* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Physiology Lec.(2) Dr. Abeer mansoor
Survey
Document related concepts
Transcript
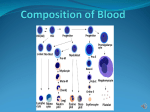
Physiology Lec.(2) Dr. Abeer mansoor ----------------------------------------------------------Production of Red Blood Cells:Areas of the Body That Produce Red Blood Cells. In the early weeks of embryonic life, primitive, nucleated red blood cells are produced in the yolk sac . During the middle trimester of gestation, the liver is the main organ for production of red blood cells, but reasonable numbers are also produced in the spleen and lymph nodes. Then ,during the last month of gestation and after birth ,red blood cells are in bone marrow Pluripotential Hematopoietic Stem Cells, Growth Inducers, and Differentiation Inducers. The blood cells begin their lives inthe bone marrow from a single type of cell called the pluripotential hematopoietic stem cell, from which all the cells of the circulating blood are derived. . As these cells reproduce, a small portion of them remains exactly like the original pluripotential cells and is retained in the bone marrow to maintain a supply of these, although their numbers diminish with age. Most of the reproduced cells,however, differentiate to form the other cell types . The intermediate stage cells are very much like the pluripotential stem cells, even though they have already become committed to a particular line of cells and are calledcommitted stem cells.The different committed stem cells, when grown inculture, will produce colonies of specific types of blood cells. A committed stem cell that produces erythrocytes is called a colony-forming unit–erythrocyte, andthe abbreviation CFU-E is used to designate this typeof stem cell. Likewise, colony-forming units that form granulocytes and monocytes . Growth and reproduction of the different stemcells are controlled by multiple proteins called growth inducers. Four major growth inducers. One of these, interleukin-3, promotes growth and reproduction of virtually all the different types of committed stem cells, The growth inducers promote growth but not differentiation of the cells.This is the function of another set of proteins called differentiation inducers . 1 2 Regulation of Red Blood Cell Production—Role of Erythropoietin Tissue Oxygenation Is the Most Essential Regulator of Red Blood Cell Production. Any condition that causes the quantity of oxygen transported to the tissues to decrease ordinarily increases the rate of red blood cell production. Thus, when a person becomes extremelyanemic as a result of hemorrhage or any other condition, the bone marrow immediately begins to producelarge quantities of red blood cells.Also, destruction of major portions of the bone marrow by any means, especially by x-ray therapy, causes hyperplasia of the remaining bone marrow, thereby attempting to supplythe demand for red blood cells in the body. At very high altitudes, where the quantity of oxygen in the air is greatly decreased, insufficient oxygen is transported to the tissues, and red cell production isgreatly increased. In this case, it is not the concentration of red blood cells in the blood that controls red cell production but the amount of oxygen transported to the tissues in relation to tissue demand for oxygen.Various diseases of the circulation that cause decreased blood flow through the peripheral vessels,and particularly those that cause failure of oxygen absorption by the blood as it passes through the lungs, can also increase the rate of red cell production. This is especially apparent in prolonged cardiac failure and in many lung diseases, because the tissue hypoxia resulting from these conditions increases red cell production, with a resultant increase in hematocrit and usually total blood volume Erythropoietin Stimulates Red Cell Production, and Its Formation Increases in Response to Hypoxia. 3 The principal stimulus for red blood cell production in low oxygen states is a circulating hormone called erythropoietin, a glycoprotein with a molecular weight of about 34,000. Inthe absence of erythropoietin, hypoxia has little or no effect in stimulating red blood cell production. Role of the Kidneys in Formation of Erythropoietin. In the normal person, about 90 per cent of all erythropoietin is formed in the kidneys; the remainder is formed mainly in the liver. It is not known exactly where in the kidneys the erythropoietin is formed. One likely possibility is that the renal tubular epithelial cells secrete the erythropoietin, because anemic blood is unable to deliver enough oxygen from the peritubular capillaries to the highly oxygen-consuming tubular cells, thus stimulating erythropoietin production Factors that decrease oxygenation 1. Low blood volume 2. Anemia 3. Low hemoglobin 4. Poor blood flow 5. Pulmonary disease Effect of Erythropoietin in Erythrogenesis. the important effect of erythropoietin is to stimulate the production of proerythroblasts from hematopoietic stem cells in the bone marrow. In addition, once the proerythroblasts are formed, the erythropoietin causes these cells to pass more rapidly through the different erythroblastic stages than they normally do, further speeding up the production ofnew red blood cells.The rapid production of cells continues .In the absence of erythropoietin, few red blood cells are formed by the bone marrow. . Especially important for final maturation of the red blood cells are two vitamins, vitamin B12 and folic acid. Both of these are essential for the synthesis of DNA, because each in a different way is required for the formationof thymidine triphosphate, one of the essential building blocks of DNA. Therefore, lack of either vitamin B12 or folic acid causes abnormal and diminished DNA and, consequently, failure of nuclearmaturation and cell division. , Maturation Failure Caused by Poor Absorption of Vitamin B12 from the Gastrointestinal Tract—Pernicious Anemia. A common cause of red blood cell maturation failure is failure to absorb vitamin B12 from the gastrointestinal tract. This often occurs in the disease pernicious anemia, in which the basic abnormality is an atrophic gastric mucosa that fails to produce normal gastric secretions. The parietal cells of the gastric glands secrete a glycoprotein called intrinsic factor, which combines with vitamin B12 4 in food and makes the B12 available for absorption by the gut. It does this in the following way: (1) Intrinsic factor binds tightly withthe vitamin B12. In this bound state, the B12 is protectedfrom digestion by the gastrointestinal secretions. (2) Still in the bound state, intrinsic factor binds to specific receptor sites , carrying intrinsic factor and the vitamin together through the membrane. Failure of Maturation Caused by Deficiency of Folic Acid (Pteroylglutamic Acid). Folic acid is a normal constituentof green vegetables, some fruits, and meats (especiallyliver). However, it is easily destroyed during cooking.Also, people with gastrointestinal absorption abnormalities, such as the frequently occurring small intestinal disease called sprue, often have serious difficulty absorbing both folic acid and vitamin B12. Therefore, in many instances of maturation failure, the cause isdeficiency of intestinal absorption of both folic acid and vitamin B12. Formation of Hemoglobin Hb consists of aprotein component globin and an iron containing Pigment haem.iron exists in ferrous form and each molecule of Hb Contains four iron atoms .Hb combines with the oxygen to form aloose reversible compound oxy-haemoglobin,which rapidly dissociate in the tissue to release oxygen. hemoglobin chain . Each chain has a molecular weight of about 16,000; four of these in turn bind together loosely to form the whole hemoglobin molecule. There are several slight variations in the different subunit hemoglobin chains, depending on the amino acid composition of the polypeptide portion. The different types of chains are designated alpha chains, beta chains, gamma chains, and delta chains. The mostcommon form of hemoglobin in the adult human being, hemoglobin A, is a combination of two alpha chains and two beta chains. . The types of hemoglobin chains in the hemoglobin 5 Abnormalities of the chains can alter the physical characteristics of the hemoglobin molecule as well. For instance, in sickle cell anemia, the amino acid v aline is substituted for glutamic acid at one point in each of the two beta chains. When this type of hemoglobin is exposed to low oxygen, it forms elongated crystals inside the red blood cells that are sometimes 15 micrometers in length. These make it almost impossible for the cells to pass through many small capillaries, and the spiked ends of the crystals are likely to rupture the cell membranes, leading to sickle cell anemia. Types of haemoglobin 1-foetal Hb:it is present in the fetal blood and its structure is the same as that of adult Hb.in fetal Hbthe beta chains of globin are replaced by gamma chain .normally fetal Hb is replaced by adult form at birth but in some cases it may persist during adult life.The fetal Hbhas greater affinity for oxygen. 2-Methaemoglobin When blood is exposed to various oxidizing agents or even otherwise under the influence of certain drugs,ferrous iron is converted into ferric form.This is known as methaemoglobin and it gives dark colour to blood.However,red cells contain enzymes which reconvert it into haemoglobin.The absence of these enzymes results in methaemoglobinemia 3-Carboxy haemoglobin:The affinity of carbon monoxide for haemoglobin is greater than that of oxygen .The compound thus formed is known as carboxyhaemoglobin.it causes areduction in oxygen transport capacity of blood and can be fatal to life. Iron Metabolism Because iron is important for the formation not only of hemoglobin but also of other essential elements inthe body (e.g., myoglobin, cytochromes, cytochrome oxidase, peroxidase, catalase), it is important to understand the means by which iron is utilized in the body. The total quantity of iron in the body averages 4 to 5grams, about 65 per cent of which is in the form of hemoglobin. About 4 per cent is in the form of myoglobin,1 per cent is in the form of the various hemecompounds that promote intracellular oxidation, 0.1 per cent is combined with the protein transferrin in theblood plasma, and 15 to 30 per cent is stored for later use, mainly in the reticuloendothelial system and liverparenchymal cells, principally in the form of ferritin. Transport and Storage of Iron. Transport, storage, and metabolism of iron in the body When iron is absorbed from the small intestine, it immediately combines in the blood plasma with a beta globulin, apotransferrin, to form transferrin, which is then transported in the plasma. The iron is loosely bound in the transferrin and, consequently, can be released to any tissue cell at any point in the body. 6 Excess iron in the blood is deposited especially in the liver hepatocytes and less in the reticuloendothelialcells of the bone marrow. In the cell cytoplasm, iron combines mainly witha protein, apoferritin, to form ferritin. ,ferritin may contain only a small amount of iron or a large amount. This iron stored as ferritin is called storage iron. , ferritin particles are so small and dispersed that they usually can be seen in the cell cytoplasm only with the electron microscope. When the quantity of iron in the plasma falls low, some of the iron in the ferritin storage pool is removed easily and transported in the form of transferrin in the plasma to the areas of the body where it is needed.A unique characteristic of the transferrin molecule is thatit binds strongly with receptors in the cell membranes of erythroblasts in the bone marrow. Then, along withits bound iron, it is ingested into the erythroblasts by endocytosis. There the transferrin delivers the iron directly to the mitochondria, where heme is synthesized. In people who do not have adequate quantitiesof transferrin in their blood, failure to transport iron to the erythroblasts in this manner can cause severehypochromic anemia Destruction of Hemoglobin. When red blood cells burst and release their hemoglobin, the hemoglobin is phagocytized almost immediately by macrophages in many parts of the body, but especially by the Kupffer cells of the liver and macrophages of the spleen and bone marrow. During the next few hours to days, the macrophages release iron from the hemoglobin and pass it back into the blood, to be carried by transferring either to the bone marrow for the production ofnew red blood cells or to the liver and other tissues for storage in the form of ferritin. The porphyrin portionof the hemoglobin molecule is converted by the macrophages, through a series of stages, into the bile pigment bilirubin, which is released into the blood and later removed from the body by secretion through theliver into the bile; Anemias Anemia means deficiency of hemoglobin in the blood, which can be caused by either too few red blood cellsor too little hemoglobin in the cells. Some types of anemia and their physiologic causes are the following. Blood Loss Anemia. After rapid hemorrhage, the body replaces the fluid portion of the plasma in 1 to 3 days,but this leaves a low concentration of red blood cells. If a second hemorrhage does not occur, the red bloodcell concentration usually returns to normal within 3 to 6 weeks.In chronic blood loss, a person frequently cannot absorb enough iron from the intestines to form hemoglobinas rapidly as it is lost. Red cells are then produced that are much smaller than normal and have 7 toolittle hemoglobin inside them, giving rise to microcytic, hypochromic anemia, . Aplastic Anemia. Bone marrow aplasia means lack of functioning bone marrow. For instance, a person exposed to gamma ray radiation from a nuclear bomb can sustain complete destruction of bonemarrow, followed in a few weeks by lethal anemia. Likewise, excessive x-ray treatment, certain industrial chemicals, and even drugs to which the person might be sensitive can cause the same effect. Megaloblastic Anemia. Based on the earlier discussions of vitamin B12, folic acid, and intrinsic factor from the stomach mucosa, one can readily understand that loss of any one of these can lead to slow reproduction oferythroblasts in the bone marrow. As a result, the red cells grow too large, with odd shapes, and are called megaloblasts. Thus, atrophy of the stomach mucosa, as occurs in pernicious anemia, or loss of the entire stomach after surgical total gastrectomy can lead to megaloblastic anemia. Also, patients who have intestinal sprue, in which folic acid, vitamin B12, and other vitamin B compounds are poorly absorbed, oftendevelop megaloblastic anemia. . Hemolytic Anemia. Different abnormalities of the red blood cells, many of which are hereditarily acquired,make the cells fragile, so that they rupture easily as they go through the capillaries, especially through the spleen. Even though the number of red blood cells formed may be normal, or even much greater than normal in some hemolytic diseases, the life span of the fragile red cell is so short that the cells are destroyed faster than they can be formed, and serious anemia results. Some of these types of anemia are thefollowing. In hereditary spherocytosis, the red cells are verysmall and spherical In sickle cell anemia, which is present in West African and American blacks, the cellshave an abnormal type of hemoglobin called hemoglobin S, containing faulty beta chains in the hemoglobinmolecule, When this hemoglobin is exposed to low concentrations of oxygen, it precipitates into long crystals inside the red blood cell.These crystals elongate the cell and give it the appearance of a sickle rather than a biconcave disc. The precipitated hemoglobin also damages the cell membrane, so that the cells become highlyfragile, leading to serious anemia. In erythroblastosis fetalis, Rh-positive red blood cells in the fetus are attacked by antibodies from an Rh-negative mother. These antibodies make the Rhpositive cells fragile, leading to rapid rupture andcausing the child to be born with serious anemia Polycythemia 8 Secondary Polycythemia. Whenever the tissues become hypoxic because of too little oxygen in the breathe air, such as at high altitudes, or because of failure of oxygen delivery to the tissues, such as in cardiacfailure, the bloodforming organs automatically produce large quantities of extra red blood cells. Thiscondition is called secondary polycythemia, and the red cell count commonly rises to 6 to 7 million/mm3,about 30 per cent above normal.A common type of secondary polycythemia, called physiologic polycythemia, occurs in natives who live at altitudes of 14,000 to 17,000 feet, where the atmospheric oxygen is very low.The blood count is generally 6 to7million permm3 Polycythemia Vera (Erythremia). a pathological condition known as polycythemia vera, in which the red blood cell count may be 7 to 8million/mm3 and the hematocrit may be 60 to 70 per cent instead of the normal 40 to 45 per cent. Polycythemiavera is caused by a genetic aberration in the hemocytoblastic cells that produce the blood cells. In polycythemia vera, not only does the hematocrit increase, but the total blood volume also increases, onsome occasions to almost twice normal.As a result, the entire vascular system becomes intensely engorged. Inaddition, many blood capillaries become plugged by the viscous blood; the viscosity of the blood in polycythemia vera increase 9