* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Constrictive Pericarditis - Mike Poullis
Remote ischemic conditioning wikipedia , lookup
Heart failure wikipedia , lookup
Echocardiography wikipedia , lookup
Pericardial heart valves wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Coronary artery disease wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Myocardial infarction wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Constrictive
Pericarditis
Mike Poullis
The pericardium
• Two-layered sac that encircles the heart
• Inner serosal layer ( visceral pericardium )
adhering to the outer wall of the heart
• Reflected at the level of the great vessels
• Joins the tough fibrous outer layer ( parietal
pericardium ).
• A thin film of fluid ( about 50 ml ) slightly
separates the two layers and decreases friction
between them.
Function of pericardium
• Fixes the heart within the mediastinum and
limits its motion;
• Prevents extreme dilatation of the heart
during sudden rises of intracardiac volume
• Function as a barrier to limit spread of
infection from the adjacent lungs.
• But patients with complete absence of the
pericardium (congenital or surgically)
generally do fine without it, casting doubt
on its actual physiologic importance.
Pathology of Constrictive Pericarditis
• Present when a fibrotic, thickened, and adherent
pericardium restricts diastolic filling of the heart.
• An initial episode of acute pericarditis, which may
not be detected clinically.
• Organisation & resorption of effusion
• Fibrous scarring and thickening of the pericardium
• Obliteration of the pericardial space
• Uniform restriction of filling of all heart chambers.
• Calcium deposition may contribute to stiffening of
the pericardium.
Importance of Constrictive
pericarditis
• Although uncommon, commands substantial
clinical interest because of the perceived
potential for surgical cure.
• In the past 15 years, the spectrum of CP,
characterized chiefly by a declining
incidence of tuberculous pericarditis and an
increase in the frequency of cases resulting
from therapeutic mediastinal radiation and
cardiac surgery
Clinical Features - Symptoms and signs
• Reduced cardiac output (fatigue, hypotension,
reflex tachycardia)
• Elevated systemic venous pressure (jugular
venous distension, hepatomegaly with marked
ascites and peripheral edema)
• Pulmonary venous congestion (exertional
dyspnea, cough and orthopnea)
• Chest pain typical of angina may be related to
underperfusion of the coronary arteries or
compression of an epicardial coronary artery by
the thickened pericardium.
JVP sign’s.
• Friedrich’s sign - rapid Y decent in JVP
• Kussmauls’s sign - increasing JVP with
inspiration
A
C
V
Z
X
Y
Clinical catch
• Because the most impressive physical
findings are often the insidious development
of ascites of hepatomegaly and ascites, such
patients are often mistakenly thought to
suffer from hepatic cirrhosis or an intra abdominal tumor. It is only after a careful
inspection of the jugular veins that a cardiac
source is identified.
Etiology of Constrictive Pericarditis
Idiopathic - nearly half of cases
. Post Viral Pericarditis
. Tuberculosis - 15 % of cases in developed nations
. Postsurgical
. Prior Mediastinal Radiation Therapy
. Chronic Renal Failure Treated with Hemodialysis
. Connective Tissue Disorders
. Neoplastic Pericardial Infiltration
. Incomplete Drainage of Purulent pericarditis
. Fungal and Parasitic Infections
. Following Pericarditis Associated with Acute Myocardial Infarction
. Following Postmyocardial Infarction ( Dressler ) Syndrome
. In Association with Pulmonary Asbestosis
Changing aetiologies
Differential
• Clinically, it is important to distinguish
constrictive pericarditis from restrictive
cardiomyopathy- each of which have
similar clinical presentations and
hemodynamic alterations
Pathophysiology
• Constriction of pericardium results in elevation
and equilibrium of all 4 cardiac chambers
• In early diastole, when intracardiac volume is
less than stiff pericardium, diastolic filling is
unimpeded and early diastolic filling abnormally
rapidly because venous pressure is elevated.
• Rapid early diastolic filling is abruptly halted
when the intracardiac volume reaches the limit
set by the noncompliant pericardium.
Atrial Naturetic Peptide
•
•
•
•
Elevated in CCF
Normal in constrictive pericarditis
Elevated after pericardectomy
Normalises
• atrial stretch hypothesis
Pathology specimen
ECG
• Atrial arrhythmias may be present.
• The amplitude of the QRS complexes and T
waves may be diminished.
• The QRS complex may be abnormal in addition
to exhibiting low voltage.
• The mean QRS vector is usually directed
normally but may shift to the right.
• Abnormal initial QRS forces and bundle branch
block may occasionally occur due to
calcification of the deeper portion of the
myocardium.
ECG
CXR
• Normal or mildly enlarged cardiac silhouette
• Calcification of the pericardium is detected in up
to 50% - not specific
• A calcified pericardium is not necessarily a
constricted one.
• Lateral CXR shows the atrioventricular groove &
the anterior and diaphragmatic surfaces of the
right ventricle.
• Pleural effusions are present in about 60 %
• Persistent unexplained pleural effusions can be
the presenting manifestation.
CXR
CXR
CT
• Pericardial calcification is best appreciated
on CT
MRI
• Normal pericardium appears curvilinear as a low
signal intensity situated between the high signal
intensity of the pericardial and epicardial fat
• Normally 1 to 2 mm in thickness - a width of up
to 4 mm is not necessarily pathologic.
• Small quantities of pericardial fluid may be seen
normally in the superior pericardial recess
(posterior to the ascending aorta).
• A pericardial thickness of greater than 4 mm is
considered evidence of constrictive pericarditis in
the appropriate clinical setting.
CT
Caution of radiology
• History of cardiac surgery or postpericardiotomy syndrome
– Both have significant pericardial thickening in
the absence of clinical symptoms.
• Absence of pericardial thickening does not
exclude constrictive pericarditis
Echocardiography
• Echocardiographic evidence is subtle
• Pericardium, if well imaged, is thickened
• Ventricular cavities are small and contract
vigorously
• Diastolic filling terminates abruptly in early
diastole (doppler flow analysis)
• Doppler echocardiography often shows the
dissociation of intrathoracic and intracardiac
pressures through respiratory changes in mitral
flow velocities.
• E - A Reversal
Doppler
• mitral valve (MV)
inflow (A) and
hepatic vein (HV)
Doppler velocity
recording (B) in
constrictive
pericarditis.
• high E and small A
velocities. EXP E
velocity is 33%
higher than INSP
Cardiac catheterization
• Elevation and equalization of the diastolic
pressures in all cardiac chambers
• Right and left ventricular tracings show an early
diastolic "dip-and-plateau "
• Right atrial pressure tracing shows a prominent Y
descent
• Findings similar to restrictive cardiomyopathies,
(suggested by a right ventricular systolic BP > 60
mm Hg) and LVDP exceeding RVDP by more
than 5 mm Hg
• Endomyocardial biopsy can distinguish these
Catheter pressures
Catheter pressures
• Elevated RV diastolic pressure, dip-and-plateau
waveform ("square root sign"), large P waves
(arrow)
• Postoperative decreased RV diastolic pressure
normalization of dip-and-plateau & P-wave
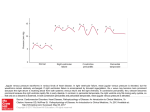
Constrictive pericarditis vs restrictive
cardiomyopathy
• group 1
constrictive
pericarditis
• group 2 other
causes of heart
failure.
• Open circles are
group 2 with
restrictive
cardiomyopathy
Management
• Chronic constrictive pericarditis is a progressive
irreversible disease
• Minority survive for years with modest elevated
JVP and peripheral edema that is controlled by
diet and diuretics.
• Drugs that slow HR, eg beta blockers and Ca2+
channel blockers should be avoided as mild sinus
tachycardia is a compensatory mechanism.
• The majority of patients become progressively
more disabled and subsequently suffer the
complications of severe cardiac cachexia.
Management (cont)
• Treatment for constrictive pericarditis is
complete resection of the pericardium.
• Attention must also be paid to the presence of
associated right atrial thrombosis, which can
partly obstruct the tricuspid valve and should be
managed with thrombectomy at the time of
pericardiectomy.
• Concomitant CABG +/- other
• Changes in technique have included the use of
median sternotomy rather than left thoracotomy
• CPB controversial
Operative
picture
Operative Mortality
• The operative mortality is between 5 and 20 %
• Low output syndrome occurring in up to 30 %
of patients in the immediate postoperative
period
• Symptomatic improvement can be expected in
about 90 %
• Complete relief of symptoms in 50 %.
• Five year survival ranges from 75-85 %
Exclude
• Pericardiectomy probably should not be
routinely attempted in
• Elderly patients with severe liver
dysfunction
• Cachexia
• Densely calcified pericardium
• Massive cardiac enlargement indicating
myocardial damage
• Patients with limited life expectancy.
Delayed cure
• May be delayed for weeks to months after
surgery
• Incomplete pericardial resection (sometimes
the visceral pericardium must also be resected)
• Myocardial atrophy or fibrosis caused by the
inflammatory process
• Development of recurrent cardiac compression
by mediastinal inflammation and fibrosis.
Not just the heart
• Involvement of adjacent pleuropulmonary
structures by the constrictive disease
process and concomitant chronic
obstructive lung disease with limited
functional recovery occurs in nearly a fifth
of patients
• These mechanisms are not mutually
exclusive in individual cases.
Outcome
Outcome
Overall survival
Age
NYHA class
Previous radiation
Serum sodium
Late survival
Age
NYHA class
Previous radiation
Late CV death
Age
NYHA class
Previous radiation
Late NYHA class III–IV
CHF
Age
Previous radiation
Ascites
Adjusted Hazard
Ratio
95% CI
P
1.07
2.43
5.13
1.11
1.04–1.10
1.22–4.86
2.49–10.56
1.04–1.18
<0.0001
0.012
<0.0001
0.001
1.08
3.99
11.80
1.04–1.12 <0.0001
1.76–9.08 0.0009
4.57–30.44 <0.0001
1.07
3.38
20.74
1.03–1.12 0.0009
1.25–9.19 0.017
6.77–63.52 <0.0001
1.04
9.47
2.19
1.01–1.07 0.010
4.19–21.39 <0.0001
1.03–4.67 0.042