* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Clinical Manifestation
Cardiovascular disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Aortic stenosis wikipedia , lookup
Cardiac surgery wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Myocardial infarction wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Islamic University of Gaza
Faculty of Nursing Pediatric Nursing
Dr. Areefa Albahri
• Cardiovascular disease is a significant cause of
chronic illness and death in children.
• Typically cardiovascular disorders in children are
divided into two major categories:
• Congenital heart disease is defined as structural
anomalies that are present at birth. CHD accounts for
the largest percentage of birth defects
• Acquired heart disease includes disorders that occur
after birth. These disorders develop from a wide
range of causes, or they can occur as a complication
of CHD.
Congenital Heart Defects
• Is a structural malformation of the heart or great vessels
presents at birth. Generally blood flows from areas of high
pressures to areas of low pressures.
• Etiology: exact cause is unknown.
• 1. Maternal infection as rubella
• 2. Poor nutrition of mother.
• 3. Diabetic mothers
• 4. Maternal alcoholism.
• 5. Maternal exposure to radiation
• 6. Genetic defect
Types of Defects:• 1. Acyanotic Heart Defects: there is no mixing of
unoxygenated blood with systemic circulation
(Oxygenated blood), its take one of the following
forms:
• a. Dextracardia ―as a part of situs inversus ―
• b. Obstructive lesion as: aortic stenosis, pulmonary
stenosis and coarctation of the aorta.
• c. Left to Right shunts as: patent ductus arteriosus,
atrial septal defect and ventricular septal defect.
• 2.
Cyanotic heart defect: un-oxygenated blood
enters the systemic circulation (Right to Left shunt)
• a. Tetralogy of Fallot.
• b. Transposition of great arteries.
• c. Tricuspid atresia.
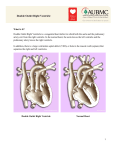
• A cyanotic Heart Defects
• I. Dextracardia with Situs Inversus
• Dextracardia indicates that the heart is in the right side of
thorax cavity. This condition is frequently associated with situs
inversus within abdominal and thoracic organs transposed to
opposite side of the body. There are usually no cardiac
defects.
• Diagnosis:
• 1. Clinically: apex beat on the right side, stomach {percussion}
on right side, the liver on the left side.
• 2. Electrocardiograph: lead I shown a mirror image with
inverted P and T waves.
• 3. X-ray: situs inversus.
II. Aortic Stenosis
• Aortic stenosis (AS) is a narrowing or a
stricture of the aortic valve that results in:
• Increase left ventricular pressure to overcome
the obstructed valve
• Left ventricular hypertrophy, myocardial
ischemia and decreased cardiac output.
• Imbalance between the increased O2
requirements and the amount of O2 supplied.
Clinical Manifestations
• Rarely symptomatic during infancy, in severe cases infant may
demonstrate evidence of decreased cardiac output such as faint
peripheral pulses or exercise intolerance.
• Older children may experience chest pain, dyspnea and fatigue
with exertion.
• Narrow pulse pressure and weak peripheral pulses.
• X-ray may show normal heart to varying degrees of left
ventricular hypertrophy.
• A harsh ejection systolic murmur is best heard in the aortic area.
• E.C.G.: left ventricular hypertrophy {T. wave inversion}.
• Diagnosis: Cardiac Catheterization.
• Complications: CHF, MI, bacterial endocarditis and death.
• Treatment: Surgery: Balloon angioplasty or valvulotomy
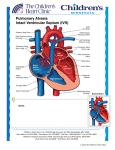
III. Pulmonary Stenosis
• Refers to narrowing of the opening to the pulmonic
valve, that cause obstruction to blood flow, so the
right ventricle has an additional work-load, causing
the muscle to thicken, resulting in right ventricular
hypertrophy and decreased pulmonary blood flow.
• Signs and symptoms: Generally asymptomatic
unless in severe stenosis
• Dyspnea, fatigue and systolic ejection murmur over
the pulmonic area.
• Complication: anoxic spells, bacterial endocarditis,
death. ―Heart Failure
• Diagnosis: Cardiac Catheterization.
• Treatment: Pulmonary valvotomy or dilation by balloon.
• IV. Coarctation of the Aorta
• Is a narrowing or constriction of the
vessel at any point. Most common,
The narrowing can be pre-ductal
(between the subclavian artery and
ductus arteriosus) or postductal (after
the ductus arteriosus).
• Altered Physiology: the narrowing of
the aorta obstructs the blood flow
through the constricted segment of
the aorta, that increasing the left
ventricular pressure. So collateral
vessels develop from the subclavian
arteries bypassing the coarcted aorta
and supplying circulation to the lower
extremities.
• Clinical Manifestation:
• Usually asymptomatic in childhood.
• May demonstrate: occasional fatigue,
headache, nose bleed and leg cramps.
• Absent or greatly reduced femoral pulses.
• Hypertension
in
upper
extremities,
hypotension in lower one.
• E.C.G: show normal to left ventricular
hypertrophy
• Diagnosis: Cardiac Catheterization, Angiography.
• Complication: Cerebral Hemorrhage, Rupture Aorta,
and C.H.F.
• Treatment:
• Management of C.H.F.
• Surgical: Resection of area of coarctation or balloon
angioplasty at 2-7 years.
• V. Patent Ductus Arteriosus
• Is the persistence of a fetal connection between the
pulmonary artery and the aorta through which blood
leaving the right heart bypasses the lungs.
• Altered Physiology:
• Failure of the ductus to close after birth. Patent ductus
arteriosus allow blood to shunt from aorta (high pressure) to
the pulmonary artery low pressure.
• Failure of the ductus arteriosus to close leads to continued
blood flow from the aorta to the pulmonary artery. Blood
returning to the left atrium passes to the left ventricle, enters
the aorta, and then travels to the pulmonary artery via the
PDA instead of entering the systemic circulation. This altered
blood flow pattern increases the workload of the left side of
heart.
• Pulmonary vascular congestion occurs, causing an increase in
pressure.
• Right ventricular pressure increases in an attempt to
overcome this increase in pulmonary pressure. Eventually,
right ventricular hypertrophy occurs.
Clinical Manifestation:
• 1- Small PDA: usually asymptomatic.
• 2- Large PDA: may develops symptoms during early infancy,
slow weight gain, feeding difficulties, frequent respiratory
infection, CHF, physical retardation, systolic murmur and
widened pulse pressure
• Complication: C.H.F., infective endocarditis.
• Treatment:
• Controlling of C.H.F.
• Surgical by ligation or division and ligation of the duct
―electively by 1-2 years‖.
• Closure of ductus arteriosus is stimulated by increase in O2
level and by indomethacin
• VI. Atrial Septal Defect
•
Is an abnormal opening in the septum between two
atrium.
• Altered Physiology:
• The pressure in the left atrium is greatening
than that in the right one, which promotes the
flow of oxygenated blood from the left to the
right atrium and thus increasing the total blood
flow through the lung.
• If the pulmonary resistance is great reversal
the shunt with unoxygenated blood flowing
from the right to left atrium and cyanosis
occur.
•
•
•
•
•
•
Clinical Manifestation:
Heart murmur
Dyspnea and right ventricular hypertrophy
Fatigue and poor growth.
Complication: CHF, and pulmonary hypertension.
Treatment: Surgical closure the defect.
Ventricular Septal Defect
• Is an abnormal opening in the septal between
the two ventricles. It may vary in size from
very small defect to very large defect {1-15
mm in diameter}. 50% of cases close
spontaneously within one to three years. It is
one of the most common congenital heart
defects.
• Altered Physiology:
• The pressure in the left ventricle is greater than that of the
right one promotes the flow of oxygenated blood from the
left to the right ventricle increasing the total blood flow
through the lungs and thus increased right ventricular and
pulmonary arterial pressure.
• If the pulmonary resistance is great, thus causing reversal of
the shunt with unoxygenated blood flowing from the right
ventricle to the left one and thus cyanosis occure
• Clinical Manifestation:
• Systolic heart murmur.
• Slow weight gain, feeding difficulties, frequent respiratory
infections.
• Dyspnea and tachypnea.
• Treatment:
• Medical management of C.H.F.
• Surgical closure: optimal age
before 2years to prevent
pulmonary hypertension.
•
• Cyanotic Congenital Heart Disease
• I. Teratology of Fallot (TOF)
• The most common type of cyanotic heart disease, its
involve four anatomical abnormalities:
• 1- Pulmonary stenosis.
• 2- Ventricular septal defect {VSD}.
• 3- Overriding of the aorta (enlargement of the aortic valve)
• 4- Right ventricular hypertrophy.
• Altered Physiology:
• Pulmonary stenosis: unoxygenated blood is shunted from
the right ventricle (from the VSD) directly into the aorta.
• The right ventricle is hypertrophied because of high right
ventricular pressure.
• Clinical Manifestation:
• Cyanosis: not cyanotic at birth {left to right
shunt}, may starts later, may be at 1-2 years,
first observed with exertion or crying, then
cyanotic even at rest.
• Clubbing of fingers.
• Squatting posture is assumed to relief stressed
heart by trapping blood in lower extremities.
• Slow weight gain.
• Hypoxia spells (Tet spells characterized by
sudden cyanosis and syncope)
• Complication: CHF, endocarditis,
CVA and iron deficiency anemia.
• Treatment:
• Improve oxygenation
• Emergency for Tet spells: betablockers as propranolol, but acute
episodes may require rapid
intervention with morphine are
required.
• Surgical
• Complete intracardiac repair of VSD and PA stenosis.
• Enter chest through the sternum.
• Connect the heart and lung machine. Heart is
stopped.
• Repair the VSD with a patch.
• removing the excessive muscle tissue will help to
function correctly.
• Pacemaker wires are placed temporarily because of
the potential for postoperative ventricular
arrhythmias.
• Individual chamber pressures are then measured
before the chest is closed. The pressure readings
help to determine how effective the surgery was.
• II. Transposition of the Great Arteries (TGA)
• TGA occurs when the aorta arises from the right
ventricle and the pulmonary artery from the left
ventricle.
• Incompatible with life unless the infant has an
associated defect which allows the blood to
communicate between the pulmonary and systemic
circulation.
• Clinical Manifestation:
• Marked cyanosis since birth.
• Failure to thrive, Fatigability and dyspnea with
subcostal retractions at rest
• Cardiomegaly, early clubbing of fingers and C.H.F.
• Prognosis: without surgical treatment, 85 % die
in the first 6 months of age.
• Treatment:
• Management of C.H.F.
• Palliative procedures: creation of A.S.D. with a
balloon catheter during catheterization or
surgical creation of A.S.D.
• Complete correction: by cardiopulmonary
bypass.
• III. Tricuspid Atresia
• Is a condition in which there is a complete
absence of the tricuspid valve. Therefore, there
is an hypoplastic of right ventricle. Its associated
with:
• Atrial septal defect.
• There is usually a V.S.D. allowing some blood to
enter the underdeveloped right ventricle.
•
• Pathophysiology:
• Blood from the systemic circulation is shunted
from the right atrium through an interatrial
communication to the left atrium, to the left
ventricle.
• Pulmonary blood flow is established either
through PDA or VSD.
• Clinical Manifestation:
• Cyanosis {marked since birth}, dyspnea on
feeding and may hypoxia spells.
• Early clubbing of fingers and failure to thrive.
• Right heart failure may occur.
• Treatment:
• Palliative procedures: to increase the pulmonary
blood flow (Anastomosis between the ascending
aorta and right pulmonary artery).
• Fontan Procedure: is a palliative surgical
procedure used in children with complex
congenital heart defects. It involves diverting the
venous blood from the right atrium to the
pulmonary arteries without passing through the
morphologic pulmonary ventricle
• Complete correction
• Diagnostic Evaluation for Congenital Heart
Defects.
• 1. Chest x- ray shows enlargement of the
affected chambers of the heart.
• 2. Cardiac catheterization: visually demonstrate
the defect, demonstrate blood oxygenation in
heart chambers.
• 3. E.C.G.
• Nursing care plan for the child with congenital heart
disease
• Assessment:
• Take careful health history including evidence of:
poor weight gain, unusual posturing or poor feeding
• Exercise intolerance – frequent respiratory tract
infections
• Perform physical assessment with special emphases
on: color, pulse (apical and peripheral), respiration,
blood pressure, examination and auscultation of
chest and manifestations of CHD.
Thank You All
Any Question ??????