* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Filariasis
Hepatitis B wikipedia , lookup
Sarcocystis wikipedia , lookup
Hepatitis C wikipedia , lookup
Trichinosis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Neonatal infection wikipedia , lookup
Plasmodium falciparum wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
Schistosomiasis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Loa loa filariasis wikipedia , lookup
Oesophagostomum wikipedia , lookup
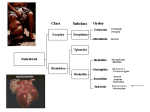
Soil transmitted nematodes • Ascaris lumbricoides • Trichuris trichiura • Ancylostoma duodenale • Necator americanus • Strongyloides stercoralis Soil-transmitted nematodes Parasitic nematode of human importance Disease Lymphatic filariasis : Agent Wucheraria bancrofti Vector-borne nematode Lymphatic disease Elephantiasis WHO elimination programme • 8 species of filariae parasitise humans • Occur in a wide range of habitats lymph glands, deep connective tissue, subcutaneous tissue or mesenteries • Intermediate host or vector (insect) • Adult worms parasites of vertebrate hosts which produce characteristic larvae known as microfilariae Filarial nematodes Filarial nematodes • 3 of the species are primarily responsible for most cases of human filariasis (Two billion exposed and at least 200 million infected) – Wucheraria bancrofti (lymphatic) – Brugia malayi (lymphatic) – Onchocerca volvulus (subcutaneous) Wucheraria bancrofti • Primary causative agent of lymphatic filariasis • Overt bancroftian filariasis : 115 million cases worldwide (45.5 million India, 40 million subsaharan Africa) • Widespread throughout the subtropics and tropics (for e.g. Central Africa, India, Thailand, Malaysia, Phillipines, Pacific Islands, Haiti, coastal Brazil) Different stages of the Wucheraria life cycle Onchocerca volvulus : Onchocerciasis • Periodic form : mf in small numbers in circulating blood during the day and peak density at night (10 pm to 2 to 4 pm) • Subperiodic form : mf peak between noon and 8 pm • Periodic form mosquitoes feed at night ; subperiodic form mosquitoes feed during the day Microfilarial periodicity Gold standard diagnosis using blood films has diminished relevance as mass drug distribution expands Use of sentinel sites for ongoing night blood films Diagnosis of Wucheraria • Frequently made on clinical grounds in endemic regions but demonstration of microfilariae in circulating blood is key • Where more than one species of filarial infection occurs need well stained slides for morphological identification of microfilariae • Filarial infections can occur without microfilaremia Diagnosis : Wucheraria bancrofti • Conventional method examination of thick smear (stained)(counting chamber method) • Concentration techniques (Nucleopore filtration or Knott’s concentration) • Detection of circulating filarial antigen immunochromatographic test (ICT) • Serodiagnosis • PCR-based assays for DNA • Imaging studies (high frequency ultrasound, lymphoscintigraphy) – mf usually in blood – 210-320um in length – Loose sheath which when stained with Giemsa is pale pinky blue and does not stain well – Nuclei are discrete and tail ends taper evenly – No nuclei on the tip of the tail Characteristics of mf of W. bancrofti Symptomatology • Clinical manifestations vary considerably • Asymptomatic microfilaraemics show microscopic hematuria and/or proteinuria • Early signs : fever, lymphangitis (limbs, breasts, scrotum), lymphadenitis (femoral, inguinal, axillary and epitrochlear nodes) • Orchitis, Lymphocoel, Hydrocoel • Elephantiasis Tropical pulmonary eosinophilia (TPE) • Distinct syndrome in some individuals • Paroxysmal cough and wheezing • Weight loss, low grade fever, pronounced blood eosinophilia • Total serum IgE and antifilarial Ab titres raised • Responds well to treatment but in its absence progressive pulmonary damage Elephantiasis • Relatively uncommon and late complication of filariasis • Elephantiasis (enlargement of limbs, scrotum, breasts or vulva with dermal hypertrophy & verrucous changes) • Impairment of circulation means secondary bacterial & fungal infections are common • Inflammatory changes in the lymphatics • Repeated attacks of inflammation lead to dilation & thickening of the affected lymphatics (lymphedema) • Chronic lymphedema : hyperplasia of connective tissue, infiltration of plasma cells, macrophages & eosinophils • Eventual thickening & verrucous changes: elephantiasis Pathology • Intensity and type of host immune response may reflect range of clinical manifestations • Immune response varies by stage of infection Immunology • Immunomodulatory molecules • Experimental animal models (B. malayi not W. bancrofti) Treatment • Diethylcarbamazine (DEC) : an effective microfilaricidal drug which can eliminate adult worms more slowly. Successfully administered in table salt (Mass treatment) • Combination of DEC & Albendazole • Combination of DEC & Ivermectin • Elephantiasis : surgery, rigorous hygiene Prevention and control • Transmission depends upon two issues (availability of vectors and presence of a population of people to infect the vector) • Vector control : larvicides, residual spraying • WHO programme to eliminate lymphatic filariasis (GPELF) : 2 prongs - stop spread of infection & reduce morbidity (mass treatment once yearly for 4-6 yrs, education and intensive local hygiene; GSK and Merck donation) Case study : Mass drug administration in India • Mass treatment of 590 million people • 1.4 billion doses of DEC and 0.51 billion of Albendazole • 1.1 million drug distributors • Challenges : quality of DEC sometimes poor, blister-packaging, side-effects, treatment coverage variability (55-89% in better developed states versus 0-35% in less), monitoring and evaluation weak Lymphatic filariasis elimination programme in India: progress and challenges Kapa D. Ramaiah Parasitology Today (2008) vol 25 (1) 7-8