* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Slide 1
Typhoid fever wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
West Nile fever wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Chagas disease wikipedia , lookup
Oesophagostomum wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Hepatitis B wikipedia , lookup
Herpes simplex virus wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Rocky Mountain spotted fever wikipedia , lookup
Marburg virus disease wikipedia , lookup
Schistosomiasis wikipedia , lookup
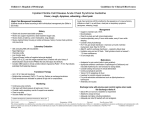
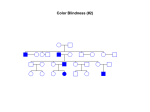
Morning Report August 24, 2009 Visual Diagnosis You are seeing a 10 year old AA male with fever, increased WOB, chest pain and cough. His RA saturation is 92% What else do you want to know??? • Duration of symptoms has been only 1 day. There has been no improvement with tylenol or tylenol with codeine (foster mom had some left over from her hospitalization and tried one) • The temp at home has been as high as 102. • No sick contacts. • PMH: this is foster mom and she has no information about this child as she has had him for only 3 weeks. His mom died from a drug overdose and his dad is not involved and unknown to the child. He looks unwell……what do you do?? Labs?? Images?? Fluids?? The CXR is done The CBC comes back: Hgb is 7 Hct is 21 WBC is 21 (no differential yet) PLTs “nl” Lytes are normal LFT’s are mildly elevated (200’s) Differential Diagnosis Time ??? HINT (your turn to talk) After 20 cc per kg of NS, his dyspnea worsens and you are called to the bedside by a frightened ER RN. Your patient has diminished BS on the right. He is crying because he feels as if he cannot breathe. He has been placed on a nonrebreather mask and his saturation is 96% Now what? The repeat CXR Time to circle your number one thought…….10 year old AA male dyspnea, fever, chest pain, mild cardiomegaly, rapidly progressive change in CXR, significant anemia, mild elevations in LFT’s Sickle cell disease with Acute Chest Syndrome Sickle Cell Statistics •1 in every 375 AA in USA • 1 in every 1200 Latino •9% AA in US carry trait •Up to 25% in parts of Africa carry trait •NBS in 44 states & DC •Life Expectancy 45; (Tripled over Last 30 years) normal Not normal Molecular Mechanisms Single Nucleotide substitution (GTG for GAG) @ codon 6 Beta globin gene on chromosome 11 Valine substitution for glutamine causes hypoxia induced polymerization leading to the classic crescent shape •Increased adhesiveness •Increased reticulocytes •Vasoconstriction (+ET1 and –NO) •Abnormal NO metabolism •Elevated Plts and Thrombin Activity Acute Chest Syndrome • 50% of patient with SCD will experience at least one episode • Typically present with fever, cough, chest pain, SOB, new infiltrate, hypoxia • Atelectasis hypoxemia sickling • 50% admitted with another diagnosis Acute Chest Syndrome • Cause identified in 55% (30% Infection, 16% presumed pulmonary infarction, 9% Fat Embolism) • In Children, Infection More Likely Infectious Agents: Chlamydia, Mycoplasma and RSV • 20% have bronchospasm responsive to bronchodilators (Corollary: Asthmatics have a two fold higher risk of ACS) Management •Oxygen •IVF •Pain Control •Antibiotics (CTX & Azithro) •Bronchodilators •Incentive Spirometer •Ambulation •Simple vs. Exchange Transfusion Goal HbS <30% & Final Hb no more than 10 Best Practices for SS Disease • Penicillin prophylaxis prevents pneumococcal sepsis in children [evidence from Prophylactic Penicillin Studies I and II(PROPS I & II)]. • Pneumococcal vaccine prevents pneumococcal infection in children. • In surgical settings, simple transfusions to increase hemoglobin (Hb) levels to 10g/dL are as good as or safer than aggressive transfusions to reduce sickle hemoglobin (Hb S) levels to below 30 percent. More Best Practice for Children • Transfusions to reduce Hb S levels to below 30 percent prevent strokes in children with high velocity central nervous system blood flow by TCD [evidence from the Stroke Prevention Trial in Sickle Cell Anemia(STOP I)]. • Hydroxyurea decreases crises in patients with severe sickle cell disease [evidencefrom the Multicenter Study of Hydroxyurea in Sickle Cell Anemia (MSH) trial]. Take Home Messages • SCD is common • SCD impacts every organ system • ACS is treated with diligent supportive care Two more Cases from PREP A 6month old girl, who was born in Nigeria, presents for an urgent visit as soon as the family arrives in the United States because of fever and irritability. Physical examination reveals a fussy infant who has anorexia, a temperature of 100°F (37.8°C), and swelling of all of the fingers of the right hand . The remainder of the examination findings are negative. Of the following, the MOST likely cause of this pattern of swelling in this child is A. cellulitis B. juvenile idiopathic arthritis C. malaria D. sickle cell disease E. trauma You are evaluating a 7year old boy who has sickle cell disease for a 5 day history of fever, rhinorrhea, headache, and worsening fatigue. Physical examination reveals a tired appearing, pale boy VS: 101.5°F (38.6°C); HR: 150 very pale conjunctivae and mucous membranes He has a faint diffuse erythematous lacy rash that is most prominent on his cheeks and trunk. Laboratory tests show a white blood cell count of 12 with 50% neutrophils, 45% lymphocytes, and 5% monocytes; hemoglobin of 4 , hematocrit of 16 and a reticulocyte count of less than 1% (0.01). Of the following, the MOST likely cause for this patient's present illness is infection with A. coxsackievirus B. cytomegalovirus C. EpsteinBarr virus D. parainfluenza virus E. parvovirus B19 Parvo B19 Fifth’s Disease