* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download penicillins
Neonatal infection wikipedia , lookup
Bottromycin wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Kharkiv National Medical University
Department of Pharmacology and Medical Prescription
assistant Gordiychuk D.
“Antibiotics part I”
Plan of lecture:
Principles of antibiotictherapy.
Pharmacology of Penicillins, Cephalosporines,
Carbapenems and Monobactams.
Antibiotics
Antibiotics and vaccines are among the biggest
medical advances since 1000. (Culver Pictures)
Antibiotics ("Anti" – against, "bios" - life)
Antibiotics - a substance produced by microorganisms, or
produced from vegetable and animal tissues, and their semisynthetic and synthetic analogs selectively inhibit the viability of
microorganisms sensitive to them.
Importance of Antibiotics:
The elimination of the global crisis of infectious diseases (cholera, plague,
dysentery).
Effective at the dangerous diseases (sepsis, meningitis, peritonitis,
pneumonia).
≈ 20 million people die each year from infectious diseases.
1/3 of all hospital patients are treated with antibiotics.
Over the past 20 years there were 20 new infectious diseases (Legionnaires'
disease, hairycell leukemia, hemorrhagic fever and others).
Unconventional use of antibiotics: peptic ulcer, asthma, myocardial
infarction, atherosclerosis.
In breadth of application group of antibiotics ranked the first place in the
world.
Today, there is no person at least who did not use antibiotics.
There is no country that doesn’t threat of epidemics and pandemics.
Antibiotics could be
narrow-spectrum and effective only
against a limited variety of pathogens or
broad-spectrum, affecting many different
types of pathogens
bactericidal if they kill the susceptible
bacteria or bacteriostatic if they inhibit
the growth of bacteria
Classification of antibiotics.
I. Β-lactams
1.
Penicillins:
2. Cephalosporins
3. Carbapenem and
monobactams
Natural
VI. Polymyxins
VII. Gramicidin
II. Glycopeptides
Semi-synthetic
VII. Cycloserine
III. Macrolides and
Antistaphylococcal Azalides
IX. Antifungal
Aminopenicillins
Antipseudomona
IV. Tetracycline
X. Lincosamides
V.Aminoglycosides XI.Chloramphenicol
Combined
XII. Fuzidin
A brief history of antibiotics
1928 - Scottish microbiologist A. Fleming discovered
penicillin - P. notatum.
1940 - British W. Florey and Chain received penicillin
E.
In 1945, Fleming, Florey, Chain received the Nobel
Prize for the discovery of penicillin.
1942 - Z. Yermolyeva - Penicillin crustosum.
1944 - American Z. Waxman – streptomycin.
1960-1980 - cyclosporine, rifampicin, semisynthetic
penicillins, tetracyclines, macrolides, azalides.
Today ≈ 6 thousand antibiotics. But, 2-3% of them are
use (300 INN ≈ 2000 oficinal names).
~ recent year: modifying old drugs, finding new discipline
in antibacterial combats.
Requirements for Antibiotic
high selectivity
lack of toxicity
long-term providing of therapeutic
concentrations
lack of rapid resistance development
availability of suitable dosage forms
Classification according SPECTRUM OF ACTION.
Narrow spectrum (mainly Gr + and Gr-):
Natural, antistaph. penicillins
Cephalosporins I generation, monobactams
Polimyxins, gramicidin C
Fuzidin
Antifungal
Broad-spectrum:
Semi-synthetic penicillins and cephalosporins II -IV
Carbapenems, Tetracyclines, Macrolides,
Aminoglycosides
Chloramphenicol
Antimicrobial drugs have also been
classified broadly into:
1. bacteriostatic, i.e. those that act primarily
by arresting bacterial multiplication, such as
tetracyclines, chloramphenicol, macrolides,
lincosamides.
2. bacteriocidal, i.e. those which act primarily
by killing bacteria, such as penicillins,
cephalosporins, aminoglycosides, isoniazid
rifampicin, quinolones etc.
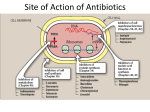
Classification according MECHANISM OF ACTION
INHIBIT:
the synthesis of
the components
of microbial wall
the function of
the cytoplasmic
membrane
the synthesis of proteines
β- LACTAMS
POLIMYXINES
GLYCOPEPTIDES
GRAMICIDINE
LINCOSAMIDES*
RIFAMYCINS
AZALIDES
FUZIDIN
TETRACYCLINES* CHLORAMPHENICOLES*
PHOSPHOMYCINE
CYCLOSERINE
ANTIFUNGAL
MACROLIDES*
AMYNOGLYCOSIDES
Has bactericidal and bacteriostatic* effect
Bacterial cell
Cytoplasmic membrane
Cell wall
Nuclear apparatus
Ribosomes
Violation
of the cell wall
synthesis.
B-lactams
Glycopeptide
Violation
of cytoplasmic
membranes
permeability.
Polymyxins
Gramicidin
Antifungal
Violation
of RNA
synthesis
Rifampicin
Violation
of protein
synthesis at the
level of
ribosomes.
Tetracyclines
Chloramphenicols
Lincosamides
Macrolides
Azalides
Aminoglycosides
Fuzidinum
Negative effects of Antibiotics:
1.The emergence of sustainability:
production of beta-lactamase;
changes in the permeability of the cytoplasmic membrane;
changes in the structure of certain portions of ribosomes
proteins or enzymes
2. Superinfection;
3. Dysbiosis;
4. Allergic reactions;
5. Systemic toxicity, nephrotoxicity, hepatotoxicity.
Penicillins are the least toxic!!!
•Antimicrobial therapy and pregnancy
•Azithromycine
•Erythromycine
•Penicillins
•The most of
cefalosporines
Conditions for rational use of antibiotics
Antibiotics should be given according to antibiogram.
Choose the most active and least toxic antibiotic.
To determine the optimal antibiotic dose and route of
administration based on the its pharmacokinetic and the
concomitant disease. The concentration of antibiotic in the
blood should be 3-4 times bigger in comparison with
minimum inhibitory concentration for the selected
pathogen.
Apply the first striking dose, followed by supporting.
To determine the tolerance of antibiotics in patients according
to the basis of medical history.
To take in account an adverse effects of antibiotics,
especially in the liver and/or kidney failure.
Early antibiotic treatment till consolidation of therapeutic
effect.
Consideration of cross sensitivity.
Use a combination of antibiotics in order to expand and
strengthen the action of the antibacterial effect.
Use of antifungal drugs to prevent dysbiosis.
BETA-LACTAM ANTIBIOTICS
(inhibitors of cell wall synthesis)
Their structure contains a beta-lactam
ring.
The major subdivisions are:
(a) penicillins whose official names
usually include or end in “cillin”
(b) cephalosporins which are
recognized by the inclusion
of “cef” or “ceph” in their
official names.
(c) carbapenems (e.g. meropenem,
imipenem)
(d) monobactams (e.g. aztreonam)
(e) beta-lactamase inhibitors (e.g.
clavulanic acid, sulbactam).
β-lactams Mechanism of Action
Action target: cell wall
on penicillin binding proteins (PBPs)
Transpeptidases (form cross-links in peptidoglycan)
Beta-lactam ring attached to 5-membered
thiazolidine ring
Accessibility of PBPs differ in gram+ and gram- bacteria.
Amino acyl side chain groups determine spectrum,
adsorption, susceptibility to lactamase.
Bactericidal inhibitors.
Penicillin
Classification of penicillins
1.Natural penicillins:
a) Short acting:
Penicillin-G
Penicillin-sodium
Penicillin-potassium
Penicillin V
b) Long acting:
Penicillin G. procaine
Benzathine penicillin (Bicillin-I)
Bicillin-3,-5
Classification of penicillins
2. Semisynthetic penicillins:
I. Penicillinase resistant
Oxacillin
Dicloxacillin
Cloxacillin
Methicillin
II. Broad spectrum penicillins
Aminopenicillins
Ampicillin
Amoxicillin
Pivampicillin
Talampicillin
Classification of penicillins
III. Carboxypenicillins
Carbenicillin
Ticarcillin
IV. Ureidopenicillins
Azlocillin
Piperacillin
V. Combined penicillins
Unazin
Ampiox (Ampicillin+Oxacillin)
Augmentin (Amoxycillin+Clavulanic acid)
Magnapen (Ampicillin+Flucloxacillin)
Spectrum of natural penicillins
Gr+ microorganisms include:
staphylococci,
streptococci (pneumoniae, pyogenes and
viridans group),
bacillus anthracis,
clostridium perfringens,
corynebacteria diphtheriae and listeria
monocytogenes
Spectrum of natural penicillins
(cont.)
Sensitive Gr- microorganisms include:
Neisseria gonorrhoeae,
Neisseria meningitis,
Leptotrichia buccalis,
Treponema pallidum,
Treponema partenue.
Pharmacokinetics of natural
penicillins
1. Acidic instability (exception Penicillin V)
2. Extracellular distribution mainly
3. Poor penetration through BBB
4. Crossing the placenta
5. Protein binding 60%
6. Small amount metabolizing
7. Excretion mainly by tubular secretion. It
may be suppressed by probenecid (uricosuric)
Clinical uses of natural penicillins
Endocarditis
Pericarditis
Meningitis
Pneumonia
Septicemia caused by streptococcus pyogenes
Gonorrhea
Syphillis (congenital and neurosyphillis).
Clinical uses of natural penicillins
(cont.)
Anthrax,
Actinomycosis (abdominal, cervicofacial or
thoracic disease),
Botulism,
Gas gangrene,
Tetanus,
Diphtheria (prevention of carrier state),
Empyema,
Rheumatic fever,
Listeriosis.
Side effects of natural penicillins
Penicillin G (benzyl penicillin) is one of the least
toxic antibiotics. It does not cause any direct
toxicity. Only in very high doses, especially
injected IV, it can cause neurotoxic effect and
bleeding.
The hypersensitivity reactions are the major
problem, incidence up to 10%.
Semisynthetic penicillins
I. Penicillinase resistant:
Oxacillin, Dicloxacillin, Cloxacillin,
Methicillin
The advantages of penicillinase resistant
semisynthetic penicillins over natural ones are
in efficacy against penicillinase producing
staphylococci and stability of some of them
(Oxacillin) in acidic medium.
They are used in treatment of infection
caused by staphylococci resistant to
penicillins.
Semisynthetic penicillins
II. BROAD SPECTRUM PENICILLINS
a) Aminopenicillins
Amoxycillin and Ampicillin
The aminopenicillins have identical spectrum and
activity, but amoxicillin is better absorbed orally
(70–90%).
They are effective against:
streptococci, enterococci
Gram-negative organisms (including H. pylori)
but have variable activity against staphylococci
ineffective against P. aeruginosa.
b) Antipseudomonal penicillins
These drugs retain activity against streptococci and
possess additional effects against Grorganisms, including various Enterobacteriaceae
and Pseudomonas.
•Carboxypenicillins
- Carbenicillin
- Ticarcillin
•Ureidopenicillins
- Azlocillin
- Mezlocillin
- Piperacillin
There is cross-allergy between all the various
forms of penicillin, probably due in part to their
common structure, and in part to the degradation
products common to them all.
Partial cross-allergy exists between penicillins
and cephalosporins (a maximum of 10%) which
is of particular concern when the reaction to either
group of antimicrobials has been angioedema or
anaphylactic shock.
Carbapenems and the monobactams
apparently have a much lower risk of cross-reactivity.
Adverse effects
Thrombophlebitis
Allergic reactions
Superinfections (diarrhea)
Seizures (rare)
Stevens – Johnson
syndrome
Lyell
syndrome
Resistance
Failure to bind to PBPs
Cannot penetrate porins (gram-)
Production of lactamase (penicillinase)
Lack autolytic enzyme
B-lactamase
Types:
Different substrate specificity
Penicillinases
Cephalosporinases
Location:
Gram+: extracellularly
Gram-: periplasmic space
Policy to deal drug resistance
Ideally, bacteriological management of
clinical infection should involve:
1. Identification of causative organism
2. Sensitivity test
3. Follow-up the drug effect
4. Monitor antibiotic level to avoid toxicity.
In reality, most patients requiring
antimicrobial therapy are treated empirically.
In serious infections immediate chemotherapy
may be life-saving.
CEPHALOSPORINS
Cephalosporins have 7-aminocephalosporanic
acid nucleus.
Cephalosporins are produced semisynthetically
from cephalosporin- C obtained from a fungus
Cephalosporium.
Spectrum – broad
Mechanism - inhibition of synthesis of bacterial
cell wall.
Effect - bactericidal
5 generations
of CEPHALOSPORINS
1.FIRST GENERATION
Cephalosporins of the first generation are highly active against
Gram+ but weaker against Gram- microorganisms.
I.Cefazolin
II.Cefalexin
2. SECOND GENERATION
The drugs were developed subsequently to the first generation;
they are more active against Gram-negative microorganisms.
III.Cefuroxim
IV.Cefaklor
5 generations of CEPHALOSPORINS (cont.)
3. THIRD GENERATION
They have enhanced activity against gram-negative bacilli,
including most enteric organisms and Serratia marcescens.
Ceftriaxone and cefatoxime have become agents of choice in
the treatment of meningitis.
Ceftazidime has activity against Pseudomonas aeruginosa.
V.Ceftriaxone
VI.Cefixime
VII.Cefoperazone
VIII.Ceftazidime
IX.Cefatoxime
5 generations of CEPHALOSPORINS (cont.)
4. 4-th generation
These drugs are in many ways similar to
cephalosporins of 3rd generation
X. Cefepim
XI.Cefpirom
5. 5-th generation
XII.Ceftobiprole
XIII. Ceftaroline
Antimicrobial activity: Ceftobiprole has powerful
antipseudomonal effect and is less susceptible to
development of resistance. Ceftaroline does not have
an anti-pseudomonal activity.
CEPHALOSPORINS
Type of action: bactericidal = penicillins
Spectrum: WIDE
INDICATIONS
infectious diseases of the respiratory, urinary and
biliary tract, abdominal cavity, skin, bones, joints,
heart,
Gonorrhea, burns, surgical prophylaxis,
Meningitis and Pseudomonas infection - III -IV
generation.
Side effects: hemorrhage, hemato-, nephro-, neuro-,
hepatotoxicity.
Contraindications: porphyria, epilepsy, severe liver
and kidney diseases, pregnancy, lactation.
Sulperazon - "protected"
(Cefoperazone + Sulbactam)
Spectrum: wide G+, Gr-, anaerobes
Resistant to β-lactamases of extended
spectrum (sulperazon and carbapenems)
Application: for severe community-acquired
and hospital-acquired infective processes:
primary and secondary peritonitis, infected
pancreatic necrosis, sepsis, diabetic foot,
phlegmons, nosocomial pneumonia.
Comparison activity of
CEPHALOSPORINS.
Activity
Generation
1-st
2-st
3-st
4-st
Gr+
Gr-
+++
+/-
++
+
+
+++
++
+++
Pharmacological "face" of
CEFALOSPORINES
Similar to penicillin in structure and action.
Wide spectrum.
Powerful bactericidal effect.
Low toxicity.
Good compatibility with other antibacterial
agents.
Most resistant to staphylococcal β-lactamase.
Cross allergic to penicillin.
It penetrates into the tissue fluid, joints, bones.
Good compatibility with other antibacterials.
CARBAPENEMS and MONOBACTAMS
CARBAPENEMS
MONOBACTAMS
1. IMIPENEM-CILASTATINE
2. MEROPINEM*
3. AZTREONAM
MECHANISM: inhibit the PBPs (transpeptidase), Imipenem - PBPs-2.
SPECTRUM
ultra-wide: the majority of aerobic
and anaerobic Gr+ and Gr- resistant
bacteria; 80% of strains of
Pseudomonas aeruginosa,
postantibiotic effect (Gr-).
narrow: Gr- aerobes: gono-,
meningococcus, Salmonella, Shigella,
Klebsiella, Proteus and Escherichia
coli, Pseudomonas etc.
INDICATIONS
severe infections of bones and joints,
skin and soft tissue, abdominal,
female genitals, urinary tract
infections, pneumonia, septicemia,
meningitis.
- resistant to -lactamases,
severe infections caused by Gr- flora
resistant to III generation
cephalosporins, aminoglycosides II-III
generation, pseudomonas penicillins.
* - resistant to renal dehydropeptidase
Pharmacological «face» of CARBAPENEMS and
MONOBACTAMS
CARBAPENEMS
MONOBACTAMS
Ultra-wide spectrum,
including strains resistant to
cephalosporins III and IV
generation.
Potent resistance to βlactamase.
Potent postantibiotical effect.
Slow development of
resistance.
Antibiotics of ultradeep
reserve!
Low toxicity and good
tolerability.
The narrow spectrum of action
(aerobic Gr-), identical to
cephalosporins III.
Potent resistance to Grβ-lactamase.
Potent bactetiocidal action.
Slow development of
resistance.
No cross-sensitization to
penicillins and cephalosporins.
The use in newborns.
Antibiotics of reserve!
Side effects of MONOBACTAMS AND
CARBAPENEMS
CARBAPENEMS
MONOBACTAMS
CRAMPS,
Allergic reactions:
WEAKNESS,
TREMOR,
ENCEPHALOPATHY,
HYPOTENSION,
NAUSEA, VOMITING,
SUPERINFECTION,
PSEUDOMEMBRANOUS
COLITIS,
PHLEBITIS,
THROMBOCYTOSIS,
EOSINOPHILIA.
URTICARIA,
PRURITUS,
ERYTHEMA,
EOSINOPHILIA,
ARTHRALGIA,
VASCULITIS,
ANGIOEDEMA,
BRONCHOCONSTRICTION,
ANAPHYLAXIS.