* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Non odontogenic inflammation diseases
Traveler's diarrhea wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Onchocerciasis wikipedia , lookup
West Nile fever wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Antibiotics wikipedia , lookup
Gastroenteritis wikipedia , lookup
Marburg virus disease wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Hepatitis C wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Sarcocystis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Trichinosis wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Hepatitis B wikipedia , lookup
Oesophagostomum wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Neonatal infection wikipedia , lookup
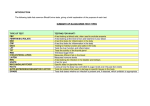
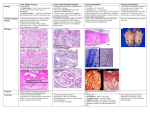
Inflammatory disease of maxillofacial area (odontogenic and non odontogenic). CLASSIFICATION OF INFLAMMATORY PROCESSES OF MFA. PERIOSTITIS, OSTEOMYELITIS, ABSCESS, PLEGMONAS: ETIOLOGY, PATHOGENESIS, CLINICAL COURSE OF, COMPLICATIONS, PROPHYLAXIS. Course of maxillofacial surgery and stomatology of Tashkent Medical Academy, associate professor Sh.A.Boymuradov Table of Content Overview General symptoms of inflammation Clinical manifestations of inflammation Differential diagnosis Causes Spectrum of bacterial therapy Prevalence of different abscesses Classification of abscesses Overview Inflammation is a defence reaction of the organism to local injuries of any type, to infection. Infection is a pathological state resulting from the invasion of the body by pathogenic microorganisms and their proliferation within the organism. Inflammation diseases Non odontogenic Odontogenic Non odontogenic inflammation diseases 1. Fufuruncle 2. Anthrex 3. erysipelas 4. Sibir canker 5. Noma (gangrenuos stomstitis) Non-odontogenic causes of soft tissue infections Infected fracture Infected soft tissue wounds or tumors Infection by foreign bodies Infection after injection Inflammatory of skin or mucosal membrane disorders Haematogeneous or lymphogeneious spreading Furuncle (inflammation of pileous follicle) Anthrex (inflammation a lot of pileous follicle) Complication of furuncle of the face: Tromboflibitis of vein Facial vassels Triangle of the death Odontogenic inflammation disesases of the face 1. Acute odontogenic periostitis 2. Acute osteomyelitis of jaws 3. Odontogenic abcsesses 4. Odontogenic phlegmonas 5. Odontogenic lymfadinitis Odontogenic centre of the inflammation Classic signs of acute infection appear Heat Redness Tumor (oedema) Loss of function (trismus, difficult to swollow speech) Additional: leucocytosis and CRP increasis CRP (C-reactive protein) is synthesised in the liver. It is one of the chemical mediators of inflammation and its serum level increases faster and to higher levels than that of any other parameters in acute infectious and non-infectious inflammation. Therefore, CRP belongs to the group of acute-phase proteins. These are blood lipids the concentration of which increases in the course of inflammatory diseases. CRP binds to invading foreign substances and activates important steps of the immune system with macrophages and the complement system. Due to its relatively short half-life of 24 hours, changes in CRP concentration indicate changes in the inflammatory process. Odontogenic chronic inflammation centre Inflammation centre The clinical picture of acute periostitis of the jaws. 1.Presence of causal teeth 2. Smoothness of a transitive fold 3. Fluctuation of a transitive fold 4. Painful percussion of causal tooth Increases of temperature up to 38 гр Dysfunctions: opening of a mouth, chewing, speech, swallowing. Acute odontogenic periostitis Tipes of osteomyelitis of the jaw on the pelationship of causes 1. Odontogenig osteomylitis 2. Traumatic osteomylitis 3. Hematogen osteomylitits Development infections from a top of a root of a tooth The theory of progress of osteomylitis of jaws 1. The infectious-embolic theory Infringements innervation of jaws The theory a sensitization The mechanism of progress of an infection Stages of current of an osteomyelitis of jaws 1. Acute 2. under acute 3. chronic Clinical picture of a acute osteomyelitis 1 Looseness of a causal tooth Infringement of function: opening of a mouth, chewing, speeches and swallowing Mobility of a several teeth Smoothness of a transitive fold from two sides. Rise in temperature of a body up to 41 гр. Fever Acute necrotic osteomyelitis Treatment of osteomyelitis of laws Elimination of cause (causal teeth extraction) Incision discharge of pus Spreading of the abcsses cavity Osteoperforation of injure bone drainage of the pus cavity Facultative antibiotic treatment Types of abscesses and phlegmonas 1. Superficial located 2. middle deep located 3. deep located Abscess submucous abscess, smooth vestibule Localized collection of pus an a cavity caused by necrosis of tissue due to bacterial infection Demarcation by abscess mambrane (granulation tissue) Firm elastic consestence Fluctuation can be palpated only in superficial abscesses Odontogenic abscesses Oedema Oedematous swelling of the ocular region in abscess of the canine fossa concomitant oedema of the upper lip in submucous abscess in region 11 accumulation of fluid in tissue classic sign of any acute inflammation (tumour) soft and elastic on palpation. Due to the anatomical situation in the maxillofacial region, the typical fluctuation of an abscess is absent in the majority of cases or only rarely identifiable Differential diagnosis of abcsesses swelling caused by neoplasms (sarcomas, malignant lymphomas, carcinomas) salivary gland diseases Inflammation more 2 anatomical region (phlegmonas) Phlegmon (cellulitis) diffusely spreading inflammation between superficial tissue levels (without being limited to them) No demarcation infection by highly virulent bacteria (release of lytic enzymes) impaired defence mechanisms of the organism serous-purulent and necrotising inflammation serous-purulent and necrotising inflammation firm to hard on palpation Several phlegmonas submandibular and parapharigial region Odontogenic causes of soft tissue infections In 92-94% of the cases, infections in the oromaxillofacial region are of odontogenic origin Periapical periodontitis Infection after teeth extraction difficult dentition (pericoronitis) Marginal priodontitis infected retained root fragments Phlegmona of infrairbital region CT ckanner of inflammation diseases Orbital phlegmonas Orbital pflegmona Anaerobic flora Odontogenic infections are always caused by a mixed flora of aerobic and anaerobic bacteria. The count of anaerobic bacteria always outnumbers that of aerobic bacteria (at least by 102). Pure anaerobic mixed infections also occur. Anaerobic bacteria play a predominant role in the generation and spreading of odontogenic soft tissue infections. Infection by clostridia as well as mixed infections by yeasts and bacteria may occur Several phlegmona of flor of mouse (ludvig angina) Therapy The following statement that Galen made almost 2,000 years ago - "ubi pus, ibi evacua" (if there is pus, remove it) which is still valid in the era of antibiotics could be considered the clinical conclusion from the abscess pathophysiology explained above. Therefore, incision and drainage are the primary therapy of an phlegmonas Incision of an abscess is advisable, possibly by a sufficiently wide incision at the maximum point of the swelling. Obtain sufficient discharge of pus with the incision. Prepare for drainage of the purulent exudate In smaller abscesses, it is usually sufficient to insert a Iodoform gauze packing strip for 2-3 days; extensive abscess cavities are drained through a tube that is fixed in place with sutures rinsing of the abscess Culture and antibiotic sensitivity testing Antibiotics for parenteral therapy Infections are classified as mild, moderate or severe infections. Differential surgical and antibiotic treatment is indicated according to the extension tendency and severity grade of infection as well as the general condition of the patient. Health teeth, no complication Thank you for attention