* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Slide 1
Survey
Document related concepts
Transcript
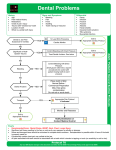
HEENT Review October 1, 2008 Nick Genes the inservice exam • • • • Feb 25, 2009 Short term $$$ (moonlighting, Mets) Long term $$$$$$ (licensure, career in EM) But also: intro to EM practice • Similar questions to ABEM • Last year: 207 questions counted • Physician’s Evaluation and Educational Review VII • Las Vegas Board Review Course MP3s (2003?) This lecture series • Board review: Five months, 20 lectures… • Different than Dr. Cherkas sessions • • • • • This year: More engagement than 2005-6 More questions, buzzwords than last year More repetition More candy HEENT • 21 questions in PEER VII (out of 410, 5%) • Some overlap in ID, Trauma, Procedures, S&S • Last year’s inservice: it was 10 out of 207 • CV, GI, Pulm, Trauma each ~20 • Likely emphasis: details that make or break ED diagnosis or management HEENT • Today: H and T, then N, then E, then E. • No evidence, no nuance. – I would love to spend 20 minutes talking about preseptal cellulitis vs. orbital cellulitis – Sorry Question 1 A 32-year-old man presents 30 minutes after getting a tooth knocked out in a fight. On examination, a small clot in the socket is noted. The next step in management is: a) Call the patient’s dentist • They’re too slow b) Clean the tooth with a brush • No brush! Worry about the dental ligament c) Gently irrigate the socket • To remove the clot to let the tooth reconnect d) Immediately replace the tooth • Sure… after clot removed e) Tell the patient the tooth cannot be reimplanted • Not true… Tooth Avulsion • Tooth completely removed from the socket • Permanent teeth avulsed for less than 3 hours can be reimplanted – – – – Rinse tooth with Hank’s solution, sterile saline, or milk Irrigate socket with sterile NS prior to reimplantation Emergent Dental Consult Do NOT scrub tooth Tooth Avulsion • What if the tooth is missing? – You need films to rule out aspiration • What if this is a four year old? – Primary teeth in children should not be replaced Tooth Avulsion • Replant permanent teeth quickly – 1% loss of survival per minute – Early, improper reimplantation is better than waiting for OMFS • Rinse first, no scrubbing (injures periodontal ligament). Handle only the crown • Transport / storage media = saliva, sterile saline, or milk. Hank’s solution is best • Only permanent teeth need replantaion – reimplantation of “baby” teeth can result in bone fusion and prevent permanent teeth eruption Tooth Fractures enamel dentin Ellis I Ellis II Ellis III pulp horizontal fx • Ellis II and III fractures require covering of exposed dentin or pulp and <24h referral to a dentist • “if you see pink, send ‘em” • May refer Ellis I for cosmesis Alveolar Osteitis (dry socket) • 2-5 days post-extraction • “The clot got lost, bugs got in” • Severe pain due to exposed alveolar bone and a localized osteomyelitis as the result of protective clot displacement • Risk factors: – Females on HRT, pre-existing gum and tooth infections, traumatic extraction, impacted third molar extractions (2035%) • Treatment: – Anesthetize, irrigate socket, pack with iodoform gauze + eugenol, Antibiotics, early referral Dental Abscesses • I don’t think there’s testable material here… no gamechanging tricks in management Periapical Abscess Question 2 A 25-year-old man presents with mouth pain and bleeding gums. He does not recall any medical problems but says he is homeless. He is afebrile without systemic symptoms. Which of the following is an ineffective component of treatment? a) Acyclovir • Because this isn’t massive herpes outbreak, no vesicles b) Chlorhexidine oral rinses c) Debridement d) Diet rich in proteins and vitamins e) Metronidazole Q2 -- Trench Mouth (ANUG) Diagnosis is based on three symptoms/signs: • Pain • ulcerations between teeth • gingival bleeding • Also smell, loose teeth, fever. • Poor hygiene, HIV. • Anaerobes. • Treat with chlorhexidine oral rinses, metronidazole. • Debridement may be necessary • Diet rich in proteins and vitamins will prevent Question 3 A 50-year-old man presents with fever and pain on swallowing. Examination reveals a nontoxic man with neck swelling, tongue elevation, and trismus. The most likely diagnosis is: a) b) c) d) e) Epiglottitis • 2-3d of throat pain, fever, can’t see it Exudative pharyngitis • can see it, also cervical LA Ludwig angina • bilateral tongue base infection, swelling… deadly Peritonsillar abscess • assymmetry, hot potato voice Pharyngeal tumor PEER VII Q223 • no fever Q3 -- Ludwig’s Angina • Bilateral cellulitis of the submandibular space • Painful edema of submandibular area • Involves connective tissue, fascia and muscle • Dental source most common (abscess, trauma, recent extraction). Mixed aerobic / anaerobic • Contrast CT is diagnostic, aids surgical mgmt • Can progress to restricted neck motion, trismus, dysphonia, posterior tongue displacement, airway compromise (drooling, stridor suggest doom) • May need fiberoptic for airway control • If that fails, cricothyroidotomy Ludwig Angina Epiglottitis • • • • Now more common in adults than children Severe sore throat with normal oropharynx exam Pain on moving thyroid cartilage, out of proportion X-ray: “thumb shaped” epiglottis • Stridor / airway obstruction / rapid onset / leaning forward / drooling. • Notify ENT, anesthesia, operating room early • Safest in OR: fiberoptic examination, intubation or tracheostomy • Admit (ie, don’t send them home) • Cefuroxime or Unasyn • Humidified oxygen, airway control / cric tray Peritonsillar Abscess • Clinical Features – Fever, malaise, sore throat – Odynophagia, Dysphagia – “Hot potato voice” – Trismus – Can spread, compromise airway • Most common deep neck infection • Rare in children under 12y • Usually Strep • 3-33% recur Peritonsillar Abscess • Clinical Features – Fever, malaise, sore throat – Odynophagia, Dysphagia – “Hot potato voice” – Trismus – Can spread, compromise airway • ED Care – Aspiration with 18- or 20- gauge • Diagnostic and Therapeutic • Try to avoid puncturing Internal Carotid Artery located 2.5cm behind and lateral to the tonsil • Antibiotic therapy with Penicillin Retropharyngeal Abscess • Young children: suppurative lymph node (primary infection elsewhere) • Adults: direct extension of infection, extension to mediastinum more likely • Fever / neck pain / difficulty talking, swallowing and breathing / torticollis • “Cri du canard” = duck-like voice • Intraoral exam shows anterior displacement of the posterior pharyngeal wall • IV Abx (Clinda or Unasyn), surgical drainage Retropharyngeal Abscess X-ray may show soft tissue displacement anterior to vertebral bodies However, expiration and neck flexion may give false-positive X-ray findings CT is the gold standard Other Pharyngeal / Laryngeal / Tracheal Infections • Pharyngitis? • Croup? • Diphtheria? • Tracheitis? Question 4 Which of the following conditions is an unlikely complication of sinusitis? a) Cavernous sinus thrombosis • extension from paranasal sinus b) Dental abscess c) Periorbital cellulitis • extension from ethmoid sinusitis d) Pott’s puffy tumor • extension from forehead anteriorly doughy, edematous e) Subdural empyema • extension from forehead posteriorly empyema or meningitis or brain abscess PEER VII Q76 Q 4 Answer Bacterial sinusitis: more than 7-10 days, fever, hyposmia, unilateral, pus, tender. If it persists, it can extend… to Pott’s puffy tumor, cavernous sinus, or brain… What to do? • Nasal Decongestant Sprays • Antibiotics (14-21 day regimens): • Levaquin, Augmentin, Bactrim For complications: CT or MRI, IV Abx, surgery eval, admit. PEER VII Q76 Cavernous Sinus Thrombosis • Complications of facial infections with extension • Veins of face, oral cavity, middle ear, and mastoid drain to cavernous sinus – dental extraction / sinusitis / periorbital cellulitis / furuncle – high fever, toxic appearance – eyelid edema / proptosis / conjunctival edema (chemosis), facial edema – III and VI nerve palsies and possibly contralateral facial nerve deficit – Pupillary dysfunction Head/neck infection + venous • MRI, dynamic CT obstruction + cranial nerve dysfunction Question 5 A 57-year-old man is transferred form a skilled nursing facility because his tracheostomy tube cuff is not inflating. The tracheostomy was done 5 days earlier for repeated pneumonia and is still in place. The patient has no active bleeding and is in no distress. The most likely complication of replacing the tube is: a) b) c) d) e) Air Trapping • only if they’re really laboring and you leave in the obturator Creating a false passage • still immature Significant bleeding • not unless eroding through to vessel Tracheostomy site closing • If it’s out for several hours, it’s a possibility Tube directed upwards • bad idea to let this happen Tracheostomy • Within the first 7 days post-op, the opening is not mature, and manipulating the tube can lead to false passage in the soft tissues of the neck. – Necessary to have ENT change tube within 7 days post-op • If tube is out for several hours, there is a risk of a closed stoma and dilation may be required. Tracheostomy • If no distress, use an obturator to solidify the tube for maneuvering (this increases air trapping) • Remember: push the tube downward (caudad). Question 6 The most common unilateral neck mass in an adult is: a) Lymphoma b) Mononucleosis c) Parotiditis d) Squamous cell carcinoma e) Thyroid disorder Question 6 – Neck Mass Trivia Young kids: neck masses usually benign: • thyroglossal cyst, branchial cleft cyst, hemangiomas, reactive lymphadenopathy. Young adults: most neck masses are • from infection (Mono) or neoplasm (Hodgkin, lymphoma) In adults: 75% of neck masses are neoplastic. • #1 is Squamous Ca of upper airway/GI with cervical node mets. • Smoking, drinking is a risk. Question 7 A 24-year old woman presents with diffuse tongue swelling that began just prior to arrival. She’s had two prior episodes in the past and her mother has similar problems. She has not eaten any new foods, denies new toiletries, clothing, and meds. Which of the following medications would be most efficacious to treat this condition? a) Cetirizine • for IgE-mediated allergic reactions b) Diphenhydramine • for IgE-mediated allergic reactions c) Epinephrine d) Methylprednisolone • will take hours to work e) Solumedrol • Really, the question was worded like this. Question 7 – Hereditary Angioedema • from C1 esterase defect. Autosomal dominant, usual onset in teens. • Attacks last 2-3 days, may be brought on by airway / GI trauma • Swelling is nondemarcated, nonpruritic. • More common in African-Americans. • aminocaproic acid? FFP? • ACE-mediated angioedema often starts within a week, but can come at any time. You never take it again. • Something about bradykinins • Treat ACE-mediated angioedema like an allergy Question 8 A 2-year-old boy presents with a 2-week history of purulent discharge from the right nostril that has not responded to a 7-day course of amoxicillin. At this point which of the following management plans is most appropriate? a) Change the antibiotic to amoxicillin-clavulanic acid • no effect if FB b) Continue amoxicillin for at least 2 more weeks • come on c) Examine the nose, looking for a foreign body • Unilateral purulent discharge is FB until proven otherwise. d) Order plain radiographs of the sinuses • no value for FB, may confuse issue with sinus opacity e) Start a course of an oral nonsedating antihistamine • no effect if FB PEER VII Q301 Nasal Foreign Body • Unilateral purulent nasal discharge in a preschoolaged child is considered a foreign body until proven otherwise • Plain radiographs unlikely to be of value • Tools for removal include forceps, suction catheters, hooked probes, balloon-tipped catheter Question 9 A 67-year old woman is brought to the ED from her skilled nursing facility for evaluation of fever and right-sided neck swelling. CT scan of the neck shows inflammatory changes in the right parotid consistent with parotitis. Which of the following antibiotic is most appropriate? a) Amoxicillin-clavulanate b) Ampicillin-sulbactam c) Cephalexin and metronidazole d) Clindamycin e) Vancomycin and metronidazole Question 9 – Suppurative Parotitis A 67-year old woman is brought to the ED from her skilled nursing facility for evaluation of fever and right-sided neck swelling. CT scan of the neck shows inflammatory changes in the right parotid consistent with parotitis. Which of the following antibiotic is most appropriate? • Vancomycin and metronidazole • SP caused by retrograde movement of oral flora into salivary gland. • Usually staph or strep, but also see anaerobes. • Risk group: Chronically ill, dry mouth, post-op or sialoliths • If stable, taking PO, can manage as outpatient on augmentin • In a nursing home patient, must cover HA-MRSA. Question 10 For the repair of a complex ear laceration, which of the following nerve blocks is most likely to provide anesthesia? a) Auriculotemporal • branch of the mandibular nerve. Inject anterior and posterior to tragus. b) Inferior Alveolar • mandibular teeth, lip, chin. May hit VII, paralyze c) Infraorbital • cheek, nose, upper lip. May hit eye. d) Mental • lower lip e) Supraorbital • forehead Question 11 A 20 year old woman presents with a painful right ear. She has no history of ear problems but swims several times a week. Examination reveals erythema of the external auditory canal with some purulent discharge and a perforation in the tympanic membrane. The treatment option most likely to damage her ear is: a) b) c) d) e) Ciprofloxacin otic and hydrocortisone otic suspension • Suspension penetrates less than solution, no acid Hydrocortisone and acetic acid otic solution • At pH 3.0, can destroy your middle ear structures, nerves Neomycin/polymyxn/hydrocortisone otic suspension • neomycin has theoretical ototoxic risk Ofloxacin otic solution • this is the only FDA-approved treatment for OE with perf Penicillinase-resistant penicillin • ? Otitis Externa Otitis Externa • Inflammatory process involving the auricle, external auditory canal, and surface of the TM • Pain on movement of auricle, purulent drainage • Caused by gram-negative organisms, Staph aureus, Pseudonomas, or fungi • Peak age 9 -19 years • Erythema, edema of EAC, white exudates on EAC and TM • Pain with motion of tragus or auricle Otitis Externa (continued) • Treatment – Fluoroquinolone otic drops – Oral antibiotics if auricular cellulitis is present or TM is perforated (Quinolones, Cephalosporins, or penicillinase-resistant pcn) • Hydrocortisone and acetic acid otic solution have a pH 3.0 which can be toxic to the middle ear in perforations TM Perforation Causes • Otic Barotrauma – Unequal pressures on either side of the TM – Blocked eustachian tubes (or external canal) • Increased altitude: gas expands in middle ear • Diving injury: increased external pressure on TM • Trauma (slap/blunt, penetrating, acoustic) • Noise (blast injury) / lightning injury • Infection: otitis externa, otitis media, myringitis • Decreased hearing (conductive loss), pain, bleeding TM perforations involving the Pars Tensa TM Perforation • Generally involves pars tensa (largest area), usually anteriorly or inferiorly • 90% heal spontaneously • Early referral (<24hrs) for penetrating trauma or posterior perforation (higher risk of ossicle damage) • Later referral is OK for blunt trauma / barotrauma • Avoid water in ear • Antibiotics (topical or systemic) only for: – obvious infection or forceful water entry (water skiing) Otitis Media • Infants and Young Children (peaks at 6 to 18 months) • 1/3 are viral • Strep pneumoniae most prevalent bacterial cause, also H. flu, M. catarrhalis • Signs include dull, bulging, immobile TM – Light reflex is of no diagnostic value • Serous Otitis media = OM with effusion – painless, fluid behind TM, decreased hearing – affects learning / speech (refer, abx for 3wks) • Treatment – Amoxicillin 80 mg/kg/day PO divided q8 – q12 for 10 days (High-dose amox therapy) Otitis Media Acute Otitis Media •Bulging TM •Loss of Light Reflex •Retraction •Decreased movement on insufflation Question 12 A 75-year-old man presents with fever and ear pain. He has had the earache for several weeks and has been treating it at home with warm mineral oil. On further questioning, he says he is diabetic and that his sugars are running higher than normal. Examination is normal except for the ear, which has granulation tissue on the floor of the external auditory canal. The most likely pathogen causing this infection is: a) b) c) d) e) Aspergillus sp. Candida sp. Pseudomonas aeruginosa Staphylococcus epidermidis Streptococcus pneumoniae PEER VII Q231 Malignant Otitis Externa • Seen in the elderly, diabetic, and immunocompromised patient • Failing 2-3 weeks of antibiotic therapy • Progresses from OE to chondritis to skull osteomyelitis… potentially lethal • Most Common Organism = Pseudomonas aeruginosa • Physical Exam Findings: – Otalgia, Otorrhea – Granulation tissue on floor of EAC • Treatment: – – – – Radiology for staging Admission Parenteral antibiotics Possible surgical debridement Question 13 A 17-year-old girl presents with a painful right ear. She has had the pain for 2 weeks but has not had time to see her family doctor. She is worried because her boyfriend said her ear was red and looked funny. On examination, the ear appears as in the picture, and a posterior auricular crease is not noted. The best treatment option is: PEER VII Q241 Question 13 a) Administer oral antibiotics and discharge b) Administer topical antibiotics and discharge c) Admit for treatment with parenteral antibiotics d) Perform typanocentesis and discharge e) Refer to an ENT for follow up care Mastoiditis is the most serious complication of OM. Mastoid air cells are blocked, inflammed, spreads to periosteum. Image with CT, treat with IV Abx like cefuroxime PEER VII Q241 Mastoiditis • Infection spreads from the middle ear (otitis media) to the mastoid air cells • Clinical Presentation: – Otalgia – Fever – Postauricular erythema, swelling – tenderness – Protrusion of the auricle – Obliteration of the postauricular crease • Imagining – CT Scan – assess extent • Treatment – Emergent ENT Consultation – IV Cefuroxime, Admission – Possible surgical drainage Question 14 A 20 year old man presents with left eye irritation. He was walking in a park and accidentally ran into a tree branch. He believes the branch scratched his eye. Examination reveals a corneal abrasion. The best treatment option is: a) Erythromycin ophthalmic ointment, no patch b) Erythromycin ophthalmic ointment, patch c) Homatropine, no patch d) Homatropine, patch e) Topical anesthetic Don’t prescribe topical anesthetics Patching may help with pain but is contraindicated in contact lenses and “organic” injuries (tree branch). Homatropine relieves ciliary spasm, thought to help with pain. PEER VII Q 160 Corneal Abrasions Corneal Abrasions • Very Painful • Fluorescein reveals dye update at abrasion site • Treatment – Topical Erythromycin, Tobramycin, or Bacitracin/Polymyxin – Tetanus updated – Patching does not facilitate abrasion healing – Topical anesthetics strictly contraindicated • Cause corneal breakdown and ulceration – Cycloplegic agents (homatropine) not recommended • Recent studies show no benefit (Carley and Carley 2001) Keratitis Sxs: Pain, redness, decreased acuity, FB sensation PE: perilimbal flush Causes: Staph, HSV, Zoster, Sjogren’s, exposure, drugs Keratitis can disrupt the epithelial layers making the cornea more susceptible to serious infection Severe Keratitis Sxs: Painful, usually causes iritis, decreased acuity PE: May see Hypopyon (pus in anterior chamber) Causes: central ulcer = GC, peripheral = Stph Rx: Gram stain / culture, cycloplegics, immediate topical and IV abx (genta, tobra, quinolone), urgent consult Viral Keratitis Herpes Simplex (HSV) Dendritic branching pattern Decreased corneal sensation Rx: Antivirals, cycloplegics, Ophtho consult NO STEROIDS May be recurrent Herpes Zoster Opthalmicus Shingles in trigeminal distribution, commonly with lid lesions Hutchinson’s sign = zoster at tip of nose, increased incidence of ocular zoster Rx: Acyclovir IV, cyclopelgic, erythromycin, ophtho consult Steroids if iritis is present (without corneal defect) Subconjunctival Hemorrhage Asymptomatic Cause: Spontaneous or Traumatic Rx: none Consider Ruptured Globe if: – Associated with trauma – Circumferential, dense, elevated – Lateral (then r/o zygoma fracture) Corneal Laceration Teardrop shape of Iris Flat Anterior Chamber Black iris pigment may be at the wound edge Seidel Test: Fluorescein on cornea is washed away by leaking aqueous humor = corneal perforation Tonometry is Contraindicated Rx: Urgent Ophtho Referral Once again… Corneal Abrasion Sxs:Pain, photophobia, FB sensation, injection PE: r/o retained FB under lids Cause: Trauma, consider intraocular FB for high pressure injury Rx: Abx Ointment, remove imbedded FBs Remove Rust Rings? Not urgent Contact lens wearers: anti-pseudomonal ointment (cipro) Question 15 A 55-year-old woman presents complaining of loss of vision in her right eye that occurred suddenly and without pain. Examination reveals a pale, edematous retina with a visible red macula. The most likely cause of this condition is: a) b) c) d) e) Bell’s Palsy • Lid, dryness may affect vision, not eye problem in itself Cataract • come on Embolus • classic description – pale, edematous, cherry red spot Glaucoma • slower, IOP causes nerve damage Optic Neuritis • painful, swollen disc but normal retina PEER VII Q145 Central Retinal Artery Occlusion • Causes – Embolus, thrombosis, arteritis – Sickle Cell Disease – Trauma • Clinical Findings: – – – – – Painless Complete or near-complete vision loss Afferent pupillary defect present Pale fundus on funduscopy examination Cherry-red macula CRAO Treatment True Ocular Emergency. 90-minute window to restore vision Goal is to lower IOP to allow emboli to move to periphery. • • • • • Gentle globe massage Rebreathing into bag -- increase pCO2 to decrease blood flow to globe IV Carbonic anhydrase inhibitors (acetazolamide) Beta blockers (timolol) Anterior Chamber paracentesis by Ophtho Need to w/u carotid and cardiac disease, consider ESR Central Retinal Vein Occlusion Sxs: Slower onset, painLESS, monocular vision loss PE: Retinal hemorrhage, cotton wool spots, macular edema, “blood and thunder” fundus (dilated venous system) Cause: Atherosclerosis, glaucoma Rx: Urgent ophtho consult, r/o CRAO consider ASA, no acute treatment Amaurosis Fugax Sxs: Transient loss of vision, unilateral, painless, lasting 5-30 minutes, with graying/blurring of part or all of visual field Causes: cholesterol or fibrin-platelet arterial emboli, sickle cell, temporal arteritis, collagen-vascular dz, syphillis Rx: Ophtho / Neuro consult, ASA Ocular TIA ?Precursor of retinal artery occlusion Retinal Detachment Another cause of painless vision loss Sxs: “Flashes of light” or “lowering of curtain” in peripheral visual fields, new prominent floaters or webs PE: decreased peripheral vision, retinal / vitreous hemorrhages, grey retina with folds Cause: Trauma, Sickle Cell, Diabetes A tear in the retina allows vitreous fluid to separate retina from the choroid Rx: Fundoscopic exam, US, Emergent Ophtho consult. If tear is inferior, elevate head. If superior, lay flat Question 16 A 50-year-old man presents with left eye pain, blurred vision, watery discharge, and photophobia that began 2 days earlier. He has no history of recent illness or trauma, has quiescent UC. The patient is in moderate discomfort and is shielding his left eye from the light. Physical examination findings are depicted in the picture. Visual acuity is slightly decreased in the left eye and normal in the R eye. Pain with a consensual light reflex is present. Flare is noted on slit-lamp examination, and the intraocular pressure is within normal limits. What is the most likely diagnosis? Question 16 A 50-year-old man presents with left eye pain, blurred vision, watery discharge, and photophobia that began 2 days earlier. He has no history of recent illness or trauma, has quiescent UC. Flare is noted on slit-lamp examination, and the intraocular pressure is within normal limits. What is the most likely diagnosis? a) Acute narrow-angle glaucoma • corneal clouding, high IOP, mid-dilated pupil b) Corneal abrasion • FB sensation, watery discharge, defect on staining c) Iritis • uvea inflammation and ciliary spasm, with flare, ciliary flush d) Orbital cellulitis • pain with eye movement, exophthalmosis e) Scleritis • often bilateral, with nodules, systemic disease The Red Eye • • • • • Conjunctivitis Foreign Body Uveitis / Iritis Narrow angle glaucoma Keratitis C FUNK Iritis / Uveitis • Consensual Light Response eliciting pain in the red eye is highly suggestive of iritis. • Inflammation of the anterior uvea and spasm of the ciliary body results in symptoms – – – – Eye Pain Blurred, decreased vision “Cells” (WBCs) “Flare” (headlights in a fog) • Treatment: – – – – Anticholinergic Preparations Cylcoplegics Topical Steroids Oral Analgesics • Ophtho Consultation Question 17 A 35-year-old woman presents with a painful right eye. She has had the pain for 1 day and some blurred vision as well. Ophthalmoscope examination reveals a swollen optic disc. She has never experienced this and has no medical problems. The best treatment options is: a) Admit for MRI • Maybe later as part of MS workup… not Tx b) Admit for treatment with methylprednisolone • This is optic neuritis. Start IV steroids in the ED. c) Begin treatment with oral prednisone • Oral steroids actually worse than placebo d) Perform lumbar puncture • ? Relief for pseudotumor e) Obtain CBC • Not tx… Optic Neuritis • Inflammation of Optic Nerve – Caused by: • Infection • Demyelination • Autoimmune Disorders • Clinical Presentation: – – – – – – Reduction of vision Pain with extraocular movement Visual field cuts Afferent pupillary defect Swelling of Optic Disc Color vision affected more than visual acuity • ED Care – IV Steroids lower risk of MS in 2 years (oral steroids actually did worse than placebo). – Admission / consult neuro, ophthalmology Optic Neuritis Sxs: decreased vision over hours to days, pain increased by EOM, unilateral (70%) PE: dilated pupil, may have APD, field defect common especially central scotoma (blind spot), red desaturation test (dullness of color), minimal disc elevation Causes: Multiple Sclerosis common (25%), sarcoid, leukemia, viruses, TB, heavy metal ingestion Rx: ED mgmt is controversial, Ophtho consult Acute Angle Closure Glaucoma • Clinical Presentation: – – – – – Eye Pain Headache, N/V steamy hazy cornea Fixed, mid-dilated pupil Increased intraocular pressure of 40 to 70 mm Hg (10-20) Acute Angle Closure Glaucoma • ED Care – – – – – Decrease intraocular pressure Timolol Apraclonidine Acetazolamide IV for pressures > 50mm Hg If pressure does not decrease in 1 hour, give IV Mannitol Question 18 Which of the following physical examination findings most strongly indicates that an eye infection is only a preseptal cellulitis? a) Decreased visual acuity • suggests orbital cellulitis b) Fever • nonspecific c) Pain with blinking • Nonspecific, maybe suggests orbital d) Recent abrasion on the eyelid • Hard to go from here to orbital cellulitis e) Swelling around the eye • nonspecific PEER VII Q260 Periorbital (Preseptal) Cellulitis • History: – Trauma, otitis • Clinical Presentation: – – – – – Warm, indurated, erythematous eyelids No restriction of ocular motility No Proptosis No painful eye movement No impairment of pupillary function • ED Care: – Oral Abx – Augmentin (staph, h. flu) – Need to admit: • Under 5 years-old • Toxic Appearing • Start on IV Abx – Vanco and Ceftriaxone • History: Orbital Cellulitis – Sinus infection • Clinical Presentation: – Warm, indurated, erythematous eyelids – Fever – Toxicity – Restriction of ocular motility – Proptosis – Painful eye movement • Diagnosis: – Orbital and Sinus CT scan w/ and w/out contrast • ED Care: – IV Abx – Cefuroxime or Vanc – Ophtho Consult – Admit Question 19 A 23-year-old man with sickle cell disease presents with blurred vision after being poked in the eye. He has a hyphema. Intraocular pressure is 30. Which of the following drugs might worsen his condition? a) Carbonic anhydrase inhibitor • Contraindicated in sicklers because lower IO pH, stiffer RBC b) Mannitol c) Optic ciprofloxacin d) Topical alpha-adrenergic agonist e) Topical beta-blocker Question 20 Question 20 A 23-year-old man presents holding both hands over his left eye. He was playing basketball when another player hit him in the eye. He is able to cooperate with the examination and reports decreased vision. The definitive treatment option in the emergency department is? a) Carbonic anhydrase inhibitor • Useful in glaucoma-mediated elevated IOP b) Gentle pressure to reduce the eye • Would make things worse (this isn’t CRAO) c) Lateral canthotomy • Because retrobulbar hemorrhage raises IOP, can compromise retina d) Observation pending ophthalmology consultation • This is a true emergency, can’t wait e) Thyroid-stimulating hormone level measurement • Maybe useful in nontraumatic exophalptosis PEER VII Q6 Retrobulbar Hemorrhage Retinal Circulation Compromised Clinical Findings: •Proptosis •Vision Loss •Decrease Ocular Movement •Increased Intraocular Pressure Immediate decompression is Key Lateral Canthotomy is the Best Option Lateral Canthotomy • emergent procedure to relieve orbital compartment pressures • release of lateral canthal tendon Cantholysis • • • • adjunctive procedure to canthotomy can further reduce orbital compartment pressures release of inferior crus of lateral canthus if necessary, may also release superior crus but should avoid if possible as lacrimal gland and artery are in the area Indications • proptosis • decreased visual acuity • increased intraocular pressure >40mm Hg, resistance on ballotment Purpose • temporizing measure • relieves orbital compartment pressures • prevents further neurovascular damage Contraindications • globe rupture Question 21 A 6-year-old boy presents complaining of severe eye pain and blurred vision. He had tipped over a cup of plaster, and some of it splashed in his eye. What is the proper order of management? a) Document visual acuity, irrigate, perform slit lamp exam, measure pH b) Document visual acuity, measure pH, irrigate, perform slit lamp exam c) Irrigate, measure pH, document visual acuity, perform slit lamp exam • Time is vision! No justification for delaying irrigation. Talk to triage nurse. d) Measure pH, irrigate, document visual acuity, perform slit lamp exam e) Perform slit lamp exam, document visual acuity, measure pH, irrigate PEER VII Q328 Chemical Ocular Injury • Acid and Alkali burns are managed in similar manner – Time is Vision – Flush eye immediately • Normal Saline or Ringer’s Lactate – 1-2 Liters (any drinkable fluid…) • Morgan Lens – topical anesthesia may help – Continue to flush until pH is normal (7.0-7.5) – Recheck pH in 20-30 minutes to ensure no additional corrosive is leaching out of tissue – Document Visual Acuity – Rx: • Cycloplegic • Erythromycin Ointment • Narcotic pain medications – Tetanus updated – Ophtho Consultation Chemical Ocular Injury • Acid and Alkali burns are managed in similar manner – What’s worse? Chemical Burn Alkali substances (worse than acids): – Liquefaction Necrosis – Damage is related to initial pH – Tear gas and mace are similar Acid: – Coaguation Necrosis – Penetration is not as deep as with alkali – Chlorine, sulfur The end