* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 2-Feldman Presentation
Survey
Document related concepts
Remote ischemic conditioning wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Baker Heart and Diabetes Institute wikipedia , lookup
Myocardial infarction wikipedia , lookup
Coronary artery disease wikipedia , lookup
Transcript
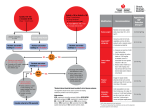
Management of Patients with Hypertension; Defining the Barriers to Control David Feldman, MD/PhD, FACC, FAHA Director of Heart Failure and Cardiac Transplantation The Ohio State University Hypertension Pre-Test Questions ? Management of Patients with Hypertension; Defining the Barriers to Control David Feldman, MD/PhD, FACC, FAHA Director of Heart Failure and Cardiac Transplantation The Ohio State University Learning Goals Recognize the economic burden of hypertension. Understand that hypertension is an antecedent to many cardiovascular events. Aggressive screening and management is required to reach the goals of the evidencebased guidelines. Recognize some of the most important barriers to overcome in order to improve blood pressure control. Explore therapeutic combinations that can prevent disease progression and improve morbidity and mortality. ? Significance of Hypertension •HTN affects approximately 50 million individuals in the US and 1 billion people worldwide. • HTN is the most common primary diagnosis in the USA with 35 million office visits per year. • Framingham Heart Study—Individuals who are normotensive at 55 years of age have a 90% lifetime risk of developing HTN • Relationship between BP and risk of CVD is continuous, consistent, and independent of other risk factors • Only 35% of hypertensive patients on treatment are under control. • For those age 40-70, each increased increment of 20 mmHg in systolic BP or 10 mmHg in diastolic BP doubles the risk of CVD across the entire BP range of 115/75 to 185/115. JNC 7: U.S. 90% lifetime risk for men who reach age 55 and women who reach age 65. Prevalence is 33.1% (65 million). 2004 direct costs = $55.5 Billion If co-morbidities are added (ESRD, CAD, CHF, DM, CVA) cost is $108 Billion. JNC 7 U.S.; Are you Surprised? 30% of adults do not know they have hypertension. 40% of those who are hypertensive are not on treatment. 66% of those who are being treated have a BP greater than 140/90 mmHg. ? Co-morbidities Which of these co-morbidities are most prevalent in your practice? 1. 2. 3. 4. Diabetes Heart Failure Renal Insufficiency Coronary Artery Disease Benefits of Lowering Blood Pressure •Anti-HTN Therapy associated with: • 35 – 40% mean decrease in stroke • 20 – 25% decrease in MI • More than 50% decrease in HF •Patients with Stage 1 HTN/Additional Risk Factors: • Achieving a sustained 12 mmHg decrease in systolic BP 10 years will prevent 1 death for every 11 pts treated •The majority of Patients will require 2 or more anti-HTN drugs. JNC 7: Treatment Algorithm for Hypertension Lifestyle modifications Not at goal blood pressure (<140/90 mm Hg) (<130/80 mm Hg for those with diabetes or chronic kidney disease) Initial drug choices Without compelling indications Stage 1 hypertension (SBP 140–159 or DBP 90–99 mm Hg) Thiazide-type diuretic for most. May consider ACEI, ARB, BB, CCB, or combination. Stage 2 hypertension (SBP 160 or DBP 100 mm Hg) Two-drug combination for most (usually thiazide-type diuretic and ACEI or ARB or BB or CCB). With compelling indications Drugs for compelling indications Other antihypertensive drugs (diuretic, ACEI, ARB, BB, CCB) as needed. Not at goal blood pressure Optimize dosages or add additional drugs until goal blood pressure is achieved. Consider consultation with hypertension specialist. SBP=systolic blood pressure; DBP=diastolic blood pressure; ACEI=angiotensinconverting enzyme inhibitor; ARB=angiotensin receptor blocker; BB=b-blocker; CCB=calcium channel blocker JNC 7. May 2003. NIH publication 03-5233. ? JNC 7: The Fine Print Cracking open the door beyond diuretics for first line in a patient without co-morbid conditions Along with promoting a thiazide diuretic for Stage 1 HTN, the committee added this surprising sentence: “May consider ACEI, ARB, BB, CCB.” The ‘Compelling Indication’ Category - JNC put emphasis on evidence showing benefits with specific antihypertensive agents for certain medical conditions. Again, taking a small sidestep from the NHLBI dictum of diuretics first. Case PresentationPrehypertension: The Executive Physical Vicki Struthers 36 White Female Presents for an Executive Physical PMH Recently returned to work 10 weeks after the birth of first child Total Cholesterol: 160 mg/dL HDL 66 mg/dL; Low-density lipoprotein (LDL): 120 mg/dL Family History of Diabetes Mellitus No History of Smoking *Hypothetical case based on a typical patient expected to present in clinical practice Vicki Struthers – by the numbers Tests Ordered Before Your Visit Today ECG- LBBB, CR 0.9 mg/dL, NA 135 mmol/L, Glucose 97 mg/dL, HCT 35, TSH 2.1, Labs Vitals HR 98 bpm, BP 148/91 mm/Hg, BMI 23 No Rx, NKDA Vicki Struthers –Parasternal Long Axis Echo What Should We Be Thinking About? ? Vicki Struthers 12 Years Later At 1 YR- “I take my medicine”, Structured Exercise program Law salt, Low fat Diet AT 12 YRS- Running 10Ks, Daughter in Middle school. Blood Pressure 118/70 WHAT SHOULD WE BE THINKING ABOUT? Clinical Practice Recommendation Exercise may be beneficial in lowering blood pressure and reducing cardiovascular risk. Strength of Evidence: Three reviews of 50 observational studies found the risk of CV disease was lowered in those who were physically active. Conversely, a review of 43 epidemiological studies found that physical inactivity was associated with a doubling of cardiovascular disease. Key Diet History Questions for Patients with HTN Do you use a salt shaker? Do you taste your food before you add salt? How often do you eat salty foods, such as chips, pretzels, salted nuts, canned and smoked foods? Do you read labels for sodium content? How many servings of fruits and vegetables do you eat everyday? How often do you eat or drink dairy products? What kind? How often do you eat out? What kinds of restaurants? Do you like to drink alcohol? How much? How often do you exercise, including walking? ? When the First Drug Doesn’t Work JNC 7 pushes for rapid progression to combination therapy before fully exploring mono-therapy. This approach is not an issue for those with Stage 2, but for Stage 1. Different mechanisms may cause HTN in different patients; and heterogeneous mechanisms from multiple class of agents may be necessary. Alternative approach: if there is a partial response, then increase the dose or add a second agent. If there is no response at all, then try an alternate class. The goal here being to find the simplest way to control BP. JNC 7: Classification and Management of Blood Pressure for Adults Initial Drug Therapy BP Classification SBP* (mm Hg) DBP* (mm Hg) Lifestyle Modification Normal <120 and <80 Encourage 120–139 or 80–89 Yes Prehypertension Stage 1 hypertension Stage 2 hypertension 140–159 160 or 90–99 or 100 Without Compelling Indications No antihypertensive drug indicated. Yes Thiazide-type diuretic for most. May cosider ACEI, ARB, BB, CCB, or combination. Yes Two-drug combination for most (usually thiazide-type diuretic and ACEI or ARB or BB or CCB). JNC 7. May 2003. NIH publication 03-5233. With Compelling Indications Drug(s) for compelling indications. Drug(s) for compelling indications. Other antihypertensive drugs (diuretic, ACEI, ARB, BB, CCB) as needed. Case Presentation #2 Nate Biddleson 55 AA male presents for follow-up after his original Executive Physical. PMH Blood pressure on presentation 145/95, now 140/90 Non-smoker , no Known CAD Fasting glucose 142 (repeated from previous visit) Initial Therapy; Diet modification, Increased exercise, take “some vacation”, and started 25 mg of HCTZ ? What Other Risk Stratification Should I Do at this Juncture to Proactively Assess my Patient? Nate Biddleson 55 AA male presents for follow-up 6 months after his last appointment PMH Blood pressure on presentation 125/75 Fasting glucose 98 Therapy; Salt modification, Increased exercise, HCTZ 12.5 mg, CCB, ACEI and sulfonourea/metformin combination. High-Risk Hypertensive Patients Require Multiple Agents to Get to Goal Achieved Systolic BP AASK1 (134 mm Hg) ABCD2,3 (132 mm Hg) ALLHAT4 (135 mm Hg) HOT2,5 (141 mm Hg) IDNT6 (140 mm Hg) RENAAL7 (140 mm Hg) UKPDS2,8 (144 mm Hg) 1 2 3 4 Number of BP Medications AASK=African-American Study of Kidney Disease and Hypertension; ABCD=Appropriate Blood Pressure Control in Diabetes; ALLHAT=Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trials; HOT=Hypertensive Optimal Treatment; IDNT=Irbesartan Diabetic Nephropathy Trial; RENAAL=Reduction of Endpoints in Non-Insulin Diabetes Mellitus with the Angiotensin II Antagonist Losartin; UKPDS=United Kingdom Prospective Diabetes Study. 1Wright JT et al. JAMA. 2002;288:2421-2431. 2Bakris GL. J Clin Hypertens. 1999;1:141-147. 3Estacio RO et al. N Engl J Med. 1998;338:645-652. 4The ALLHAT Officers and Coordinators. JAMA. 2002;288:2981-2997. 5Hansson L et al. Lancet. 1998;351:1755-1762. 6Lewis EJ et al. N Engl J Med. 2001;345:851-860. 7Bakris GL et al. Arch Intern Med. 2003;163:1555-1565. 8UK Prospective Diabetes Study Group. BMJ. 1998;317:703-713. Compelling Indications for Consideration of One Drug Class vs. Another Heart Failure: Post- MI: Thiazide/loop, BB, ACEI, ARB, Aldosterone antagonist BB, ACE, Aldosterone antagonist High CVD risk: Thiazide, BB, ACE, ARB DM: Thiazide, BB, ACE, ARB, CCB ACE, ARB. For creatinine 2-3 try CRF loop diuretic Cr > 1.5 in men Cr > 1.3 in women Thiazides Chlorothiazide (Diuril) Chlorthalidone Hydrochlorthiazide (Microzide, Hydrodiuril) Polythiazide (Renese) Indapamide (Lozol) Metolazone (Mykrox, Zaroxolyn) *All trade / brand / generic names are specific to the USA Loop Diuretics • Bumetanide (Bumex) • Furosemide (Lasix) • Torsemide (Demadex) Potassium-sparing Diuretics • Amiloride (Midamor) • Triamterene (Dyrenium) *All trade / brand / generic names are specific to the USA Aldosterone Receptor Blockers • Eplerone (Inspra) • Spironolactone (Aldactone) Combined a and b-blockers • Carvedilol (Coreg) • Labetalol (Normodyne, Trandate) *All trade / brand / generic names are specific to the USA Beta-Blockers Atenolol Betaxolol Bisoprolol Metoprolol XL) Nadolol Propranolol Timolol Nebivolol (Tenormin) (Kerlone) (Zebeta) (Lopressor, Toprol (Corgard) (Inderal/XL) (Blocadren) (Bystolic) *All trade / brand / generic names are specific to the USA ACE Inhibitors Benzapril Captopril Enalpril Fosinopril Lisinopril Moexipril Perindopril Quinapril Ramipril Trandolapril (Lotensin) (Capoten) (Vasotec) (Monopril) (Prinivil, Zestril) (Univasc) (Aceon) (Accupril) (Altace) (Mavik) *All trade / brand / generic names are specific to the USA Angiotensin II Receptor Blockers Candesartan (Atacand) Eprosartan (Tevetan) Irbesartan (Avapro) Losartan (Cozaar) Olmesartan (Benicar) Telmisartan (Micardis) Valsartan (Diovan) *All trade / brand / generic names are specific to the USA Calcium Channel Blockers Dihydropyridines Amlodipine (Norvasc) Felodipine (Plendil) Isradipine (Dynacirc) Nicardipine (Cardene SR) Nifedipine (Adalat, Procardia) Nisoldipine (Sular) • DHPs have been particularly known to have a negative inotropic effect. Calcium Channel Blockers Non-Dihydropyridines: Diltiazem (Cardizem, Dilacor, Tiazac) Verapamil (Calan, Isoptin) Constipation Conduction Abnormalities *All trade / brand / generic names are specific to the USA Alpha1 Blockers Doxazosin Prazosin Terazosin Direct Vasodilators Hydralazine (Apresoline) Minoxidil (Loniten) (Cardura) (Minipress) (Hytrin) *All trade / brand / generic names are specific to the USA Centrally Acting Drugs Clonidine Methyldopa Reserpine Guanfacine (Catapres) (Aldomet) (generic) (generic) *All trade / brand / generic names are specific to the USA ? ACC/AHA Practice Guidelines Pyramid Approach to HF Stages Refractory End-Stage HF Marked symptoms at rest despite maximal medical therapy* D HF with Current or Prior Symptoms C Known structural heart disease Shortness of breath and fatigue Reduced exercise tolerance Structural Heart Disease B Previous MI LV systolic dysfunction Asymptomatic valvular disease High Risk for Developing HF A Hypertension CAD Diabetes mellitus Family history of cardiomyopathy Hunt et al., Journal of American College of Cardiology. 2005;38:1116-43 ? Case Number Three Clark Galloway 42 White Male Presents for a Executive Physical Past Medical History (PMH) “Borderline” Hypertension (HTN) “…too Busy to Exercise” Cholesterol Total: 223 mg/dL High-density lipoprotein (HDL): 24 mg/dL Parents deceased related to “some heart failure thing” +TOB (smoker) *Hypothetical case based on a typical patient expected to present in clinical practice Clark Galloway – by the numbers Tests Ordered Before Your Visit Today ECG (electrocardiogram)- normal sinus rhythm (NSR), No Q wave, normal intervals, No STT Abnormalities Echocardiogram (Echo) -next slide Serum Creatinine (SCr) 1.1mg/dL, Sodium (Na) 140 mmol/L, Fasting Glucose 140 mg/dL, Hematocrit (HCT) 44, Thyroid-Stimulating Hormone (TSH) 1.1, Fasting Blood Glucose taken on two separate days 128 mg/DL and 138 mg/DL Labs Vitals Heart Rate: 82 beats per minute (bpm), Blood Pressure: 142/86 mmHg, Body Mass Index (BMI): 26 No Prescription Medicine (Rx), No Known Drug Allergies (NKDA) Clark Galloway –Parasternal Long Axis Echo ? What Lifestyle changes should we ask him to consider and should we start any medications at this time? Clark Galloway 12 Years Later At 1 YR- “I was too busy to exercise and I don’t like medicine… I felt fine” AT 5 YRS- Promoted, gained 15 lbs, and joined a cigar club AT 8 YRS- First MI, LVD, uncontrolled DM, ED AT 12 YRS- Next Appt. with you. ? New Medical Profile Left Ventricular Ejection Fraction (LVEF) <20% VO2 MAX 11 BP 108/50 mmHg, HR 95 bpm Shortness of Breath (SOB) at rest, Chest Pain (CP) 2-3/day, Paroxysmal nocturnal dyspnea (PND) 9 kg weight gain despite two calls to office this wk ACC/AHA Practice Guidelines Pyramid Approach to HF Stages Refractory End-Stage HF Marked symptoms at rest despite maximal medical therapy* D HF with Current or Prior Symptoms C Known structural heart disease Shortness of breath and fatigue Reduced exercise tolerance Structural Heart Disease B Previous MI LV systolic dysfunction Asymptomatic valvular disease High Risk for Developing HF A Hypertension CAD Diabetes mellitus Family history of cardiomyopathy Hunt et al., Journal of American College of Cardiology. 2005;38:1116-43 Hypertension in Patients With HighRisk Conditions ~3/4 of adults with diabetes have BP 130/80 mmHg or use prescription medications for HTN1 ~2/3 of patients with HF have a past or current history of HTN2 More than 50%–75% of patients with chronic kidney disease have BP >140/90 mmHg3 1. National Institute of Diabetes and Digestive and Kidney Diseases. National Diabetes Statistics. Bethesda, MD: US Department of Health and Human Services, NIH, 2005. Available at http://diabetes.niddk.nih.gov/dm/pubs/statistics/index.htm. Accessed Oct. 2006. 2. Hunt SA et al. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult. Available at http://www.acc.org/qualityandscience/clinical/guidelines/failure/update/index.pdf. Accessed Oct. 2006. 3. National Kidney Foundation. Kidney Disease Outcomes Quality Initiative (K/DOQI) Clinical Practice Guidelines on Hypertension and Antihypertensive Agents in Chronic Kidney Disease. Available at http://www.kidney.org/professionals/KDOQI/guidelines_bp/guide_1.htm. Accessed Oct. 2006. Chronic Kidney Disease Goals: 1) Slow deterioration of renal function 2) Prevent CVD • Often need 3 or more drugs • Target < 130/80 • Drugs: ACE-Inhibitors/ARBs—Favorable effects on progression -- Increase in Creatinine of 35% is acceptable • Advanced Renal Disease: GFR < 30, CR 2.5 – 3.0 mg/dl Increased dose of loop diuretics usually needed in combo with other drugs Incidence of Coronary Heart Disease (CHD) Events in Patients With and Without Diabetes P<.001 50 45.0 Incidence During 7-Year Follow-up* (%) Nondiabetics with no prior MI 40 30 Nondiabetics with prior MI Diabetics with no prior MI Diabetics with prior MI P<.001 18.8 20.2 n=69 n=1,304 n=169 n=890 3.0 0.5 7.8 3.2 20 10 3.5 0 Events per 100 Person-years *Among 1373 nondiabetic subjects and 1059 diabetic subjects, from a Finnish population-based study. Haffner SM et al. N Engl J Med. 1998;339:229-234. Causes of Death in Persons With Diabetes, Based on US Studies Cardiac Disease Cerebrovascular Disease Diabetes Malignant Neoplasms Pneumonia/Influenza All Other 0 10 20 1990 US death certificates with mention of diabetes, all ages. 1990 US death certificates with mention of diabetes, age at death 45 years. 30 Deaths (%) 40 50 Moss SE et al. Am J Public Health. 1991;81:1158-1162. Ochi JW et al. Diabetes Care. 1985;8:224-229. Kleinman JC et al. Am J Epidemiol.1998;128:389-401. Bender AP et al. Diabetes Care.1986;9:343-350. 60 The Diabetic Hypertensive Patient Is at Especially High Risk… For CV disease For myocardial infarction (MI) “Two thirds to three fourths of people with diabetes mellitus die of some form of heart or blood vessel disease”1 Patients with diabetes without a previous MI have as high a risk of MI as patients without diabetes with a previous MI2 For congestive heart failure (CHF) In the DIGAMI trial, 66% of total mortality among patients with diabetes was due to HF3 DIGAMI=Diabetes Insulin-Glucose Infusion in Acute MI. American Heart Association. Heart and Stroke Statistical—2004 Update. Dallas, TX: AHA; 2003; 2Haffner SM et al. N Engl J Med. 1998;339:229-234; 3Malmberg K et al. Eur Heart J. 1996;17:1337-1344. UKPDS: Blood Pressure Control Study in Type 2 Diabetes Effect of Intensive BP Lowering on Microand Macrovascular Complications Risk 0 MI Any Diabetesrelated Endpoint Diabetesrelated Death Retinopathy Renal Failure Stroke Vision Deterioration HF Risk Reduction (%) -10 -20 21 -30 -40 P=.13 24 P=.0046 32 P=.019 34 P=.0038 42 P=.29 -50 44 P=.013 47 P=.0036 -60 Benefits of 144/82 vs 154/87 -70 1,148 hypertensive patients with type 2 diabetes were allocated to tight (144/82 mm Hg, n=758) or less tight (154/87 mm Hg, n=390) and followed for a median of 8.4 years. UKPDS Group. UKPDS 38. BMJ. 1998;317:703-713. 56 P=.0043 UKPDS: Benefits of Glycemic vs BP Control With ACEIs or b-Blockers 20 Risk of Event (%) HF Stroke MI Diabetic Death 0 +7 -8 -9 -12 -20 -21 -32 -40 -44 Glycemic control -60 -56 ACEI or b-Blocker ACEI=Angiotensin-converting enzyme inhibitor. UKPDS Group. BMJ. 1998;317:703-713. Lancet. 1998;352:837-853. ? Clinical Practice Recommendation Treating high blood pressure to JNC-7 GOALS with anti-hypertensive medications reduces the risk of cardiovascular disease and death. Strength of Evidence: Level of Evidence 1 Grade A ? Clinician Input When we first encountered Clark, what are the things we could have done that would have made a difference?” AND “Do you have patients like Clark in your practice?” Failures of Patient Education 50% of patients discontinue their antihypertensive within one year of initiating treatment. DASH diet for hypertension: limit sodium Increase fruits and vegetables (8-10/d) Increase low fat dairy (3-4/d) Focus on diet history for hypertensive patients Noncompliance Estimates of noncompliance with medical treatment in general: Noncompliance causes 125,000 deaths a year twice the mortality rate from MVAs 30% of hospital admissions for people over the age of 65 are directly caused by noncompliance. Half of all prescriptions are taken incorrectly, contributing to prolonged or additional illnesses. Noncompliance increases with the number of meds and doses per day; at 4 times a day, only 40% get it right. Selected Factors that Influence Dissemination and Implementation of Healthcare Systems of Care Access to care Coverage Marketing influences Provider Lack of knowledge Lack of conviction Forgetfulness Innovation bias Marketing influences Patient Level Preferences Symptoms Marketing Influences Differences Between More and Less Successful Providers More Successful Less Successful Involved patients in decision-making. Referenced technical aspects of drug benefits. Used med changes to educate / engage. Patient-maintained record card to monitor compliance. Less information sharing – “only if asked”. Felt time constraint did not permit Progressively introduce effective dose discussing adverse effects of meds. and number of meds. Awareness of patient ability to afford / role of formulary (e.g., VA) Least expensive appropriate med when possible. Greater attention to gender, comorbidities, age when prescribing. Felt knowledge of side effects would hinder compliance. Shared Traits of More and Less Successful Providers Several BP readings to confirm HTN, multiple visits. Unless BP very high or comorbidities present. High awareness of national BP guidelines. Concurrence on HTN treatment goals, especially for comorbidities, e.g., diabetes, etc. Likely to begin HTN treatment with 2-3 months of lifestyle management. Not sufficient to attain desired BP Difficulty / reluctance in treating older patients to JNC standards. Questioned value of aggressively treating older (80+ years) patients with other severe problems Would look at any BP reduction as partial success Causes of Resistant HTN Improper Measurement Volume Overload Excess Sodium Volume retention from Renal Disease Inadequate Diuretic Therapy Drug-Induced/Other Causes Noncompliance Inadequate Doses Inappropriate Combos NSAIDS; COX 2 inhibitors Cocaine, amphetamines, other illicits Sympathomimetics (decongestants etc.) OCPs Steroids Erythropoietin Cyclosporine and tacrolimus Licorice Ephedra ma haung Bitter Orange Obesity EtOH Additional Challenge in Treatment of HTN: Medication Adherence Adherence to a drug regimen is an important component of BP control Approximately 50% of patients with poor BP control have adherence problems (defined by taking <80% of medication) Several drug-related factors can influence medication adherence, including: Adverse events Frequency of adverse events has been inversely correlated with adherence rates Dosing frequency Reduction in dose frequency can lead to improved adherence Feldman R et al. Can J Public Health. 1998;89:I-16–I-18. Strategies to Improve Management of Patients With HTN and DM ACC/AHA HF Guidelines1 In-hospital Initiation2,3 Increasing Outpatient Compliance2,3 I IIa IIb III • Clinical trial evidence incorporated into recommendations for patient care • Implement evidence-based care and therapies • Majority of patients eligible for treatment • Early benefit of therapy not missed • Higher persistence rates postdischarge • Improve quality of care and outcomes 1. Hunt SA et al. Circulation. 2005;112:1825–1852. 2. Fonarow GC. Rev Cardiovasc Med. 2002;3:S2–S10. 3. Gattis W et al. J Am Coll Cardiol. 2004;43:1534–1541. Improved Adherence Has Been Associated With Improved Outcomes In the BHAT trial, patients who took 75% of their prescribed βblocker regimen were 2.6 times more likely to die within the first year of follow-up, compared with more compliant patients1 In the COMPASS study, patients treated with oral nitrates had better efficacy with once-daily dosing2 Mean weekly number of chest pain episodes: 94% decrease in once-daily group 30% decrease in twice-daily group (P<.0001 compared to oncedaily group) Beta-Blocker Heart Attack Trial (BHAT): multicenter, randomized, double-blind trial comparing propranolol vs placebo in 3837 patients aged 30–69 years surviving acute MI. Patients 5–21 days post-MI were randomized to propranolol or placebo and were followed for an average of 25 months. Adherence data were available for 2175 patients (1081 randomized to propranolol). Compliance With Oral Mononitrates in Angina Pectoris Study (COMPASS): open, nonblinded, randomized, parallel-group study in 101 patients aged 40–75 years; compared patient compliance (using electronic measurement) and treatment effectiveness in patients with stable angina pectoris treated with oral nitrates administered once daily vs twice daily. 1. Horwitz R et al. Lancet. 1990;336:542–545. 2. Kardas P et al. Am J Cardiol. 2004;94:213–216. SUMMARY-CHALLANGE 1. Every patient in my practice will be screened for hypertension. 2. I understand that hypertension is a significant risk factor for cardiovascular disease. 3. Every patient in my practice will be treated to goal to decrease the risk of CV death. 4. My treatment plans will include helping patients comply with lifestyle and medication changes. I will make an extra effort to demonstrate to my patients how important their hypertension is to me and will provide additional time if needed. JNC-7 The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Full text available: Hypertension, 2003;42:1206-1252 References • JNC 7 report: available via NIH (Publication 035233) • JAMA 289 (19), May 21 2003 (online) • Adapted slides from Dr. Omar Khan’s AAFP 01/2006 update (online) • AAFP monograph: #305 • AHA/ACC Hypertensive Guidelines • Weber, MA. The JNC 7 Report: Challenges and Dilemmas in Writing Guidelines. J. Clin Htn.;5(4):p282, 2003. Hypertension Post-Test Questions ?





















































































![[ Insert Title Here ]](http://s1.studyres.com/store/data/008479268_1-03ff748536c27aeae665c17a72e89ec4-150x150.png)