* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download CONGENITAL SYPHILIS
Clostridium difficile infection wikipedia , lookup
Herpes simplex wikipedia , lookup
Tuberculosis wikipedia , lookup
Brucellosis wikipedia , lookup
Chagas disease wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Marburg virus disease wikipedia , lookup
West Nile fever wikipedia , lookup
Toxoplasmosis wikipedia , lookup
Diagnosis of HIV/AIDS wikipedia , lookup
Trichinosis wikipedia , lookup
Onchocerciasis wikipedia , lookup
Sarcocystis wikipedia , lookup
Leptospirosis wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Hepatitis C wikipedia , lookup
Hepatitis B wikipedia , lookup
Schistosomiasis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Fasciolosis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Lymphocytic choriomeningitis wikipedia , lookup
Neonatal infection wikipedia , lookup
Epidemiology of syphilis wikipedia , lookup
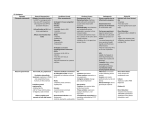
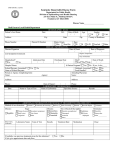
CONGENITAL SYPHILIS SINDHU E. PHILIP, MD. DEPARTMENT OF PEDIATRICS 09/20/02 Introduction Infant usually infected in utero by transplacental passage of Treponema pallidum from infected mother at any time. Infection may also occur from contact with an infectious lesion during passage through the birth canal It remains unclear what factors determine which mothers, particularly those in the latent stage, will pass the disease to the fetuses. Also unclear why some infants, infected in utero, are born asymptomatic, but develop overt dz. In first few wks./mo. Epidemiology Worldwide, but more frequent in urban areas. Incidence of congenital syphilis has dramatically decreased in the U.S. since 1991. Infection can be transmitted to fetus at any stage of disease. Rate of infection 60% - 100% during second stage. Transmission rates slowly decreases with increasing duration of the disease. Women, untreated early syphilis: 40% of pregnancies result in spontaneous abortion, stillbirth, or perinatal death. Pathogenesis Infection before 4th month of pregnancy? Possible that treponemes do in fact pass from mother to fetus before 5th month of gestation, but classic pathologic changes do not occur until after 5th month. Infection involves the placenta, and spreads hematogenously to the fetus, widespread involvement is characteristic. Infected placenta is paler, thicker, and larger than normal. Clinical Manifestations Damage to fetus depends on the stage of development at which infection has taken place and time elapsed before treatment. Early infection, untreated: miscarriage, stillbirth, neonatal death, IUGR, premature delivery. Survivors: Early congenital syphilis: clinical manifestations within first 2 years of life Late congenital syphilis: clinical manifestations after 2yo. Early Congenital Syphilis Early manifestations are varied, with multi-system Involvement • Hepatosplenomegaly- diffuse inflammation, scarring • Jaundice – due to hepatitis • Generalized lymphadenopathy – epitrochclear nodes • Coombs – hemolytic anemia, thromobocytopenia, leukopenia, leukocytosis • Hydrops fetalis • Mucocutaneous: rhinitis (highly infectious), “snuffles”, mucous patches • Macuolpapular rash • Desquamation • Pemphigus syphiliticus (vesicular bullous eruptions of palms and soles) • Petechial lesions • Bony lesions, osteochondritis, periostitis, pseudoparalysis • Syphilitc leptomeningitis • Chorioretinitis,salt and pepper fundus, glaucoma • Pancreatitis Papulosquamous Plaques Broken vesicles, desquamation Condylomata around anus Infiltration, desquamation and rhinitis Rhinitis (snuffles), mucous patches, damage to palate(late) Bullae and vesicular rash on soles Eroded papular lesions Lone Bone Radiographs Osteochondritis of distal radius and ulna Osteochondritis of femur and tibia metaphysis Late Congenital Syphilis Results primarily from chronic inflammation of bone, teeth, and CNS. • Interstitial keratitis (inflammatory) • Nerve deafness • Clutton’s Joints (synositis, restricted movement) • Hutchinson’s triad (teeth, intersitial keratitis, 8th nerve deafness) • Mulberry molars • Flaring scapulas • Hydrocephalus • • • • • • • Mental retardation Frontal bossing Saddle nose Protruding mandible High arched palate Perioral fissures Higouemenaki’s sign(periosteal rxn of clavicle, sternocleidomastoid) • Saber shins • Rhagades (linear scars that become fissured or ulcerated) Hutchinson’s teeth – peg shaped upper incisors Frontal Bossing Saber shins: Anterior bowing of tibias Gumma: Thin atrophic scar Diagnosis Definitive diagnosis can be made by dark-field microscopy on specimen from skin lesions, placenta, umbilicus. Serologic tests are the principal means for diagnosis: 1) Nontreponemal test: VDRL, RPR 2) Treponemal tests: TPI, FTA-ABS, MHA-TP Diagnosis Nontreponemal: VDRL, RPR Quantitative results correlate with disease activity, therefore helpful in screening. Titers rise when disease is active, fall when treatment is adequate In congenital infxn. These tests become non- reactive within a few months of adequate treatment. Non-treponemal testing Detects antibodies against a cardiolipin- cholestrollecithin complex, not specific for syphilis. False Positives: Only in serum, not in CSF testing certain viral infxns: infectious mononucleosis, hepatitis, varicella, measles lymphoma, TB, malaria, endocarditis, connective tissue disease pregnancy (?) abuse of injection drugs Diagnosis A sustained 4 fold decrease in titer of nontreponemal test after treatment demonstrates adequate therapy. A 4 fold increase titer increase after treatment suggests reinfection or relapse. Confirmatory Testing Treponemal Tests: TPI, FTA-Abs, MHA-TP Treponemal antibody titers become positive soon After initial infection and usually remain positive For life, even with adequate therapy. Antibody titers do not correlate with disease activity, and are not quantified. Not 100% specific for syphilis: other spirochetal dz, Infant Testing Reactive serology in neonate could be due to IgG passively transferred to newborn through placenta, and does not indicate active infection. If infant’s titer higher than mother’s congenital infection If decreasing titer in infant passive transfer of antibodies, should disappear by 3-4 months of age. Persistently reactive VDRL, with rising titer Active Infection Recommended Interpretation Non-treponemal Test (VDRL, RPR, EIA, ART) Treponemal Test (MHA-TP, FTAABS) Mother Infant Mother Infant Interpretation - - - - No syphilis or incubating syphilis in the mother and infant. + + - - No syphilis in mother (false-positive non-treponemal test with passive transfer to infant). + +/- + + Maternal syphilis with possible infant infection; or mother treated for syphilis during pregnancy; or mother with latent syphilis and possible infection of infant. + + + + Recent or previous syphilis in the mother; possible infection in the infant. + Mother successfully treated for syphilis before or early in pregnancy; or mother with Lyme disease, yaws, or pinta (ie, false-positive serology). - - + CSF Examination CSF abnormalities may occur in congenital syphilis Even in absence of neurologic involvement. * Leukocytosis * Elevated protein in CSF * positive VDRL (no false positives) Evaluation • Maternal hx, results of serologic testing • Thorough P.E. • Long bone xrays • Non-treponemal AB titer • Treponemal AB titer • Head US • Csf Analysis for VDRL, cell count & protein • CBC with platlets • LFT’s • UA • Chest xray • HIV antibody test • Opthalmologic exam Treatment Proven or highly probable: Aqueous crystalline Penicillin G 100,000-150,000U/kg/day (given q8-q12hrs) IV for 10 days OR Procaine Penicillin G 50,000 U/kg/day IM for 10days If >1 day of therapy missed, entire course should be restarted! Treatment Asymptomatic, Normal CSF exam, CBC, platelets, and Radiologic exam: 1. No maternal tx aqueous PCN G IV for 10-14 days 2. Tx w/ Erythromycin clinical, serologic follow-up, and Benzathine Pcn G IM x 1 3. Tx < 1month before Delivery, or <4 fold Decrease in titers clinical, serologic follow-up and Benzathine Pcn G IM x 1 Treatment Treat all newborns w/ positive VDRL as if they have congenital syphilis, even if mother thought to not have an active infection. 1. Difficult to document that mother received adequate tx, and has falling VDRL titer. 2. Low titer VDRL test may be compatible with latent maternal syphilis. 3. Newborn may not have clinical manifestations at birth. 4. Compliance with follow-up visits may be problem. Follow-up Should have careful follow-up examination at 1, 2, 4, 6, and 12 months of age. Serologic non-treponemal tests: 3, 6, 12 months, and end of tx (or until non-reactive) Non-treponemal Ab titers decline by 3 months of age, and Should be Non-reactive by 6 months, if infant was not infected. (transplacentally aquired antibodies.) If persistent, stable titers, consider retreatment. Congenital neurosyphilis- CSF exam at 6 month intervals until normal Research Advances UT Southwestern Medical Center at Dallas research team has develop 2 blood test that quickly and reliably diagnose Congenital syphilis in newborns. (June, 2002) Detect neonatal antibodies to the syphilis bacterium or the DNA of the syphilis organism itself, as predictors of CNS Invasion. (one day vs. ten days of PCN) 1. IgM Immunoblotting test 2. PCR In 1998 scientist at UTHSC in Houston, Institute for Genomic Research in Maryland, mapped the 1.1 million base pairs of DNA that make up the syphilis genome.Entire genomic pattern of Treponema Pallidum now known. Difficult to study previously b/c of dependence on mamalian host for viability. New breakthroughs?