* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Biol 155 Human Physiology - University of British Columbia
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Electrocardiography wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Heart arrhythmia wikipedia , lookup
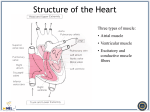
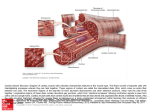
Dextro-Transposition of the great arteries wikipedia , lookup
Smooth Muscle Characteristics Not striated Dense bodies instead of Z disks as in skeletal muscle Have noncontractile intermediate filaments Ca2+ required to initiate contractions Types Visceral or unitary Function as a unit Multiunit Cells or groups of cells act as independent units Smooth Muscle Contraction Electrical Properties of Smooth Muscle Functional Properties of Smooth Muscle Some visceral muscle exhibits autorhythmic contractions Tends to contract in response to sudden stretch but no to slow increase in length Exhibits relatively constant tension: Smooth muscle tone Amplitude of contraction remains constant although muscle length varies Smooth Muscle Regulation Innervated by autonomic nervous system Neurotransmitter are acetylcholine and norepinephrine Hormones important as epinephrine and oxytocin Receptors present on plasma membrane which neurotransmitters or hormones bind determines response Cardiac Muscle Found only in heart Striated Each cell usually has one nucleus Has intercalated disks and gap junctions Autorhythmic cells Action potentials of longer duration and longer refractory period Ca2+ regulates contraction Cardiac Muscle Elongated, branching cells containing 1-2 centrally located nuclei Contains actin and myosin myofilaments Intercalated disks: Specialized cell-cell contacts Desmosomes hold cells together and gap junctions allow action potentials Electrically, cardiac muscle behaves as single unit Cardiac myocyte action potential: Refractory Period Absolute: Cardiac muscle cell completely insensitive to further stimulation Relative: Cell exhibits reduced sensitivity to additional stimulation Long refractory period prevents tetanic contractions AP-contraction relationship: AP in skeletal muscle is very short-lived AP is basically over before an increase in muscle tension can be measured. AP in cardiac muscle is very long-lived AP has an extra component, which extends the duration. The contraction is almost over before the action potential has finished. Functions of the Heart Generating blood pressure Routing blood Ensuring one-way blood flow Heart separates pulmonary and systemic circulations Heart valves ensure one-way flow Regulating blood supply Changes in contraction rate and force match blood delivery to changing metabolic needs Orientation of cardiac muscle fibres: Unlike skeletal muscles, cardiac muscles have to contract in more than one direction. Cardiac muscle cells are striated, meaning they will only contract along their long axis. In order to get contraction in two axis, the fibres wrap around. Circulation circuits: Heart Wall Three layers of tissue Epicardium: This serous membrane of smooth outer surface of heart Myocardium: Middle layer composed of cardiac muscle cell and responsibility for heart contracting Endocardium: Smooth inner surface of heart chambers Valve function: Coronary circulation: Pacemaker potential: Cardiac conducting system: EKG: Heart Sounds First heart sound or “lubb” Second heart sound or “dupp” Atrioventricular valves and surrounding fluid vibrations as valves close at beginning of ventricular systole Results from closure of aortic and pulmonary semilunar valves at beginning of ventricular diastole, lasts longer Third heart sound (occasional) Caused by turbulent blood flow into ventricles and detected near end of first one-third of diastole Heart sounds: Cardiac Arrhythmias Tachycardia: Heart rate in excess of 100bpm Bradycardia: Heart rate less than 60 bpm Sinus arrhythmia: Heart rate varies 5% during respiratory cycle and up to 30% during deep respiration Premature atrial contractions: Occasional shortened intervals between one contraction and succeeding, frequently occurs in healthy people Mean Arterial Pressure (MAP) Average blood pressure in aorta MAP=CO x PR CO is amount of blood pumped by heart per minute CO=SV x HR SV: Stroke volume of blood pumped during each heart beat HR: Heart rate or number of times heart beats per minute Cardiac reserve: Difference between CO at rest and maximum CO PR is total resistance against which blood must be pumped Pressure relationships: Cardiac Cycle Heart is two pumps that work together, right and left half Repetitive contraction (systole) and relaxation (diastole) of heart chambers Blood moves through circulatory system from areas of higher to lower pressure. Contraction of heart produces the pressure Factors Affecting MAP Regulation of the Heart Intrinsic regulation: Results from normal functional characteristics, not on neural or hormonal regulation Starling’s law of the heart Extrinsic regulation: Involves neural and hormonal control Parasympathetic stimulation Supplied by vagus nerve, decreases heart rate, acetylcholine secreted Sympathetic stimulation Supplied by cardiac nerves, increases heart rate and force of contraction, epinephrine and norepinephrine released Heart Homeostasis Effect of blood pressure Effect of pH, carbon dioxide, oxygen Chemoreceptors monitor Effect of extracellular ion concentration Baroreceptors monitor blood pressure Increase or decrease in extracellular K+ decreases heart rate Effect of body temperature Heart rate increases when body temperature increases, heart rate decreases when body temperature decreases Baroreceptor and Chemoreceptor Reflexes