* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download PPT - The Citadel
Compounding wikipedia , lookup
Pharmaceutical marketing wikipedia , lookup
Drug design wikipedia , lookup
Orphan drug wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmacognosy wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Drug interaction wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Effects of long-term benzodiazepine use wikipedia , lookup
Prescription costs wikipedia , lookup
Neuropharmacology wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
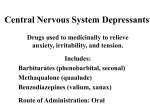
Chapter 7 Depressants and Inhalants Depressants These drugs all have a widespread effect in the brain that can be summed up as decreased CNS activity. Why are CNS depressants problematic? Usually prescribed under physician direction Second most frequently abused prescription drug and sometimes contributes to death due to accidental overdoses Can cause very alarming and dangerous behavior if not closely monitored Most problems associated with these drugs due to inadequate professional supervision Depressants As a group, also called sedativehypnotics Sedatives treat anxiety (current examples of popular sedatives include Xanax and Ativan) Hypnotics treat insomnia (sleeping pills: Ambien and Lunesta) Widely used depressants include: Alcohol Benzodiazepines (prescription) - Benzodiazepines possess sedative, hypnotic, anxiolytic, anticonvulsant, muscle relaxant, and amnesic actions, which are useful in a variety of indications such as alcohol dependence, seizures, anxiety, panic, agitation and insomnia. (source) DISCUSSION In your small group, discuss why you think physicians may be careless when prescribing depressants for patients suffering from anxiety. Discuss what you believe are the dangers of this practice and what other alternate therapies may exist History: Before Barbiturates Chloral hydrate Synthesized in 1832 - It was discovered through the chlorination of ethanol in 1832; chloral hydrate was not used clinically until about 1870. In the early 1900s a Chicago bartender named Mickey Finn became briefly famous when he was prosecuted for adding chloral hydrate to the drinks of some of his customers, after which they would become incapacitated and be robbed by one of his “ house girls.” The term “ Mickey Finn” entered our language as slang for a drug added to someone’s drink without his knowledge. Chloral hydrate is rapidly metabolized to trichloroethanol, which is the active hypnotic agent. When taken orally, chloral hydrate has a short onset period ( 30 minutes), and one to two grams will induce sleep in less than an hour. History: Before Barbiturates Paraldehyde Synthesized in 1829; used clinically in 1882 Effective with a wide safety margin and was soon found to be an effective anticonvulsant, hypnotic and sedative Today, paraldehyde is sometimes used to treat status epilepticus. Unlike diazepam and other benzodiazepines, it does not suppress breathing at therapeutic doses and so is safer when no resuscitation facilities exist or when the patient's breathing is already compromised. Paraldehyde has an extremely noxious taste and an odor that permeates the breath of the user. History: Before Barbiturates Bromides Widely used as a sleep agent in patent medicines Bromides accumulate in the body, and the depression they cause builds up over several days of regular use. Serious toxic effects follow repeated hypnotic doses of these agents. Bromides remained in OTC drugs through the 1960s In the early 1900’s, bromides were replaced by Barbiturates. Barbiturates Background First introduced in 1903, the barbiturates became so important that eventually over 2,500 different examples of this chemical class were synthesized Examples of once-popular barbiturates include phenobarbital, amobarbital, and secobarbital. Barbiturates are grouped according to time of onset and their duration of action (See Table 7.1, next slide). The short- acting barbiturates begin to produce effects in as little as 15 minutes, and have effects lasting only 2 or 3 hours, whereas the long- acting drugs may take an hour to produce effects, but they may last for 8 hours or more. BARBITURATES Grouped based on the time of onset and duration of activity Short-acting and rapid onset: used to induce sleep and often prescribed in high doses Long-acting and delayed onset: used to reduce anxiety and often prescribed in low doses See written description of grouping examples on next slide… Examples of Barbiturates Short-acting Intermediate-acting Pentobarbital, Secobarbital Time of onset: 15 minutes Duration of action: 2 to 3 hours Amobarbital, Butabarbital Time of onset: 30 minutes Duration of action: 5 to 6 hours Long-acting Mephobarbital, Phenobarbital Time of onset: 1 hour Duration of action: 8 hours or longer Concerns About Barbiturates Overdose Deaths Abuse and dependence Intentional and accidental the cause of death is typically respiratory depression (breathing slows and eventually stops) and in a great many cases this is due to the combined effects of alcohol and a depressant drug. Reinforcing effects of a drug are related to the rapidity of onset of effects Short-acting drugs are more likely to lead to psychological dependence Physical dependence ( withdrawal symptoms) are more likely to occur when a drug leaves the body quickly Concerns led to search for safer medications concerns about overdoses, psychological dependence, and physical dependence led to a search for safer CNS depressants Meprobamate Meprobamate ( Milltown) was patented in 1952 psychological dependence, and physical de-pendence led to a bad reputation for all bar-bituratesWidely prescribed beginning in the 1950s Used as an anxiolytic Like barbiturates, can produce psychological and physical dependence Still available as a prescription drug Meprobamate Meprobamate ( Milltown) was patented in 1952, the FDA approved its use in 1955. like the other barbiturates, produced both psychological and physical dependence In 1970, meprobamate became a Schedule IV controlled substance, and although it is still available for prescriptions under several brand names, the benzodiazepines have largely replaced it. Methaqualone Other names: Brand = Quaalude or Sopor Slang = “ludes” or “sopors” Despite problems in other countries, drug was introduced in the U.S. (1965) Package insert read “Addiction potential not established” Physicians overprescribed, thinking the drug was a safe alternative to barbiturates Widely misused and abused - Physicians were overprescribing a hypnotic drug that they believed to be safer than the barbiturates. Scheduling history: 1973: Schedule II 1985: Schedule I Benzodiazepines First introduced in 1960: The first of the benzodiazepines was chlordiazepoxide, which was marketed under the trade name Librium ( possibly because it “ liberates” one from anxieties). Reduces anxiety without inducing sleep Chlordiazepoxide enabled the treatment of emotional disturbances without a loss of mental acuity or alertness Much larger safety margin than barbiturates Physical dependence and overdose was rare (only when combined with other depressants like alcohol) Diazepam (Valium) became the best seller among all prescription drugs Benzodiazepines As these drugs became widely used, reports again appeared of psychological dependence, occasional physical dependence, and over-dose deaths. Dose level and time course are critical factors Overdose deaths more likely for drugs sold in higher doses Psychological dependence more likely with drugs that have a rapid onset of effects Physical dependence more likely with drugs that have a short duration of action - one way to reduce the severity of withdrawal symptoms is to reduce the dose of a drug slowly over time. Are benzodiazepines safer than barbiturates? More differences among drugs within each class Benzodiazepines: Rohypnol A 1990s version of a “Mickey Finn” Rohypnol ( flunitrazepam), a benzodiazepine sold as a hypnotic in many countries around the world but not in the United States, hit the news when reports surfaced of its being put into the drinks of unsuspecting women by their dates. Produces profound intoxication when mixed with alcohol during which the woman would be highly suggestible and unable to remember what had happened to her. Reportedly used as a “date-rape” drug Slipped into drinks 1997 change in the formulation causes a distinctive color when dissolved in a drink Nonbenzodiazepine Hypnotics The most recent additions to the class of depressant drugs do not have the chemical structure of the benzodiazepines, but they have similar effects. “Z-drugs” (Zopiclone) Similar to benzodiazepines but with a different chemical structure Zolpidem (Ambien) became the most widely prescribed hypnotic Short duration Rapid onset Nonbenzodiazepine Hypnotics “Z-drugs” Although many initially hoped that the nonbenzodiazepines would be more specific and avoid some of the problems of earlier drugs, there have been reports of withdrawal reactions and other complications with them as well. They are listed, along with the benzodiazepines, in Schedule IV, one step below the Schedule III classification of the barbiturates. Mechanism of Action Benzodiazepines and barbiturates Bind with receptors on GABA receptor complex Separate binding site for barbiturates and benzodiazepines Enhances the normally inhibitory effects of GABA Nonbenzodiazepine hypnotics Drug companies quickly began developing new drugs based on their ability to bind to these sites, leading to the development of the entire class of nonbenzodiazepine hypnotics. Thus the nonbenzodiazepine hypnotics were an entirely new class of drugs designed to selectively bind to different sites on the GABA receptor complex Beneficial Uses As Anxiolytics Sedatives often prescribed to reduce anxiety Most physicians used to accept the widely held view that various types of dysfunctional behavior ( e.g., phobias, panic attacks, obsessivecompulsive disorders psychosomatic problems) result from various forms of psychological stress that can be lumped under the general classification of “ anxieties.” Four benzodiazepines are among the top 100 most commonly prescribed medications in the United States Xanax Ativan Klonopin Valium Concerns: Anxiolytics Sedatives are not appropriate for all anxiety disorders Example: For specific phobias ( e.g., fear of spiders), behavior therapy is a more effective treatment. And for obsessivecompulsive disorder and most of the official “anxiety disorders”, certain antidepressant drugs seem to be most effective. Overprescribed… Most sedatives are not prescribed by psychiatrists Most patients do not have a clearly defined anxiety disorder or physical ailment, and in any individual case it may be impossible to know whether the patient just enjoys getting a “ feel- good pill” or feels better because of a specific antianxiety effect. Beneficial Uses As hypnotics Insomnia is the term used to include several symptoms: trouble falling asleep, trouble staying asleep, or waking up too early. Sedatives (at large enough doses) decrease sleep onset time - This is essentially the principle on which hypnotic drug therapy is based: a large enough dose is taken to help you get to sleep more quickly. About a third of American adults report trouble sleeping - most people who are concerned about insomnia do not take prescription hypnotic drugs, and there are effective nonmedical ways of dealing with insomnia ( see Targeting Prevention Box, p157). Concerns: Hypnotics Concerns about the nonbenzodiazepine hypnotics include: Sleepwalking Sleep-eating Driving while in a semi-waking state These concerns led the FDA to investigate such reports, and in 2008 all hypnotic drugs were required to attach a warning label about sleep- driving and other dangerous behaviors that might occur after taking these drugs. If you or someone you know has trouble sleeping, before resorting to the use of medication it would be wise to follow the suggestions given in the Targeting Prevention Box. These tactics will probably help most people deal with sleeplessness. Beneficial Uses As anticonvulsants Barbiturates and benzodiazepines may be prescribed for seizure disorders (epilepsies) They are effective in reasonably low doses and are often combined with other anticonvulsant drugs for even better effectiveness. Potential concerns Tolerance can make it difficult to find a dose that is effective but doesn’t cause excessive drowsiness Abrupt withdrawal is likely to cause seizures so medication changes should be done carefully. Causes for Concern – Dependence Liability Psychological dependence Especially associated with short-acting sedatives: Animals given the opportunity to press a lever that delivers intravenous barbiturates will do so, and the short- acting barbiturates work best for this. Animals will also self- inject several of the benzodiazepines, but at lower rates than with the shortacting barbiturates. Experiments in humans yielded similar results These experiments indicate that these sedative drugs can serve as reinforcers of behavior but that the short- acting barbiturates are probably more likely to lead to dependence than are any of the benzodiazepines currently on the market. Causes for Concern – Dependence Liability Physical dependence Withdrawal syndrome is similar to alcohol and potentially life-threatening Barbiturate withdrawal symptoms: anxiety, insomnia, tremulousness, weakness, nausea and vomiting, seizures, disorientation, agitation, delusions, and visual and auditory hallucinations Benzodiazepine withdrawal is similar but less severe Because there is a cross- dependence among the barbiturates, the benzodiazepines, and alcohol, it is theoretically possible to use any of these drugs to halt the withdrawal symptoms from any other depressant. Drug treatment is often used, and a general rule is to use a long-acting drug, given in divided Causes for Concern – Acute Toxicity Behavioral Behaviorally, all these drugs are capable of producing alcohol- like intoxication with impaired judgment and incoordination. Additive effects if combined with alcohol so that the danger is further increased. Physiological Respiratory depression Especially dangerous if combined with alcohol In the coroners’ reports, in almost every case the culprit is the drug in combination with alcohol or another drug, rather than the benzodiazepine alone Causes for Concern – Patterns of Abuse Almost all of the abuse of the sedative- hypnotic agents has historically involved the oral use of legally manufactured products. Two types of typical abusers: 1) Older adults using prescription drugs who develop tolerance and increase their dosage Even though some of these individuals visit several physicians to obtain prescriptions for enough pills to maintain this level of use, many would vehemently deny that they are “ drug abusers.” This type of chronic use can lead to physical dependence. Causes for Concern – Patterns of Abuse Two types of typical abusers: 2) The other major group tends to be younger and consists of people who obtain the drugs simply to get high. These younger abusers tend to take relatively large doses, to mix several drugs, or to drink alcohol with the drug, all for the purpose of becoming intoxicated. With this type of use, the possibility of acute toxicity is particularly high. Inhalants Examples of products that contain inhalable solvents gasoline, glue, paint, lighter fluid, spray cans, nail polish, correction fluid when inhaled, can have effects that are similar in an overall way to the depressants. High-dose exposure to these fumes makes users intoxicated, often slurring their speech and causing them to have trouble walking a straight line, as if they were drunk on alcohol. similar to alcohol and other depressants Examples of InhalantsSee Table 7.3, next slide Gaseous Anesthetics Nitrites Nitrous oxide, ether Current and former medical anesthetics Isoamyl, isobutyl “Locker room,” “Rush,” “poppers” Volatile solvents Petroleum, acetone, toluene Paint, paint thinner and remover, nail polish remover, correction fluid, glues TABLE 7.3 - SOME CHEMICALS ABUSED BY INHALATION Gaseous Anesthetics One of the oldest, nitrous oxide, was first used in the early 1800s and quite early acquired the popular name “ laughing gas” because of the hilarity exhibited by some of its users. Nitrous oxide is still used for light anesthesia, especially by dentists. It is also often used in combination with one of the more effective inhaled anesthetics, allowing the use of a lower concentration Used as a propellant for commercial and home whipping-cream dispensers and is abused by recreational users Nitrites Amyl nitrite was first introduced into medicine in the mid- 1800s as a treatment for chest pain. Inhaling the vapors of this drug relaxes blood vessels, including the coronary arteries. Causes systemic vasodilation Reduces blood pressure, pre-syncope Used to treat cyanide poisoning In addition to amyl nitrite, butyl, isopropyl, and isobutyl nitrite produce similar effects. These products have been used in various cleaning products, and some users have inhaled those products to achieve the same effect. Volatile Solvents The modern era of solvent abuse can be traced back to 1959 investigative article News articles and education programs demonstrated how to abuse volatile solvents (see text p. 161-162) Use may have spread due to increased publicity In general, abuse tends to occur as localized fads Most users are very young 8% of 8th-graders reported past year use 3.6% of 12th-graders reported past year use Dangers of Inhaling Solvents Several solvents have been linked to: Kidney damage Brain damage Peripheral nerve damage Irritation of the respiratory tract Severe headache Death by suffocation Laws to limit sales of these household solvents to minors or to make it illegal to use them to become intoxicated have been passed in some areas, but typically they have little effect. Too many products are simply too readily available. Gamma Hydroxybutyric Acid GHB Gamma hydroxybutyrate (GHB) occurs naturally in the brain as well as in other parts of the body. Its structure is fairly close to the inhibitory neurotransmitter GABA. GHB has been known for some time to be a CNS depressant, and has been used in other countries as an anesthetic. Structurally similar to the inhibitory neurotransmitter GABA Is a CNS depressant Taking larger quantities of GHB alone, or combining GHB with alcohol, produces a combined depressant effect similar to what would be produced by combining alcohol with any of the other depressants In 2000, Congress directed that GHB be placed on Schedule I. Except for one formulation (Xyrem) Reduces frequency of cataplexy (affects roughly 70% of people who have narcolepsy) End of presentation