* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Cardiovascular System & Disease
Saturated fat and cardiovascular disease wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Jatene procedure wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
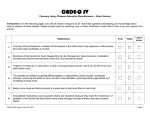
Course Contents
Section 1
Exercise and the cardiovascular system
1.1
Structure and function of the cardiovascular system
1.2
Pathology of cardiovascular diseases (CVD)
1.3
Role of exercise in prevention and treatment of CVD
Section 2
Exercise and Metabolism
2.1
Energy
2.2
Body composition & Weight Control
2.3
Diabetes Mellitus
2.4
Osteoporosis
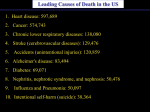
BHF Survey, 2007
Scottish Stats
Deaths from CHD
The CVS is subject to disease processes e.g.
Atherosclerosis & hypertension are disease processes that
lead to the development of :
Structure/ Function of CVS
2 parts:
Pump
Vessels
Heart
Heart external
view
Double pump
Right side – pumps to lungs (pulmonary
circulation)
BICUSPID
Left side – pumps to body (systemic
(mitral)
circulation
VALVE
Left
side > right side
TRICUSPID
VALVE
Heart
Valves prevent backflow of blood
Coronary arteries supply heart muscle with
blood (food & oxygen)
SEMILUNAR VALVE
Heart & Blood Supply
Pulmonary artery – deoxygenated blood
Pulmonary
N.B.
Hepatic Portal vein
Vein – oxygenated
Coronary
arteries
– heart.
supply heart
does not return
blood to
Coronary veins – drain into the right atrium
Supplies
liver with products of digestion.
Aorta
- blood
body
(from L. ventricle)
Important
in firstto
pass
metabolism
Vena cava
(sup./toxins
inf.)to -bedrain
(into
– allowing
broken body
down before
systemic circulation
R atrium)
Heart Beat
Heart beat is endogenous (continues to beat if
removed from body)
Rhythmical contraction of muscles
Under nervous/ hormonal control
Influence strength & frequency of contraction
Heart beat originates in SinoAtrial node
Max. rate limited (refractory period)
AV node collects signal and initiates ventricular
contraction via Bindle of His after a short delay.
In disease, arrythmia can develop in damaged tissue
Extra heart beat can occur initiated by damaged tissue
Heart beat signal propagated through heart by bundle
of His (atria – ventricles), & Purkinje fibres (nerves
through muscle tissue)
Heart Sounds
Stethoscope
Listen to heart sounds
Lub dub (closing of valves)
Lub – closure of AV valves
Dub – closure of semilunar valves
Diagnostic of valvular disease
Leaky – indistinct lub/ dub
Heart & ECG
ECG is a record of the electrical signals
producing the heart beat
ECG= ElectroCardioGram
Used diagnostically to show heart
problems
Cardiac Cycle
DIASTOLE (relaxed phase)
Venous filling of atria
Atria distend
Some passive flow into ventricles
SYSTOLE (contractile phase)
SA initiates atrial contraction
Blood expelled from atria into ventricles
Bundle of His conducts excitation to
ventricles/ propagated rapidly by Purkinje
fibres
Ventricle contracts expels blood into arteries
Contraction ends, relaxes (refractory period)
Blood Vessels
Arteries
Must withstand high pressure
Thick walled
Mainly elastic fibres near heart
Arteries more distant from heart less elastic fibres/
more muscle (under nervous control)
Stretch to absorb pressure of blood expelled by heart
At diastole stretched arteries relax so maintain blood
flow (120/80 mmHg)
Muscles regulate blood flow into capillary beds
Arteries lead to arterioles
Can have pre-capillary sphincters to completely close
blood flow e.g to skin in cold
Blood Vessels
Capillaries
Wall single cell thick
Allows exchange of soluble substances
No cell more than few cell widths from a
capillary
Diffusion rapid over these short distances
Blood vessels
Veins
Less muscle/ elastic fibre than arteries
Floppy
Low pressure in vein – requires valves to
stop backflow
Muscle pumping in calves helps venous
return (Economy Class Syndrome)
Blood Pressure
High arterial blood pressure (80-120
mmHg (systolic/ diastolic)
Rapid fall in BP in arterioles/ capillaries
Very low BP in veins
Blood Pressure
BP quoted as Systolic / diastolic
Measure with a sphygmomanometer
Block all blood flow
Slowly release pressure
Systoliic BP = pressure when sound of
artery closing (snap) is heard
Diastolic BP = pressure when all noises
stop
Summary of Structure
Cardiovascular Disease
Coronary Heart disease
Angina pectoris
Myocardial infarction
CVD s
Cerebrovascular disease
Stroke (cerebrovascular
accident (CVA))
Cardiovascular disease
pathology
Two major pathological processes lead to
CVD
Atherosclerosis
Narrowing & hardening of arteries (claudication/ angina)
Damage to endothelium
– promotes blood clot formation
blocking arteries – thrombosis/ embolism
Hypertension
Prolonged, elevated blood pressure
– Primary – no known cause
– Secondary – caused by pathology
Kidney disease
Phaeochromacytoma (excess epinephrine produced)
Atherosclerosis
Typically starts in childhood, progresses in
adulthood.
Damage to the arterial wall caused by e.g.
elevated levels of cholesterol and triglyceride in
the blood
high blood pressure.
tobacco smoke
diabetes
Atherosclerosis
Fat accumulates under inner lining of arteries
As disease progresses, fibrous material / calcium/
lipids (inc. cholesterol) accumulates (atheroma)
Bulges into lumen of vessel
Starts to reduce diameter of artery
Restricts blood flow
Reduces elasticity of arterial wall
Can lead to high blood pressure
Atherosclerosis
Progression accelerated by:
High blood cholesterol (especially LDL or "bad"
cholesterol over 100 mg/dL)
Cigarette smoking and exposure to tobacco
smoke
High blood pressure
Diabetes mellitus
Obesity
Physical inactivity
Cholesterol & CVD
Cholesterol – steroid
– Cell membranes, hormones, bile salts
Most cholesterol in blood is synthesised by liver
Dietary cholesterol acts to suppress liver biosynthesis
Dietary cholesterol NOT important risk factor for
CVD (overall cholesterol should be less than
200mg/dl)
Saturated fats (animal) are used by liver to
produce cholesterol
High dietary saturated fat INCREASES blood
cholesterol levels!!
Cholesterol & CVD
Cholesterol – insoluble in blood
Transported attached to a protein LIPOPROTEIN
Two types of LIPOPROTEIN
HDL – High density lipoprotein
LDL – Low density lipoprotein
HDL – transports cholesterol to liver for destruction
LDL – transports cholesterol to body cells for
deposition
GOOD
BAD
In abnormal circumstances LDL will deposit cholesterol in
arteries
Cholesterol & CVD
LDL (bad) – 60-70% blood cholesterol
As LDL increases risk of atherosclerosis
increases
HDL (good) – 20-30% blood cholesterol
AS HDL increases risk of atherosclerosis
decreases
Risk of CHD is predicted from HDL:LDL ratio
High HDL (40mg/dl or more):LDL is GOOD
Exercise, low fat diet, not smoking improve
HDL:LDL ratio
Atherosclerosis – Heart - AP
Narrowing of coronary arteries leads to
ischaemia (inadequate blood flow)
Pain - angina pectoris (AP) due to ischaemia in
heart muscle
AP only during exertion of heart (when O2 needs
are high)
Glycerol trinitrite tablets release Nitric oxide (dilates
blood vessels)
Angioplasty/ Stents
Bypass surgery
Atherosclerosis – Embolism
Clots
thrombus-attached
embolus-travelling
Embolus/ thrombus can cause blood supply to a
region of the heart muscle (myocardium) to
become blocked, causing myocardial infarction
Thrombosis/ embolus may occur in cerebral artery
– stroke (cerebrovascular accident-CVA)
or lungs pulmonary embolus
Myocardial Infarction
Myocardial infarction – MI (death of heart tissue)
Caused by a sudden blockage to a coronary artery.
Due thrombosis/ embolis
Atherosclerosis (may cause angina symptoms) leads to increased
likelihood that thombosis will occur.
Causes pain (15 min) in arm, neck, jaw; nausea.
If large artery blocked – collapse, sudden death
Tissue dies forming a scar, can cause:
Heart failure (weak pumping action)
Arrythmia, irregular contraction
Cardiac arrest – ventricular fibrillation
Hypertension
Persistently high resting blood pressure
e.g. diastolic >90mmHg (normal
120/80; high 140/90)
Often caused by atherosclerosis leading
to narrowing of arteries or loss of
elasticity
Risk factor for majority of CVDs (incl. CHD)
Hypertension – risk factors
Diet (high salt
(Na+), high fat)
Nicotine (vasoconstrictor)
Smoking
Obesity
Genetic
predisposition
Stress
Risk Factors for CVD- SQA
Modifiable
Diet, Smoking, Activity, Obesity
Non modifiable
Age, Gender, Race, Heredity
Risk factors Summary
What other factors contribute to heart disease risk?
•Diabetes•The
mellitus
—heart disease in people who drink
risk of
•Obesity
andseriously
overweight
— of alcohol
•Diabetes
increases
your risk
developing
moderate
amounts
(anofaverage
of one drink
cardiovascular
disease.
for who
women
or excess
two drinks
forfat
men
per day) isiflower
than
•People
have
body
— especially
a lot of
it is at
•risks in
arenondrinkers.
even greater
if blood
sugar
is notas
well
controlled.
One
drink
is defined
1-1/2
fluid
the
waist
—
are
more
likely
to
develop
heart
disease
and stroke
Physical
inactivity
•Aboutounces
three-quarters
of
people spirits
with diabetes
of some form of
(fl oz)
ofother
80-proof
(such asdie
bourbon,
even
if
they
have
no
risk
factors.
Regular,
moderate-to-vigorous
physical
activity helps
prevent
heart
heart
or
blood
vessel gin,
disease.
Scotch,
vodka,
etc.),
1
fl
oz
of
100-proof
spirits,
4
fl
High
blood
pressure
High
cholesterol
and blood
blood
vessel
disease.
•Excess
weight
increases
the
heart's
work.
Itworkload,
also raises
blood
oz
of
wine
or
12
fl
oz
of
beer.
It's
not
recommended
High
blood
pressure
increases
the
heart's
causing
As
blood
cholesterol
rises,
so does
risk
of coronary
heart
The
more
vigorous
the
activity,
thetriglyceride
greater
your
benefits.
pressure
and
blood
cholesterol
and
levels,
and
that
nondrinkers
start
using
alcohol
or
that
drinkers
the
heart
to
thicken
and
become
stiffer.
disease. Physical activity can help control blood cholesterol, diabetes and
lowers
HDL
("good")
cholesterol
levels.
increase
the
amount
they
drink.
Tobacco
It
also
smoke
increases
your
risk
of
stroke,
heart attack,
kidney failure
When
other
highpressure
blood pressure
and
tobacco
obesity,
as risk
wellfactors
as help(such
loweras
blood
in some
people.
and
• congestive
Smokers'
heart
risk
failure.
ofrisk
developing
coronary
disease
is obese
2–4 times that
•It
can
also
make
diabetes
more
likelymore.
toheart
develop.
Many
smoke)
are
present,
this
increases
even
of nonsmokers.
highcholesterol
blood
pressure
exists
with
obesity,
smoking,
highby
and
overweight
people
may have
difficulty
losing
weight.
AWhen
person's
level
is also
affected
by age,
sex, But
blood
•
cholesterol
riskdiet.
factor
forfew
sudden
oras
diabetes,
thedeath:
risk
about
heart
twice
attack
the
orheart
risk
stroke
of
losing
evenlevels
as
10cardiac
pounds,
youof
can
lower
your
heredity
and
increases
nonsmokers.
several
times.
disease
risk.
•
Exposure to other people's smoke increases the risk of heart
disease even for nonsmokers.
Exercise & CVS
Cardiovascular system (CVS) delivers oxygen
& nutrients to body tissues, removes wastes
During exercises more O2 & nutrients required by
exercising tissues (muscles), wastes removed
Exercise effects Cardiovascular system
function
Cardiac output increased
Circulation redistributed to important tissues
Cardiac Output
Cardiac output (C.O.) = volume of
blood pumped per min. by the heart
Regulated by:
– Heart rate (H.R.)
– Stroke volume (S.V.)
C.O. = H.R. x S.V.
Exercise effects on Heart
Exercise causes HR & SV to increase i.e.
CO
Meets needs of muscles
Athlete’s Heart
Regular exercises strengthens heart muscle
Ventricular mass (echocardiography) increases (210-300g)
Force of contraction , more blood expelled per beat (SV )
Ventricular volume also increases (100-180ml) (SV )
Consequently HR at rest of a trained athlete
(Bjorn Borg – 32bpm, Miguel Induraine, 29bpm)
CO of trained heart increased so more O2 and food
delivered at max. HR
Therefore max. level of activity greater
Redistribution of Blood flow
During exercise blood flow directed
away from non-essential needs (gut,
kidney)
Redirected to heart, muscles, skin
(cooling)
Vasodilation/ vasoconstriction of
supplies to these tissues.
Exercise & Blood Pressure
Cardiac Output increased (HR/ SV)
Tends to increase BP
Vasodilation of blood supply to muscles
Increases volume of vascular system
Peripheral vascular resistance reduced
Tends to reduce BP
Overall slight increase in BP
Systolic increase > diastolic
Exercise & Hypertension
Regular exercise, produces long term,
moderate fall in BP
Offsets age related hardening of arteries
Acutely, a fall in BP is also found following
exercise.
Role of exercise
- in preventing CVD
Decreases a number of risk factors:
HDL , LDL
Resting HR
Arterial blood pressure
Body fat (i.e. obesity )
Reduces development of atheroma
Reduces stress
Moderate exercise 3-5 times per week lasting
more than 20mins
Exercise testing - Introduction
Monitor recovery from MI
Monitor improvement in athletic training
programme
Measure aerobic capacity
Assess performance of respiratory and
cardiovascular systems in delivering oxygen
Exercise testing - Principles
Oxygen required by body to work
Maximum work rate – determined by body’s
ability to deliver oxygen to body
VO2max – maximal oxygen uptake
Higher the VO2max, the greater the aerobic fitness
Measure by exercising to exhaustion and
directly measure O2 uptake and CO2 ouput
Exercise testing – Direct Method
Treadmill/ bicycle ergometer
Using online gas analysis
Progressively increase workload until no
further increase in O2 consumption
i.e. exercise to exhaustion
Oxygen consumption at that point =
VO2max
Suitable for fit people
Exercise testing – Indirect
Method
Shuttle test
Run between two cones (20m apart)
Rate determined by a tape (beep)
Subject continues until they can’t maintain
pace
Number of completed shuttles can be
used to predict VO2max
Exercise Testing – Sub maximal
If exercise to exhaustion clinically contraindicated
Submaximal testing used
Patient O2 consumption measured at various
levels of work intensity (submaximal)
Graph of O2 consumption vs. HR plotted
Theoretical max. HR calculated (220-age)
Graph extrapolated to estimate theoretical
max. O2 consumption
Exercise Testing – Sub maximal
Assumptions:
Direct relation between HR and O2 consumption
and intensity of exercise
Sources of error:
HR affected by other factors:
– Emotion
– Temperature
– Anxiety
Predicted HR may be inaccurate for a given
individual
Exercise Stress Testing
Used to diagnose heart abnormality
only present under stressed conditions
Bruce Protocol
Treadmill speed/gradient increased
incrementally
Exercise to exhaustion
ECG can be monitored to evaluate
effect of exercise on heart