert their effects within body tissues. • The normal proportion of each type of blood cell lies within narrow limits, as determined by a “Complete Blood Count (CBC)”. • “Differential leukocyte count" values will help to identify specific white cell types in blood and in tissues. 9 Blood composition: Formed elements Platelets Erythrocytes 10 Red blood cells • Red cells are uniform in size and shape with an average diameter of 7.2 to 7.9 µm. • Erythrocytes are anucleate (i.e. no nucleus), uniformly acidophilic bi-concave. • No mitosis, & No organelle. • Normal RBC should be the size of a mature lymphocyte nucleus. • Life span - 120 days. 11 Peripheral blood smear 12 Biconcave shape of erythrocytes • RBC shape is maintained by a subplasmalemma cytoskeleton (spectrin, actin, and band 4.1 protein) that is connected to the lipid bilayer by ankyrin. • Ankyrin is linked to both band 3 proteins and spectrin tetramers, thus attaching the spectrin-actin complex to transmembrane proteins. • Within the bilayer are various integral proteins, such as glycophorins, ion channels, and band 3 protein. 13 RBC cytoskeleton • The biconcave shape provides erythrocytes with a large surface-to-volume ratio, thus facilitating gas exchange. • Shape, along with the fluidity of the plasma membrane, allows the erythrocyte to deform readily, and are able to pass through the smallest capillaries. • The cytoskeleton of nonerythroid cells consists of Actin, alfa-Actinin and Vinculin. 14 Hereditary spherocytosis • • • • Mutation in spectrin that renders the protein incapable of binding to band 4.1 protein, thus destabilizing the spectrin-actin complex of the cytoskeleton. Such RBC adopt a spherical shape and are osmotically fragile. In a blood smear, the affected cells lack the pale area in the center because they are spherical. These fragile cells are prone to rupture, leading to anemia Spleen is the principal site for the removal of worn-out rbcs, individuals with spherocytosis show splenomegaly. 15 Hereditary elliptocytosis • Deficiency in band 4.1 proteins results in elliptical erythrocytes. • Erythrocytes are unable to adapt to changes in their environment (e.g., osmotic pressure and mechanical deformations), which results in premature destruction of the cells, or hemolysis. 16 Reticulocytes • Reticulocytes are immature red blood cells still retain residual nuclear material, few mitochondria & Golgi complex. • Less than 1% of circulating red blood cells. • Stain with basic dyes cytoplasm shows blue precipitates. • Increase proportion of reticulocytes in the bloodstream. – hemorrhage – exposure to high altitudes – bone marrow pathology 17 White blood cells • Five types of leucocytes are normally present in the circulation. • These are divided into two main groups based on their nuclear shape and cytoplasmic granules. • Within the C.T. they act in cellular and humoral immune responses to foreign agents. • On the basis of the presence and type of granule in their cytoplasm and the shape of the nucleus, white blood cells are classified into two groups: – Granulocytes – Agranulocytes 18 Peripheral blood cells A. Erythrocytes; B. Large Granular Lymphocyte; C. Neutrophil; D. Eosinophil; E. Neutrophil; F. Monocyte; G. Platelets; H. Lymphocyte; I. Band Neutrophil; J. Basophil 19 • Granulocytes - these cells have multilobulated nuclei and contain primary and secondary (specific granules). – Neutrophils (polymorphs) – Eosinophils – Basophils • Agranulocytes (Mononuclear leucocytes) these cells have non-lobulated nuclei and contain primary or azurophil granules. Agranulocytes do not have specific granules. – Lymphocytes and Monocytes. 20 Differential leucocyte count • In general, leucocytes number between 6,000 and 10,000 cells/mm3 in blood. • In an acute infection (as for example, appendicitis), the cell number may rise to 20,000 or 40,000/mm3. • The relative proportion of leucocytes in the blood (differential count) is usually constant within an individual: – Neutrophils (50%-70%) of total leukocytes – Lymphocytes (20%-30%) – Monocytes (3%-8%) – Eosinophils (2%-4%) – Basophils (0-1%) 21 White Blood Cells 22 Neutrophils • These cells constitute 50–70% of circulating leucocytes. • The cytoplasm of a neutrophil contains three kinds of granules, reflect the various phagocytotic functions of the cell. • They are 12–15 mm in diameter, with a nucleus consisting of 2–5 (usually 3) lobes linked by fine threads of chromatin. • Neutrophils with more than five lobes are called hypersegmented (in Vitamin B12 or folate deficiency). 23 Neutrophil granules • Primary (azurophilic) granules 1. Myeloperoxidase 2. Phospholipase A2 3. Lysozyme 4. Acid hydrolases 5. Elastase 6. Defensins 7. Bacterial permeability increasing protein (BPI) • Secondary (specific) granules 1. Phospholipase A2 2. Lysozyme, 3. NADPH oxidase 4. Leukocyte alkaline phosphatase (LAP) 5. Collagenase 6. Lactoferrin • Tertiary granules: – Phosphatases and metalloproteinases (gelatinases & collagenases) 24 Band Neutrophil • • Juvenile neutrophils Non-lobulated nucleus 25 Functions • Under normal conditions, 90% of the neutrophils are in the bone marrow, 2–3 % are circulating and the rest are in the tissues. • Neutrophils to survive in an anaerobic environment is highly advantageous, since they can kill bacteria and help clean up debris in poorly oxygenated regions, eg, inflamed or necrotic tissue. • Neutrophils constitute a defense against invasion by micro organisms, especially bacteria. • Dead neutrophils, bacteria, and semi digested material form a viscous, usually yellow collection of fluid called pus. 26 Eosinophils • Eosinophils constituting only 2–4% of leukocytes in normal blood. • Diameter of 12–15 mm and contains a characteristic bilobed nucleus. • Azurophilic granules are lysosomes, contain lysosomal acid hydrolases and hydrolytic enzymes that function in destruction of parasites and hydrolysis of antigen–antibody complexes internalized by the eosinophil. 27 Eosinophils (specific granules) • Specific granules of eosinophils contain a crystalloid body. • Crystalloid body contain four major proteins: 1. Major basic protein (MBP), for the intense acidophilia of the granule. MBP is localized in the crystalloid body. 2. Eosinophil cationic protein (ECP) 3. Eosinophil peroxidase (EPO) and 4. Eosinophil-derived neurotoxin (EDN) • MBP, ECP, and EPO have a cytotoxic effect on protozoans and helminthic parasites. • EDN causes nervous system dysfunction in parasitic organisms. 28 Eosinophil 29 Functions • Phagocytosis of antigen/antibody complexes in asthma, hay fever and other allergies. • Destruction of invading parasites - their numbers rise sharply during allergic reactions or parasitic infections. Eosinophils are activated by interactions with IgG, IgA, antibodies and have receptors for IgE, which is important for destruction of parasite. • Counteracting the effects of basophils - eosinophils produce substances that break down products released by basophils: – Histaminase - anti-histamine – Arylsulfatase (which neutralizes leukotrienes secreted by basophils and mast cells ) 30 Basophils • Less than 1% of blood leukocytes. • They have bilobed nucleus but this is usually obscured by numerous densely basophilic (deep blue) specific granules. • Structural and functional similarities with tissue mast cells. 31 Basophil • Heterochromatin is in a peripheral location, and euchromatin is centrally located • The basophil plasma membrane possesses numerous high-affinity Fc receptors for IgE antibodies. Electron micrograph and Light microscopic appearance of a basophil 32 Basophil function • Basophils participate in certain specific types of immune reactions because they have surface receptors for IgE. When activated, they release their vasoactive substances. • The basophil's specific granules contain: – Heparin, a powerful anticoagulant. – Histamine, which quickly and drastically increases the permeability of blood vessels, causes vasodilation, and causes smooth muscle contraction in bronchi. – Leukotrienes or Slow-Reacting Substance of Anaphylaxis (SRS-A), for the slow, sustained contraction of smooth muscle. 33 Lymphocytes • Lymphocytes are the smallest cells in the white cell series, being only slightly larger than erythrocytes. • They are the second most common leucocytes in circulating blood and make up 20-50% of the differential white cell count. • Lymphocytes are characterized by a round, densely stained nucleus and a small amount of pale basophilic, non-granular cytoplasm. 34 Lymphocytes • The amount of cytoplasm depends upon the state of activity of the lymphocyte, and in circulating blood there is a predominance of 'small' inactive lymphocytes (6-9 μm in diameter). • 'Large' lymphocytes (9-15 μm in diameter) make up about 3% of lymphocytes in peripheral blood. • Large lymphocytes represent activated B or T lymphocytes. ONLY cells that leave and re enter circulation. 35 Lymphocytes 36 Types of lymphocytes 37 Types of lymphocytes • T cells: – Th (T helper) cells: activate and regulate T and B cells. – CD8+ cytotoxic T cells: virus-infected and tumor cells. – Regulatory (suppressor) T cells: Returns the functioning of the immune system to normal after infection; prevents autoimmunity. • B cells: – Precedes plasma cells and releases antibodies. • Natural killer cells: acts on virus-infected and tumor cells. 38 Monocytes • Monocytes are the largest of the white cells (up to 20 μm in diameter) and constitute from 2 to 10% of leucocytes in peripheral blood. • They are motile phagocytic cells and are the precursors of macrophages found in peripheral tissues and organs. • Monocytes are characterized by a large, eccentrically placed nucleus; nuclear indentation tends to become more pronounced as the cell matures, so as to give a kidney shape appearance. • Cytoplasm stains pale greyish blue, contains numerous small purple stained lysosomal granules and cytoplasmic vacuoles which gives a 'frosted-glass' appearance. 39 Monocyte 40 Monocyte • Monocytes migrate to peripheral tissues where they assume the role of macrophages. • Monocyte-macrophage system (mononuclear phagocyte system), consisting of circulating monocytes, their bone marrow precursors, and tissue macrophages both free and fixed (histiocytes). • Monocytes respond by chemotaxis to the presence of factors from damaged tissue, microorganisms and inflammation by migration into the tissues and differentiation into macrophages; with their capacity for phagocytosis. 41 Platelets • Blood platelets (thrombocytes) are nonnucleated, disk like cell fragments 2–4 mm in diameter that participate in clot formation. • Platelets arise from megakaryocytes, extremely large cells that are found in the bone marrow. • Megakaryocytes have a single, large, highly lobulated nucleus. They arise in turn from megakaryoblasts by the process of endomitosis, in which nuclear division occurs without cytoplasmic division and the nucleus will become polyploid. • In stained blood smears, platelets appear in clumps. 42 Hyalomere and Granulomere region • The hyalomere contains actin and myosin, which enable the platelets to contract. • The granulomere contains three types of granules ( α, δ, λ ) – 1. The alfa (α ) granules contain factors that are involved in repair of blood vessels, aggregation of platelets, and coagulation of blood. • These factors include fibrinogen, platelet-derived growth factor, platelet thromboplastin, and coagulation factors V and VIII. – 2. Dense (δ) bodies contain factors that are involved in vasoconstriction, platelet aggregation, and platelet adhesion. These factors include ADP, ATP, ionized calcium, histamine, epinephrine, and serotonin storage (produced mostly by enteroendocrine cells of the gut). – 3. The λ granules contain lysosomal enzymes, participate in the removal of blood clots. 43 Platelets 44 Platelets 45 Platelet function • Platelets play a crucial role in blood clotting (coagulation). – Maintenance of vascular integrity. Upon activation, they are able to increase their surface area by severalhundred fold . This enables them to spread across gaps torn in the endothelium and to stick to endothelial walls, temporarily sealing leaks in vessels until the tissue can regenerate . – Release of blood clotting factors. – Clot retraction and dissolution. 46 Complete Blood Count • Screens for anemia and infection • Total RBC, WBC & platelet counts; differential WBC; hematocrit and hemoglobin measurements • Normal hemoglobin range – infants have 14 to 20 g/100mL of blood – adult females have 12 to 16 g/100mL of blood – adult males have 13.5 to 18g/100mL of blood White cell count in disease • Raised neutrophil count (neutrophilia) indicates an acute inflammatory response and is seen in bacterial infections. • Raised eosinophil count (eosinophilia) is seen in response to allergy and in infections with certain parasites. • Raised lymphocyte count (lymphocytosis) is seen in response to viral infections. • Malignant tumors can form from the bone marrow cells that make white blood cells, termed leukaemias. In these conditions it is common to find a very raised white cell count corresponding to circulating malignant cells. • Reduction in white cells in the blood may indicate defective function of the bone marrow. 48 49 Anemia • Low RBC count, • Decreased hemoglobin in peripheral blood • Etiology: – Loss of blood (hemorrhage) – Insufficient production • Lack of iron, vitamin B12 – Increased destruction due to intrinsic factors – Hemolytic Anemia 50 Anemia • Results in: – ↓ oxygen-carrying capacity of the blood → hypoxia → vasodilation – ↑ in pulse and respiratory rates (effort to supply sufficient oxygen to tissues) – ↓ exercise & cold tolerance – Pale skin (↓ red colored oxy Hb) – ↑ fatigue and lassitude (lack of energy) – ↓ blood viscosity → ↓ peripheral resistance → ↑ blood flow, venous return and CO and work load on the heart • Etiological classification: – – – – Nutritional Aplastic Hemorrhagic Hemolytic 51 Clinical features • Symptoms: – Tiredness – Easy fatiguability – Generalized muscular weakness – Lethargy – Headache • Signs: – – – – – Pallor Retinal hemorrhages Menstrual disturbances Mild proteinuria Anorexia, flatulance 52 53