* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Edwards syndrome
Saethre–Chotzen syndrome wikipedia , lookup
Nutriepigenomics wikipedia , lookup
Medical genetics wikipedia , lookup
Frontonasal dysplasia wikipedia , lookup
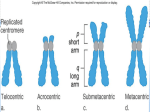
Neocentromere wikipedia , lookup
DiGeorge syndrome wikipedia , lookup
Fetal origins hypothesis wikipedia , lookup
Turner syndrome wikipedia , lookup
Down syndrome wikipedia , lookup
Imad Fadl-Elmula Nondisjunction History Independently described by: 1. Edwards et al., 1960. 2. Smith et al., 1960. Incidence Incidence Trisomy 18 is the second most common autosomal trisomy after trisomy 21. 1 in 6000-8000 live births. Morbidity Approximately 95% of conceptuses with trisomy 18 die in embryonic or fetal life. 5-10% of affected children survive beyond the first year of life. Race No racial predilection exists. Sex Females compose about 80% of cases. Age Trisomy 18 is detectable during the prenatal and newborn periods. The high mortality rate is often due to: 1. Cardiac and renal malformations. 2. Feeding difficulties. 3. Sepsis. 4. Apnea caused by CNS defects. Trisomy 18 in 95% of cases. Mosaicism 46,XY/47,XY,+18 Translocation trisomy gives rise to partial trisomy 18 syndrome. Origin of trisomy 90% of trisomies are maternal in origin. 10% of trisomies are paternal in origin. Meiosis II errors occurring twice as frequently as meiosis I errors. Mechanisms While full trisomy results from meiotic nondisjunction. Mosaic trisomy is due to postzygotic mitotic nondisjunction. Translocation trisomy gives rise to partial trisomy 18 syndrome. The smallest extra region necessary for expression of serious anomalies of trisomy 18 appears to be 18q11-q12. Phenotype The clinical is variable depending on the level of mosaicism and the tissue involved. Trisomy 18 severely affects all organ systems In translocations that result in partial trisomy or in cases of mosaic trisomy 18. Clinical expression is less severe and longer survival is usual. Edwards Syndrome (47,+18) Phenotype Short sternum. Narrow pelvis. Limited hip abduction Hypoplastic nails. Dorsiflexed great toes. Short neck with excessive skin folds. An infant with Edwards syndrome Characteristic hand posture (Clenched hands) The index finger overriding the middle finger. The fifth finger overriding the fourth finger). Rocker-bottom foot with prominent calcaneus The hands of a fetus with Edwards syndrome Note typically manifests overlapping digits with the second and fifth fingers overriding the third and fourth fingers respectively. Overall posturing of the wrists and fingers suggests contractures. Diagnosis Conventional cytogenetic studies Full trisomy 18 (95% of cases). Trisomy 18 mosaicism (5% of cases) Translocation (very rare). Prenatal diagnosis Percutaneous umbilical blood sampling (PUBS) Percutaneous umbilical blood sampling (PUBS) is of limited use, except in cases detected late in pregnancy. The preimplantation diagnosis is not of any realistic relevance for current care Chorionic villus sampling (CVS) Is performed at 10-13 weeks’ gestation. The accuracy (96-98%) is less than that of mid trimester amniocentesis because of confined placental mosaicism and maternal cell contamination. Congenital anomalies detectable by prenatal ultrasonography Renal defects Omphalocele Cardiac defects Neural tube defects Choroid plexus cysts 2-vessel umbilical cord Abnormally shaped fetal head Intrauterine growth retardation Abnormal position of fetal fingers Oligohydramnios/polyhydramnios Cystic hygroma or lymphangiectasia 9%. 20% 37% 9% 43% 40% 43% 29% 89% 12%. 14% Genetic counseling Recurrence risk is 1% for full trisomy 18. If a parent is a balanced carrier of a structural rearrangement, the risk is substantially high. Risk should be assessed based on the type of structural rearrangement. Consultations Clinical geneticist. Developmental pediatrician. Cardiologist. Ophthalmologist. Orthopedist. Psychologist. Speech language pathologist. Audiologist. Early childhood educational programs. Medical/Legal Pitfalls Failure to identify characteristic symptoms and signs of Edwards syndrome and refer to a geneticist for evaluation and genetic counseling Failure to request chromosome analysis with clinical diagnosis of Edwards syndrome Failure to offer prenatal screening for pregnant women Failure to offer prenatal diagnosis after birth of an affected child Delayed psychomotor development. Mental retardation (100%). Neonatal hypotonia followed byhypertonia. Malformations Microcephaly. Cerebellar hypoplasia. Meningoencephalocele. Hydrocephaly. Holoprosencephaly. Frontal lobe defect. Migration defect. Arachnoid cyst. myelomeningocele. Cranial Microcephaly. Elongated skull. Narrow bifrontal diameter. Wide fontanels. Prominent occiput. Cardiac malformations in 90% of infants. Ventricular septal defects. Pulmonary and aortic valve defects. Atrial septal defects. Patent ductus arteriosus. Overriding aorta. Coarctation of aorta. Hypoplastic left heart syndrome. Tetralogy of Fallot. Transposition of great arteries. Endocrine Thymic hypoplasia. Thyroid hypoplasia. Adrenal hypoplasia. Gastrointestinal Malrotation of the intestine. Ileal atresia and Meckel diverticulum. Esophageal atresia with or without tracheoesophageal fistula and omphalocele. Diaphragmatic eventration. Prune belly anomaly and absent appendix. Diastasis recti and absent gallbladder. Accessory spleens and pilonidal sinus. Exstrophy of Cloaca and pyloric stenosis. Imperforate or malpositioned anus. Umbilical, inguinal, and diaphragmatic hernias. Urinary System Bifid uterus. Hydroureters. Double ureters. Megaloureters. Hydronephrosis. Horseshoe kidneys. Unilateral renal agenesis. Micromulticystic kidneys. Hypospadias. Bifid uterus. Cryptorchidism. Micropenis in males. Hypoplastic ovaries. Hypoplasia of labia and ovaries. Clitoral hypertrophy in females. Surgical Care Because of the extremely poor prognosis, surgical repair of severe congenital anomalies such as esophageal atresia or congenital heart defects is not likely to improve the survival rate of infants and should be discussed with families. Prognosis Survival rates Newborns have a 40% chance of surviving to age 1 month. Infants have a 5% chance of surviving to age 1 year. Children have a 1% chance of surviving to age 10 years.