* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download CVS3_IHDi
History of invasive and interventional cardiology wikipedia , lookup
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Rheumatic fever wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
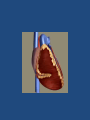
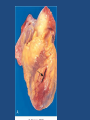
Ischemic Heart Disease CVS3 Hisham Alkhalidi Ischemic Heart Disease A group of related syndromes resulting from myocardial ischemia Ischemic Heart Disease • The vast majority of ischemic heart disease is due to coronary artery atherosclerosis • Less frequent contributions of: – vasospasm – vasculitis • Is it exactly the same as coronary artery disease (CAD)? – Frequently yes Ischemic Heart Disease Angina pectoris • Chest pain: – Can radiate down the left arm or to the left jaw (referred pain) – Due to inadequate perfusion – Duration and severity is not sufficient for infarction Ischemic Heart Disease Stable angina – Occurring reliably after certain levels of exertion – Typically due to atherosclerotic disease with ≥75% (critical stenosis) fixed chronic stable stenosis Ischemic Heart Disease Unstable angina • Unstable (occurring with progressively less exertion or even at rest) • Results from a small fissure or rupture of atherosclerotic plaque triggering: • • • • Platelet aggregation Vasoconstriction Formation of a mural thrombus that may not be occlusive Usually proceed MI Ischemic Heart Disease Variant angina • Vessel spasm or Prinzmetal angina • Without fixed atherosclerotic disease • The etiology is not clear Ischemic Heart Disease Myocardial infarction • The severity or duration of ischemia is enough to cause cardiac muscle death • Typically results from acute thromboses that follow plaque disruption Ischemic Heart Disease MI types • Transmural – Full thickness (>50% of the wall) • Subendocardial – Inner 1/3 of myocardium – Two mechanisms: • Fixed atherosclerosis but with increased demand, vasospasm or hypotension OR • Evolving transmural with relieve of the obstruction (often multifocal) Ischemic Heart Disease MI, common locations – In Right dominent coronary artery heart (90% of population): • 2 cm proximal LAD (up to 50%) – anterior left ventricle – anterior septum – apex circumferentially • Left circumflex ( up to 20%) – infarct involves lateral left ventricle except the apex. • 1st and last thirds of RCA (up to 40%) – posterior left ventricle – posterior septum – right ventricular free wall, sometime Ischemic Heart Disease Ischemia to myocardium rapidly (minutes) leads to loss of function and causes necrosis after 20 to 40 minutes Ischemic Heart Disease Clinical picture of MI • Severe, crushing substernal chest pain or discomfort that can radiate to the neck, jaw, epigastrium, or left arm • Diaphoresis • Nausea • Dyspnea • Can be silent (DM, old age) Ischemic Heart Disease ECG • Changes such as: – Q waves (indicating transmural infarcts) – ST-segment abnormalities – T-wave inversion • Arrhythmias Ischemic Heart Disease Laboratory evaluation • Cardiac troponins T and I (TnT, TnI) • Creatine kinase (CK, and more specifically the myocardial-specific isoform, CK-MB) • Lactate dehydrogenase • Myoglobin Troponins and CK-MB have high specificity and sensitivity for myocardial damage Ischemic Heart Disease Laboratory evaluation • TnI and TnT are not normally detectable in the circulation • After acute MI both troponins: – Become detectable after 2 to 4 hours – Peak at 48 hours – Their levels remain elevated for 7 to 10 days Ischemic Heart Disease Laboratory evaluation • CK-MB is the second best marker • CK-MB activity: – Begins to rise within 2 to 4 hours of MI – Peaks at 24 to 48 hours – Returns to normal within approximately 72 hours Ischemic Heart Disease Complications of MI • At least 80% will suffer: – Cardiogenic shock (>40% infarct of LV) – Congestive heart failureCHF – Arrhythmia – Rupture of ventricle, free wall, septum, or papillary muscle – Aneurysm formation, – Mural thrombus, potentially soursce of emboli – Pericarditis Ischemic Heart Disease MI death and complications rates • • • • 25% die, presumably due to arrythmia 10% of the rest will die within a month 80-90% will develop complications Overall 30% die in the 1st year and then 10% per year Chronic ischemic heart disease • Progressive heart failure due to ischemic injury, either from: – prior infarction(s) (most common) – chronic low-grade ischemia Ischemic Heart Disease Sudden cardiac death • Unexpected death from cardiac causes either without symptoms or within 1 to 24 hours of symptom onset (different authors use different time points) • Results from a fatal arrhythmia, most commonly in patients with severe coronary artery disease Ischemic Heart Disease Acute coronary syndrome • is applied to three catastrophic manifestations of IHD: – Unstable angina – Acute MI – Sudden cardiac death