* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Antiatherosclerotic drugs
Survey
Document related concepts
Environmental impact of pharmaceuticals and personal care products wikipedia , lookup
Pharmacognosy wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Prescription costs wikipedia , lookup
Neuropharmacology wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Transcript
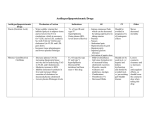
Antiatherosclerotic drugs Learning Objectives: ■ Describe the four main classes of drugs used to treat hyperlipidemia ■ Explain their mechanisms of action, effects upon serum lipid concentrations and ADR Introduction Atherosclerosis is a disease which characterized by intimal thickening and lipid deposition. Hyperlipidemia Endothelial injury Thrombosis Atherosclerosis Smooth muscle cell proliferation Macrophage Inflammatory mechanism Introduction Antiatherosclerotic drugs – Used to prevent or slow progression of atherosclerosis to reduce the risk of coronary artery disease and prolong life Lipid-regulating drugs Antioxidant Endothelium protective drugs Polyunsaturated fatty acids Goals for Lipids & diagnosis of hyperlipidemia • LDL(mg/dL) – – – – – • HDL < 100 →Optimal 100-129 → Near optimal 130-159 → Borderline 160-189→ High ≥ 190 → Very High – < 40 → Low – ≥ 60 → High • Serum Triglycerides – – – – • Total Cholesterol – < 200 → Desirable – 200-239 → Borderline – ≥240 → High • < 150 → normal 150-199 → Borderline 200-499 → High ≥ 500 → Very High Cholesterol (TC, LDL-C, HDL-C) 1 mg/dL = 0.02586 mmol/L • TG 1 mg/dL = 0.01129 mmol/L Treatment of hyperlipidemia – Non-Pharmacological Therapy – 1st line tx • 1. Diet modification – – – – – – – Decrease intake of total fat and especially saturated fat Increase fiber intake Increase Omega-3-fatty acids (found in fish) ↓ homocysteine ↑ fruits and vegetables (antioxidants) ↓ simple sugars (sucrose) Moderate alcohol consumption (EtOH can ↑ TG) 2. Exercise Treatment of hyperlipidemia • Niacin (Nicotinic acid, niaspan®, slo-niacin, Vitamin B3, V-pp) – Decreases VLDL and LDL and significantly ↑ HDL – Mechanism of action (MOA) 1. Inhibits free fatty acid (FFA) release from adipose tissues by inhibiting the intracellular lipase system 2. Increases clearance of VLDL via lipoprotein lipase pathway 3. Inhibits VLDL secretion into the blood thereby preventing production of LDL 4. Reduces circulating fibrinogen (contributes to clot formation) and ↑ tissue plasminogen activator (clot dissolver) 5. HDL catabolic rate is decreased • Niacin –Indications »↓ levels of TG (VLDL) » Mixed elevation of LDL and VLDL (alone or in combination with reductase inhibitors) » Elevation of TG (VLDL) and low levels of HDL (Niaspan® approved for elevating HDL levels) • Niacin - Adverse effects –Flushing »Harmless cutaneous vasodilation »Uncomfortable sensation of warmth »Occurs after drug is started or ↑ dose »Lasts for the first several weeks »Can give 325 mg aspirin 30 minutes before each dose (prevents prostaglandin synthesis). Can also take ibuprofen in place of ASA(acetylsalicylic acid) • Niacin - Adverse effects – Pruritis, rashes, dry skin – acanthosis nigricans (黑棘皮症 , eruption of velvet warty benign growths and hyperpigmentation) » Associated with insulin resistance – Nausea and abdominal discomfort – Hepatotoxicity – Hyperuricemia – Hypotension Antilipemic agents •Fibrates (gemfibrozil [Lopid®], fenofibrate [Tricor®], clofibrate [Atromid-S®], bezafibrate) – – – – Little or no effect on LDL ↓ VLDL (TG) moderate ↑ of HDL MOA » Ligand for the nuclear transcription regulator, peroxisome proliferator-activated receptor-α (PPAR- α) » MOA mostly unknown • Fibrates –MOA »↑ activity of lipoprotein lipase for lipolysis of triglyceride (↑ clearance) »↓ lipolysis in adipose tissue, ↓ FFA release »↓ secretion of VLDL by liver »↓ uptake of FFA by liver »↑ HDL levels moderately • Fibrates – Indication: Hypertriglyceridemia » Gemfibrozil – 600mg QD-BID (half life 1.5hrs) » Fenofibrate – 1-3 67mg tablets QD (half life 20hrs) » Taken with food - ↑ absorption » Max reduction of VLDL is achieved within 34 weeks of treatment – Adverse Effects » Rashes » GI disturbances (nausea, abdominal pain, diarrhea) • Fibrates - Adverse Effects – Gallstones (upper abdominal discomfort) » Gemfibrozil ↑ biliary cholesterol saturation » Use with caution in pts with biliary tract ds, women, obese pts, and Native Americans – Myopathy (muscle injury) » Tenderness, weakness, or unusual muscle pain » Will increase risk of statin-induced myopathy when used together (rhabdomyolysis has occurred rarely) • Fibrates - Adverse Effects –Hepatoxicity –Arrythmias –Hypokalemia –Displaces warfarin from plasma albumin since drug is highly protein bound. Need to ↓ warfarin dose • Bile Acid-Binding Resins (colestipol [Colestid®] and cholestyramine [Questran®]) – Will ↓ LDL, may ↑ VLDL (would require niacin if ↑ TG prior to tx) – MOA » Bile acids, the metabolites of cholesterol, are normally reabsorbed in the jejunum and ileum. When resins are given, they bind to bile acids in the intestinal lumen, prevent their reabsorption and increase their excretion. • Bile Acid-Binding Resins – MOA » ↑ excretion creates a demand for ↑ synthesis of bile acid. Liver cells must have an ↑ cholesterol supply (provided by LDL) to synthesize bile acid. Liver cells will ↑ their LDL receptors, ↑ing uptake of LDL from plasma. – Indication » Used alone to ↓ LDL (by 15-20%) » Normally used as adjuncts to the statins to ↓ LDL (by 50%) • Bile Acid-Binding Resins – Indication » Can be used to relieve pruritis in pts who have cholestasis » Dispensed in powder form (must be mixed with fluid). – Adverse Effects » Must be taken with meals » Constipation, bloating, indigestion, nausea » Large doses may impair absorption of fats or fat soluble vitamins (A, D, E, and K) • HMG CoA Reductase Inhibitors (“statins”) (lovastatin [Mevacor®], fluvastatin [Lescol®], pravastatin [Pravachol®], simvastatin [Zocor®], atorvastatin [Lipitor ®], cerivastatin [Baycol ®]) –Most Effective for ↓ LDL –moderately ↑ HDL and ↓ VLDL –Fewest adverse effects and tolerated best Acetyl-CoA, 乙酰辅酶A Acetoacetyl-CoA 乙酰乙酰辅酶A Statins,他汀类 HMG-CoA Reductase HMG-CoA MVA, 甲羟戊酸 Squalene, 鲨烯 Cholesterol, 胆固醇 de novo synthesis pathway of Cholesterol , 胆固醇从头合成 • “Statins” – MOA » Inhibits hepatic HMG CoA reductase » Inhibition of cholesterol synthesis causes hepatocytes to synthesize more LDL receptors » Hepatocytes are able to remove more LDLs from the blood » Decrease production of apolipoprotein B100, thereby ↓ production of VLDL » ↓ plaque cholesterol content • “Statins” – MOA » ↓ inflammation at the plaque site » Improve abnormal endothelial function » Enhance the ability of blood vessels to dilate » ↓ risk of thrombosis (inhibits platelet aggregation and blocks thrombin synthesis) » Statins have high first pass extraction by liver (only a small fraction of each dose reaches the general circulation) • (“Statins”) – Indications alone to ↓ LDL Used with bile acid – binding resins to ↓ LDL Used with niacin to ↓ LDL, ↓ VLDL, and ↑ HDL Enhanced if taken with food (except for pravastatin – taken without food) Used • “Statins” – Indications – Atorvastatin is most efficacious agent for use in severe hypercholesterolemia – High potency (>40-50% LDL lowering) – atorvastatin, simvastatin, cerivastatin – Low potency (20-40% LDL lowering) – lovastatin, fluvastatin, pravastatin – ↓ LDL within 2 weeks; max reduction in 4-6 weeks • “statins” – Adverse Effects –Since LDL cholesterol levels will return to pretreatment values if drugs are withdrawn, treatment must continue lifelong –Statins are pregnancy category X –Headache, rash, GI disturbances (dyspepsia, cramps, flatulence, constipation, abdominal pain) • “Statins” – Adverse Effects – Hepatotoxicity » Discontinue medication(D/C med) if aminotransferase activity is elevated more than 3X the upper normal limit » Check LFTs at baseline, 6 wks, 12 wks, then every 6 months – Myopathy (0.5% of pts) » Risk highest with lovastatin and especially in combination with Fibrates Antioxidant ---probucol • Pharmacological effects: to lower TC, LDL-C and HDL • MECHANISM: to inhibit the oxidative modification of LDL via the combination with lipoprotein for its hyper-lipophilic property Vit E, C - antioxidant Endothelium protective drugs • Drugs: polysaccharide sulfate • Mechanisms of action: to prevent the conglutination of white cell and platelet to inhibit the proliferation of vascular smooth muscle Polyunsaturated fatty acids---fish oil • EPA and DHA to decrease TG, VLDL,LDL-C to increase HDL-C • Potentially important effects: Inhibition of platelet function Prolongation of bleeding time Decrease of blood mucosity Prevention of atherosclerosis Summary Medications for Hyperlipidemia Drug Class Agents Effects (% change) Side Effects HMG CoA reductase inhibitors Lovastatin Pravastatin LDL (18-55), HDL (5-15) Triglycerides (7-30) Myopathy, increased liver enzymes Cholesterol absorption inhibitor Ezetimibe LDL( 14-18), HDL (1-3) Triglyceride (2) Headache, GI distress LDL (15-30), HDL (15-35) Triglyceride (20-50) Nicotinic Acid Flushing, Hyperglycemia, Hyperuricemia, GI distress, hepatotoxicity Fibric Acids Gemfibrozil Fenofibrate LDL (5-20), HDL (10-20) Triglyceride (20-50) Dyspepsia, gallstones, myopathy Bile Acid sequestrants Cholestyramine LDL HDL No change in triglycerides GI distress, constipation, decreased absorption of other drugs TCM Tx for AS • Folium Ginkgo 银杏叶 • Radix Salviae Miltiorrhizae 丹参 • Gynostemma pentaphyllum 绞股兰/七叶胆