* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download MICR 454L - Cal State LA - Instructional Web Server
Bacterial morphological plasticity wikipedia , lookup
Horizontal gene transfer wikipedia , lookup
Infection control wikipedia , lookup
Neonatal infection wikipedia , lookup
Urinary tract infection wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Methicillin-resistant Staphylococcus aureus wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Triclocarban wikipedia , lookup
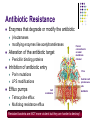
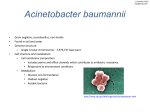
MICR 420 Emerging and Re-Emerging Infectious Diseases Lecture 3: Challenge of Antibiotic Resistance S. aureus (MRSA), E. faecalis (VRE), A. baumannii Dr. Nancy McQueen & Dr. Edith Porter Overview Challenge of antibiotic resistance S. aureus E. faecalis Methicillin resistance Vancomycin resistance A. baumannii MDR Morphology Virulence factors Diseases Diagnosis Culture, biochemicals PCR: toxin production Antibiogram Penicillin binding protein 2a latex agglutination assay Challenge of Antibiotic Resistance Antibiotic resistance Resistance genes Transfer of resistance genes Antibiotic Resistance Enzymes that degrade or modify the antibiotic Alteration of the antibiotic target Penicillin binding proteins Funnel connection to an outer membrane channel Inhibition of antibiotic entry b-lactamases modifying enzymes like acetyltransferases Porin mutations LPS modifications Efflux pumps Pore Central cavit promiscuous site Cell membrane Tetracycline efflux Multidrug resistance efflux Resistant bacteria are NOT more virulent but they are harder to destroy! Antibiotic Resistance Genes Plasmid and chromosomal encoded Spontaneous mutations E.g., Plasmid: beta-lactams, aminoglycosides E.g.,Chromosomal: fluoroquinolones, tetracyclines At low doses of antibiotics Acquisition of resistance genes Acquisition of Resistance Genes Inherited Horizontally Conjugation Less efficient Transduction Cell to cell contact Virus-mediated Transformation Uptake of free DNA Occurs also between distantly related genera such as between gram-positive and gram-negative bacteria! Major Causes for Increased Antibiotic Resistance Distribution of Antibiotics Manufactured in the U.S. (Currently about 50 Million Pounds per Year) Human Animal Agriculture Improper use in medicine After Stuart B. Levy in “The Challenge of Antibiotic Resistance” Incomplete therapy Inappropriate use for viral infections Unnecessary use of broadspectrum antibiotics Low dose use in animal husbandry to promote animal growth Use in agriculture leads to unwanted distribution of aerosols Detection of Antibiotic Resistance Conventional antibiotic disk diffusion (Kirby Bauer) and determination of minimal inhibitory concentrations DNA microarrays for detection of plasmidmediated antimicrobial resistance (and virulence factor) genes Active Learning Exercise What role do transposons play in antibiotic resistance? Staphylococcus aureus Staphylococcus aureus MSA Agar Plates Gram positive cocci In clusters Facultative anaerobic Catalase positive Mannitol positive Coagulase positive Often beta-hemolytic Normal flora (low numbers) S. epidermidis Nostrils Pharynx Perineal S. aureus S. aureus: Virulence Factors Coagulase Various enzymes Protein A Wound Infections Purulent infections Binds antibodies via Fc receptor Various toxins Enterotoxins Exfoliative toxin (epidermiolysin) Toxic shock syndrome toxin Toxin specific diseases S. aureus Food Intoxication Uptake of preformed enterotoxin Nausea, vomiting, diarrhea Self limited Short duration Staphylococcal Exfoliative Toxin: SSSS Staphylococcal scalded skin syndrome Cleaves cell adhesion molecules of keratinocytes (desmoglein) (http://dermatlas.med.jhmi.edu/derm/) Toxic Shock Syndrome First described in menstruating women using certain types of tampons High fever, rash, skin peeling in palms, shock, multiple organ failure Staphylococcus TSST production triggered in these tampons TSST resorption through vaginal mucosa Toxic Shock Syndrome Pathogenesis Superantigen mediated Uncontrolled immune response to staphylococcal and streptococcal toxins Early signs Fever Dizziness Confusion Flat red rash over large areas of the body Shock and multi-organ failure Superantigens Activate numerous T Helper cells simultaneously T Helper cells release numerous proinflammatory cytokines Bacterial Superantigens Staphylococcal superantigens S. aureus Over 20 described TSST, exfoliatins, enterotoxins Streptococcal S. pyogenes (Group A beta-hemolysing streptococci) Exotoxin A and C, and others New Threats by S. aureus Nosocomial infections (healthcare-associated infections, HAIs) 15% of all isolates; 8% of all HAIs Spread of MRSA in the community Vancomycin resistant MRSA Methicillin Resistance High level resistance encoded by MecA Encodes alternative penicillin binding protein PBP2a Structural changes in transpeptidase penicillin-binding proteins Plays role in peptidoglycan synthesis Low affinity of binding to beta-lactams Carried by staphylococcal cassette chromosome mec (SCCmec) Unique mobile genetic element Integrated into the S. aureus chromosome Composed of the mec gene complex encoding methicillin resistance and the ccr gene complex that encodes recombinases responsible for its mobility These elements also carry various resistance genes for nonbeta-lactam antibiotics Spread of MRSA S. aureus in the Community Adam H et al. Fatal case of post-influenza, community-associated MRSA pneumonia in an Ontario teenager with subsequent familial transmission. Can Commun Dis Rep. 2007 Feb 15;33(4):45-8. van der Flier M et al. Fatal pneumonia in an adolescent due to community-acquired methicillin-resistant Staphylococcus aureus positive for PantonValentine-leukocidin. Ned Tijdschr Geneeskd. 2003 May 31;147(22):1076-9. Francis JS et al. Severe community-onset pneumonia in healthy adults caused by methicillin-resistant Staphylococcus aureus carrying the PantonValentine leukocidin genes. Clin Infect Dis. 2005 Jan 1;40(1):100-7. First Reports of Vancomycin Intermediate and Resistant MRSA Hososaka Y et al. Nosocomial infection of betalactam antibiotic-induced vancomycin-resistant Staphylococcus aureus (BIVR). J Infect Chemother. 2006 Aug;12(4):181-4. Resistance mechanism described for VISA Sequential point mutations in key global regulatory genes associated predominately with cell wall thickening and restricted vancomycin access to its site of activity in the division septum (Howden et al., 2010) Enterococcus faecalis Enterococcus faecalis Gram positive cocci In pairs and chains Catalase negative Non-hemolytic Facultative anaerobic Bile esculin positive Normal flora in intestine Often highly resistant to antibiotics Nosocomial infections Urinary tract infection Wound infections Endocarditis Vancomycin resistance observed E. faecalis Virulence factors Surface protein (ESP) Adherence Antiphagocytic Variations observed Escapes immune response Vancomycin Resistant E. faecalis (VRE) Vancomycin binds to an essential substrate at a late stage of the biosynthetic pathway of peptidoglycan (Reynolds 1989) D-Ala-D-Ala in peptidoglycan precursor Vancomycin resistance is caused by the production of depsipeptide D-Ala-D-Lac, which replaces D-Ala-D-Ala (Gin and Zhanel, 1996) Results in a more-than1,000-fold lowering of the affinity of vancomycin for its target (Reynolds and Courvalin, 2005). New Threats by E. faecalis Spread of VRE in the hospital setting Zubaidah et al. Hospital-acquired vancomycin-resistant enterococci: now appearing in Kuala Lumpur Hospital. Med J Malaysia. 2006 Oct;61(4):487-9. Comert et al. First isolation of vancomycin-resistant enteroccoci and spread of a single clone in a university hospital in northwestern Turkey. Eur J Clin Microbiol Infect Dis. 2007 Jan;26(1):57-61. Vonberg et al. [Prevention and control of the spread of vancomycin-resistant enterococci : Results of a workshop held by the German Society for Hygiene and Microbiology.] Anaesthesist. 2007 Feb;56(2):151-7. Huang et al. Risk of acquiring antibiotic-resistant bacteria from prior room occupants. Arch Intern Med. 2006 Oct 9;166(18):1945-51. Bar et al. Systemic inflammatory response syndrome in adult patients with nosocomial bloodstream infections due to enterococci. BMC Infect Dis. 2006 Sep 26;6:145. Furtado et al. Risk factors for vancomycin-resistant Enterococcus faecalis bacteremia in hospitalized patients: an analysis of two case-control studies. Am J Infect Control. 2006 Sep;34(7):447-51. Acinetobacter baumannii Acinetobacter baumannii Pleomorphic gramnegative or gramvariable coccoid rods Short, fat rods, resemble cocci and diplococci Can be confused with Neisseria spec. Non-motile Non-fermenter Biofilm production contributes to antibiotic resistance (Dallo SF, Weitao T 2010) http://www.cyberspaceorbit.com/AB_picenh2.jpg Threats by Acinetobacter baumannii Increasingly isolated in hospital settings (war and natural disaster victims) Wound infections Septicemia Increasingly resistant Outbreaks of infections with carbapenem resistant A. baumannii production of carbapenemases (metallobetalactamases, CRAB) Worldwide spreading of resistant strains http://www.bioquell.com/Pictures/Acinetobacter%20map.jpg World Wide Spread of Acinetobacter Infection. 2010 Apr 1. Successful treatment of three children with postneurosurgical multidrug-resistant Acinetobacter baumannii meningitis. Ozdemir H et al (Turkey) J Infect Dev Ctries. 2010 Mar 29;4(3):164-7. In vitro antimicrobials activity against endemic Acinetobacter baumannii multiresistant clones. Rodriguez CH et al. (Buonos Aires) Scand J Infect Dis. 2010 Mar 26. The microbiological characteristics of patients with crush syndrome after the Wenchuan earthquake. Wang T et al. (China) J Hosp Infect. 2010 Mar 18. Emergence of an extreme-drug-resistant (XDR) Acinetobacter baumannii carrying bla(OXA-23) in a patient with acute necrohaemorrhagic pancreatitis. Grosso F et al. (Portugal) J Med Assoc Thai. 2009 Dec;92 Suppl 7:S173-80. Clonal spread of carbapenem resistant Acinetobacter baumannii in the patients and their environment at BMA Medical College and Vajira Hospital. Phumisantiphong U et al. (Thailand) Increasing Nosocomial Infections with Drug Resistant A. baumannii Search Terms* 1988 1998 2008 2009 AB & infection 1 27 181 172 AB & nosocomial 0 16 72 78 AB & resistant 1 23 186 226 Take Home Message Increasing antibiotic resistance is a major threat to public health. Of particular concern are MRSA, VISA and VRSA, VRE, and A. baumannii. Antibiotic resistance is mediated by expression of enzymes inactivating the antibiotic, alteration of the drug target, prevention of drug entry into the cell, and drug efflux pumps. Inappropriate drug use is the major cause. Resources Microbiology: An Introduction, by Tortora, Funke and Case; Pearson Prentice Hall; 9th ed, 2007, Chapter 11; pp 436t, 591, 593, 606. 633b Current Issues: pp 62 -71 Alekshun MN and Levy SB (2007) Molecular mechanisms of antibacterial multidrug resistance. Cell 128(6):1037-50 Emerging Infectious Diseases: pp28 – 30 http://www.microbelibrary.org CDC fact sheets http://dermatlas.med.jhmi.edu/derm/ Hiramatsu K, Cui L, Kuroda M, Ito T. The emergence and evolution of methicillin-resistant Staphylococcus aureus. Trends Microbiol. 2001 Oct;9(10):486-93. Embedded in slides