* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Sinus Rhythms - Beaumont Emergency Medicine
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Electrocardiography wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
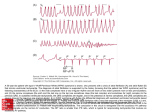
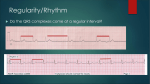
Cardiac Arrhythmias A Guide For Medical Students William Beaumont Hospital Department of Emergency Medicine Evaluating Arrhythmias Rate – Is it fast or slow? If slow, is there group to group beating? Rhythm – Is it regular, irregular or irregularly irregular? P waves – Are they present? QRS – Is it narrow or wide? Sinus Bradycardia What is it? What causes it? When do you treat it? How do you treat it? Sinus Bradycardia Characteristics: Sinus rhythm Normal intervals Rate less than 60 bpm Etiology: Normal variant Beta blocker overdose Digoxin overdose Hypothermia Hypothyroidism Brady-tachy syndrome SA node ischemia Sinus Bradycardia Treatment: Requires treatment only if there is evidence of hypoperfusion Two treatment options: Pacing: transvenous or transcutaneous Atropine 0.5 mg IVP Sinus Tachycardia Characteristics: Sinus rhythm Faster than 100 bpm Etiology: Usually a physiologic response to a stressor Volume depletion / low stroke volume Hypoxia Systemic pathology: fever, anemia, hyperthyroidism Drugs Treatment: Treat the underlying cause Atrial Arrhythmias Premature Atrial Contraction (PAC) Multifocal Atrial Tachycardia (MAT) Atrial Fibrillation (A-fib) Atrial flutter (A-flutter) Supraventricular Tachycardia (SVT) Pre-excitation Syndromes (WPW) Multifocal Atrial Tachycardia Three distinct p waves in a narrow complex tachycardia Causes: Almost always associated with pulmonary disease (hypoxia) Less often due to hypokalemia or hypomagnesemia Treatment: Treat the underlying disorder – usually hypoxia Unlike the other atrial tachyarrhythmias, cardioversion is of no value in MAT MAT Rule of Threes 3 different p waves, 3 different pr intervals and 3 different r to r intervals Atrial Fibrillation: Causes Cardiovascular – CAD, HTN, CHF, myopathy, myo-, endo- and pericarditis, infiltrative disease, valvular, congenital Metabolic – thyroid, electrolytes Pulmonary – pulmonary HTN, PE Toxic – cocaine, ETOH (holiday heart), beta agonists Sepsis Idiopathic Atrial Fibrillation: EKGs Regularity – irregularly irregular Rate – atrial rate usually > 350 Controlled – ventricular rate < 100 RVR – ventricular rate > 100 P wave – none discernable, may be flutter waves QRS Less that 0.12 seconds If > 0.12 sec must rule out VT (which is usually more regular) Atrial Fibrillation with RVR Ventricular rate > than 100-120 bpm Patients usually symptomatic requiring rapid treatment Unstable – cardioversion Stable – control rate with calcium channel blockers, beta blockers or digitalis Atrial Fibrillation Treatment Recognize the underlying cause A rate under 120 in an asymptomatic patient generally requires no emergent treatment Unstable patients with acute rapid a-fib should receive synchronized cardioversion with 50-100 J Treatment otherwise depends on the duration Atrial Fibrillation Treatment Less than 48 hours duration Unstable – Cardiovert, synchronized if possible, with 50-100 J May also cardiovert electively in symptomatic, stable patients Pharmacologic cardioversion Procainamide Amiodarone Ibutilide Atrial Fibrillation Treatment Longer duration predisposes the patient to atrial clot formation and failure of conversion Greater than 48 hours duration Rate control with diltiazem, beta blockers or digitalis Do not attempt cardioversion unless emergently indicated Anticoagulation and arrangement for echo Atrial Flutter Patients usually with cardiac or pulmonary disease Conduction through the AV node may be at a 2,3, 4, or 5:1 rate If you see a ventricular rate close to 150, consider atrial flutter Frequently is a transient rhythm which may degenerate into atrial fibrillation or convert to sinus Treatment of Atrial Flutter Unstable – immediate synchronized cardioversion Stable Vagal manuevers – if no carotid bruits Adenosine – will not terminate the atrial tachycardia, but may allow flutter waves to become more apparent Dig, beta blockers or calcium channel blockers for AV nodal blockade to slow the ventricular rate Supraventricular Tachycardia (SVT) AV nodal reentrant tachycardia Usually regular, narrow complex tachycardia without p waves Treatment Adenosine Beta blockers Calcium channel blockers Digoxin SVT – HR around 150s Is it SVT, a-fib, a-flutter, sinus tach? Wolf-Parkinson-White Syndrome Pre-excitation Syndrome AV re-entrant tachycardia (accessory pathway) Short PR interval, delta waves Treatment: Treat like SVT if the QRS is narrow If the QRS is wide or if afib is present, use amiodarone or procainamide Slow the atrial rate and increase conduction through the AV node Avoid ABCD – adenosine, beta blockers, calcium channel blockers, digoxin if wide QRS Narrow complex WPW Wide complex WPW Atrioventricular Blocks •First Degree •Second Degree - Type I •Second Degree - Type II •Third Degree Second Degree AV Blocks Group to group beating Second degree blocks are partial blocks Two types Type I, Mobitz I or Wenckebach – transient Type II, Mobitz II or Classic – often degenerates into 3rd degree heart block Second Degree: Mobitz Type I Decremental conduction: grouped beats with progressively longer PR intervals until an impulse is not conducted (a p without a QRS) Usually narrow QRS May be associated with inferior MI Treatment: Generally requires no treatment Atropine, temporary pacing if symptomatic Second Degree, Mobitz Type II Conduction fails suddenly, no change in the PR interval This is NOT a benign rhythm Often progresses to a complete heart block Associated with anteroseptal MI May have wide QRS Second Degree, Type II: Treatment No pharmacologic treatment Atropine has no effect on the His-Purkinje system and may worsen the conduction ratio Emergency treatment – transcutaneous or transvenous pacing Third Degree Block Complete block – there is total AV Dissociation None of the atrial impulses are conducted through to the ventricles P and QRS are independent, P-P and R-R intervals constant An escape rhythm will drive the ventricles If the escape rhythm originates in the AV junction, the ventricular rate will be in the range of 40-60 with a narrow QRS If the escape rhythm originates in the ventricles, the ventricular rate will be in the range of 20-40 with a wide QRS Third Degree Block: Treatment Although patients may be asymptomatic, transcutaneous or transvenous pacing is warranted Autonomic drugs such as atropine will have no effect on ventricular rate Type I anti-arrhythmics should be avoided as they may suppress the escape rhythm Ventricular Arrhythmias •Premature Ventricular Contraction (PVC) •Ventricular tachycardia (VT) •Ventricular fibrillation (V-fib) PVCs: Causes Generally benign May be a consequence of a pathology, especially if multifocal More concerning causes including hypoxia, ischemia, MI, toxins/drugs, acidosis or alkalosis, hypokalemia Ventricular Tachycardia Results from a dysrhythmia originating at or below the bundle of His Has a wide QRS complex (>0.12 second) May be monomorphic or polymorphic Monomorphic V-tach Morphologically consistent QRS complexes Most common form of V-tach Seen primarily with cardiac ischemia Also seen in cardiomyopathy, valvular disease, electrolyte imbalance, myocarditis Polymorphic V-tach QRS complexes vary in structure and amplitude Predominantly caused by CAD Associated with more severe disease Torsades de Pointes A specific form of polymorphic v-tach Associated with prolonged QT May be due to drugs (tricyclics), electrolyte imbalance (hypo K, Mg or Ca), or subarachnoid hemorrhage V-Tach: Treatment Unstable: Immediate unsynchronized cardioversion 100J, 200J, 300J, 360 J Stable: Amiodorone 150 mg IVP or lidocaine 1 mg/kg Prepare for elective synchronized cardioversion Torsades de Pointes: magnesium sulfate 1-2g IV Ventricular Fibrillation An irregularly irregular rhythm with no p waves or definite QRS complexes Treatment of V Fib Defibrillate Adult: 360/360/360 joules Children: 2 J/kg Epinephrine 1 mg IVP q 3-5 min (0.01 mg/kg) Amiodarone Lidocaine Magnesium Other EKG Abnormalities •Osborne Waves •Brugada Syndrome Osborne Waves Not a true arrhythmia, but an EKG abnormality suggestive of underlying pathology Seen primarily in hypothermia, < 35.6 degrees May also be seen in other conditions, such as hypercalcemia or brain injury Also called J-waves, Camel backs, hathooks Osborne Waves – Hypothermia Osborne Waves – Hypercalcemia Brugada Syndrome Genetic disease – autosomal dominant Mutation in the gene that controls the Na channel Prevalence for Asians Characteristic ECG: ST segment elevation V1-V3 No signs of ischemia Short QT interval Most common cause of sudden death in young males with no underlying cardiac disease Cause of death – polymorphic V-tach or V-fib Treatment: AICD to abort lethal arhythmias Brugada Syndrome: Diagnostic Criteria Type I is the only ECG criterion that is diagnostic of Brugada (see figure). Definitive diagnosis – Type 1 ST-segment is observed in greater than one right precordial lead (V1 to V3) PLUS one of the following: Documented V-fib Polymorphic VT Family history of sudden cardiac death at <45 yo Inducibility of VT with electrical stimulation Coved-type ECGs in family members syncope nocturnal agonal respiration. Brugada Syndrome The End Any Questions?