* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Snímek 1
Heart failure wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Coronary artery disease wikipedia , lookup
Myocardial infarction wikipedia , lookup
Jatene procedure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
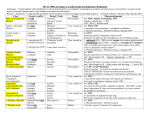
Systemic arterial hypertension Blood pressure BP is defined by physical factors of circulatory system (compliance and elasticity) P = Q x R (analogy of Ohm’s law) P = mean arterial pressure Q = amount of circulating blood R = resistance against blood flow in exact part of cardiovascular system Systolic arterial pressure Factors affecting its levels: Venous return and acquired preload of ventricles Contractility of myocardium Systolic volume – amount of blood ejected with one ventricular contraction Speed/rate of ejection to the large arteries Compliance of large arteries of elastic type Resistance in the arteries of muscular type Diastolic arterial pressure Depends on: Systolic pressure Peripheral resistance Time between two systoles Arterial HTN • HTN is BP above 140/90 mm Hg (WHO) • Pulmonary circulation – upper limits: 30/12 mm Hg Increase in BP could be the result of: • Increase in blood volume (Q) • Increased resistance of vessels (R) • Combination of both mechanisms (Q + R) System arterial hypertension • In 95% of cases cause (or pathogenesis) is unknown = essential (primary) hypertension Hypothesis • Disorders of reabsorption of salt and water in kidneys • Changes in reactivity of sympathoadrenal system • In the remaining 5% of cases causes and pathogenesis are know = secondary hypertension Primary HTN Genetic factors + environmental factors + disorders of regulation mechanisms 1. Genetic factors: 30% of those participate in the development of HTN Familiar predisposition The responsible gene has not been identified yet Polygenic and heterogenic inheritance Changes in polymorphism of gene responsible for angiotenzinogen are often 2. Environmental factors Increased Na intake: reduction of intake has beneficial effect in HTN management High caloric intake: HTN is 2-3fold more often in obese patient (increased Na in high food intake + insulinoresistance) Increased alcohol intake: ↑ sympathoadrenal activity, ↓ magnesium, etc. Smoking: mobilization of catecholamines and other vasoconstrictive substances, activation of atherosclerosis development Psychological stress Secondary HTN Secondary HTN as main result of increased peripheral resistance • • Pheochromocytoma Renal artery stenosis Secondary HTN as main result of increased blood volume and its circulation • • • • Primary hyperaldosteronism (Conn syndrome) Cushing syndrome (hypercortisolism) Acromegaly Hyperthyreosis Secondary HTN as a result of increased peripheral resistance and blood volume • • End-stage chronic kidney failure Hypothyreosis Pressure overload of the heart in HTN (increased afterload) Causes: Increased peripheral vascular resistance Narrowing of lumen (acceleration of atherosclerosis) Pressure overload leads to • Changes in ejection fraction • Changes in ejection volume With time leads to eventual left-sided heart failure Volume overload of the heart in HTN (increased preload) • • • Result of hyperkinetic/hyperdynamic circulation Systolic volume is increased as a result of increased preload Heart adapts by hypertrophy and dilatation