* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Cardiovascular response to extreme circumstances
Cardiovascular disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Jatene procedure wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
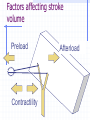
Cardiovascular system in its context Reverend Dr. David C.M. Taylor School of Medical Education [email protected] http://pcwww.liv.ac.uk/~dcmt/cvs06.ppt What is the role of the cardiovascular system? Blood Pressure Depends upon the amount of blood leaving the heart cardiac output and the resistance of the vasculature total peripheral resistance Peripheral Resistance Which will give the greater flow ? Peripheral resistance 2 Which will give the greater flow ? Cardiac Output Heart rate x stroke volume End diastolic volume - End systolic volume Stroke volume Cardiac output Heart rate Factors affecting stroke volume Preload Contractility Afterload increased enddiastolic volume stretches the heart cardiac muscles stretch and contract more forcefully Frank-Starling Law of the heart Tension developed % Preload 100 80 60 40 20 40 60 80 100 120 140 160 Percentage sarcomere length (100% = 2.2 µm) Tension developed % Starling’s Law 2.2 m 1.8 m 3.8 m 100 80 60 40 20 40 60 80 100 120 140 160 Percentage sarcomere length (100% = 2.2 m) Contractility-”Inotropic effect” positive inotropic agents increase available intracellular Ca2+ increase number of actinomyosin binding sites increase force of contraction positive inotropic agents sympathetic stimulation catecholamines glucagon thyroid hormones increased extracellular Ca2+ Afterload decreased arterial blood pressure during diastole decreased afterload semilunar valves open sooner when blood pressure in pulmonary artery & aorta is lower afterload blood pressure viscosity of blood elasticity of arteries Stroke Volume Cardiac Output Heart Rate Heart Rate Nervous system increased sympathetic decreased parasympathetic Chemicals catecholamines thyroid hormones moderate Ca2+ increase Heart Rate 2 Other factors age gender “fitness” body temperature Pacemaker activity The rhythm of the pump is provided by the pacemaker activity of some specialized muscle cells in the wall of the right atrium - the sinoatrial node 0 mV -70 0 mS 300 Chronotropic effect 0 mV -70 0 mS 300 Hypertension David Taylor School of Medical Education Hypertension Excellent article: ABC of Hypertension: The pathophysiology of hypertension, Beevers G, Lip GYH and O’Brien E (2001) BMJ, 322:912-916 Upto 5% of patients with hypertension have it as secondary to some other disease (e.g. renal disease) The rest have “essential hypertension” The story so far... http://pcwww.liv.ac.uk/~dcmt/cvs06.ppt intrinsic (Starling’s Law) extrinsic (principally autonomic) Stroke volume Cardiac output Heart rate Postulated mechanism Increased sympathetic activity Leads to increased cardiac output And peripheral vasoconstriction (to protect the capillary beds) Drop in blood flow Triggers renin-angiotensin system Evidence Cross transplantation studies show that essential hypertension has its origins in the kidneys. Human and animal studies Little evidence that “stress” is involved But, of course, drugs that decrease sympathetic activity lower blood pressure. Control Autonomic N.S. Volume ADH Pressure Chemicals Local Blood Flow Angiotensin Pressure Sensed by baroreceptors in carotid arteries and aortic arch an increase in pressure causes a decrease in sympathetic activity a decrease in pressure causes an increase in sympathetic activity Volume Sensed by atrial volume receptors A decrease in volume causes an increase in ADH secretion and a decrease in ANF secretion Chemicals A decrease in O2, or more usually an increase in CO2 or H2 causes an increase in chemoreceptor activity which increases sympathetic activity Local Blood Flow (kidney) Decreased renal blood flow Monitored by JGA cells Renin production Angiotensinogen Angiotensin I Converting enzyme Angiotensin II Sodium reabsorption Aldosterone Potassium secretion Vasoconstriction Hormones Angiotensin II is a vasoconstrictor Aldosterone increases vascular sensitivity to Angiotensin II ADH (anti-diuretic hormone) increases water reabsorption ANF decreases sodium reabsorption Overview ADH Fluid loss Arterial pressure Blood volume Venous return heart rate vol sympathetic contractility vasoconstriction Cardiac output baro Arterial pressure chemo CNS Cardiac output Venous return veins capillary pressure Blood volume Local blood flow kidney renin/angiotensin aldosterone Shock David Taylor School of Medical Education Shock Stage 1 Compensated/Nonprogressive mechanisms work as planned Stage 2 Decompensation/Progressive if blood volume drops more than 15 - 25% Stage 3 Irreversible Progressive shock depression of cardiac activity bp <60 mmHg poor flow through coronary arteries leads to ischemia depression of vasoconstriction bp 40 - 50 mmHg increased capillary permeability caused by hypoxia clotting, cell destruction, acidosis