* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Slide 1
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
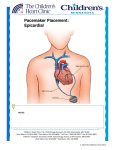
The Dizzy Ranger Simulation Case Debriefing Material Debriefing questions – What went right? – What went wrong? – How do you treat bradycardia secondary to high degree AV block? – What are the indications and contraindications for emergent pacing? – What is the proper placement of the single lumen introducer catheter for transvenous pacing? – What heart chamber are you trying to place the pacemaker? – How can you confirm proper placement and capture of the pacemaker? – Describe the cardiac manifestations of Lyme carditis. – How is Lyme carditis treated? ACLS bradycardia interventions (HR <60 with symptoms) • • • • Assess airway and breathing. Establish IV, give O2 (continuous pulse oximetry) Place on cardiac monitor (and obtain ECG) and check blood pressure With signs/symptoms of poor perfusion: – Prep for trancutaneous pacing (emergent use if high degree AV block present) – Consider atropine 0.5 mg IV and repeat to a max total dose of 3mg if pacer is not ready – Consider epi (2-10 micrograms/min) or dopamine (2-10 micrograms/min) infusions if pacer not ready or is ineffective – Prepare the transvenous pacer and consider consulting cardiology Recognizing high degree AV block • 2nd degree AV block – Mobitz I (Wenckebach): Progressive prolongation of the PR interval and shortening of the R-R until the QRS is dropped. • Not generally associated with a higher mortality EXCEPT in the context of acute MI – Mobitz II: Atrial beat sporadically not conducted with constant PR and R-R intervals. • Can progress to 3rd degree heart block and thus carries a higher mortality – Both can be seen with Lyme disease • 3rd degree AV block – See complete AV dissociation with the QRS being conducted at an independent rate from the atrial rate – Patient’s are generally hemodynamically unstable with bradycardia and hypotension Indications for pacing in the setting of bradycardia • Symptomatic sinus node dysfunction • Sinus arrest, tachy/brady syndrome, sinus bradycardia • Second or third degree heart block • Includes Mobitz I in the setting of myocardial infarct • Symptomatic slow atrial fibrillation • New LBBB, RBBB with left axis deviation, bifascicular block, or alternating BBB in the setting of acute MI • Prior to procedures that may induce bradycardia • Malfunction of implanted pacemaker Contraindications to pacing in the setting of bradycardia • No absolute contraindications • Hypothermia – Bradycardia may be manageable without pacing while awaiting rewarming – Pacing may precipitate V Fib that is difficult to convert. • Thrombolytic use: – Transcutaneous pacing may be preferred • Asymptomatic patients – Good idea to consider placing pacing pads in case of deterioration Highlights for transcutaneous pacing • Consider pretreating with opiods and benzodiazepines prior to initiation • Place anterior pad at point of maximal impulses to the left chest wall • Place the posterior pad directly posterior to the anterior pad • Attach the patient to the ECG monitor and make sure both ECG leads and pacer pads are hooked up to the pacemaker • Set the presets to rate 80 and around 40-60 mA – May also start with lower amperage and increase dose until capture occurs • Confirm placement by assessing rhythm strip for consistent pacer spike followed by QRS and improvement in patient’s symptoms Highlights for emergent transvenous pacing • If you have the time: – Arrange for either ultrasound to confirm placement OR – Attach the negative electrode the the V1 lead on an ECG machine • Please refer to the Pacing instructions for tips on transvenous placement – Figure 4 Proper location for single lumen catheter for transvenous pacing • Preferred locations are the right internal jugular vein or the left subclavian vein • These provide the straightest path to the the right heart anatomically • Check your institutions preference and cardiology preference for permanent pacemaker placement – Avoid the most likely site of permanent pacemaker placement if possible Transvenous pacer: Confirmation of placement • Right ventricular placement is confirmed on ECG with LBBB pattern and LAD – Note that RBBB may indicate coronary sinus placement or septal perforation and LV pacing • Look for cannon waves present on exam of the neck veins • Listen for tricuspid insufficiency murmur due to obstruction from the catheter • Clinically assess for improvement in vitals, mentation, cardiac congestion • Obtain portable CXR radiological confirmation • May also use ultrasound to confirm that placement of the catheter in the right ventricle Treatment of Lyme Carditis caused by high degree AV block • Symptomatic support including pacing if necessary – Complete heart block generally resolves within one week • Hospitalize and give IV ceftriaxone (2g IV daily for 2-4 weeks) or high-dose Penicillin G. • A combination of IV and po antibiotics should be continued for 4 weeks. – Including amoxicillin, doxycycline, and/or ceftriaxone References • Field, JM; Hazinski, MF; Gilmore, D. American Heart Association’s Handbook of Emergency Cardiovascular Care for Healthcare Providers. 2005. • Roberts J.R., Hedges J.R.: Clinical Procedures in Emergency Medicine, 4th ed. Philadelphia, PA, WB Saunders, 2003, CH 15. • Bing OH, McDowell JW, Hantman J, et al: Pacemaker placement by electrocardiographic monitoring. N Eng J Med 287:651, 1972 • Goldberger E: Treatment of Cardiac Emergencies, 3rd ed. St. Louis, CV Mosby, 1982, p252. • Fish AE; Pride YB; Pinto DS: Lyme carditis. Infect Dis Clin North Am; 22(2): 275-88, vi; 2008