* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 2nd T. 4th L. Updated
Environmental impact of pharmaceuticals and personal care products wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Neuropharmacology wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacognosy wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Drug interaction wikipedia , lookup
Psychopharmacology wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
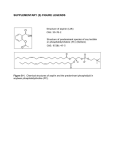
Pharmacology-1 PHL 211 2nd Term 4th Lecture By Abdelkader Ashour, Ph.D. Phone: 4677212 Email: [email protected] Chemistry & Pharmacokinetics of NSAIDs Although there are many differences in the kinetics of NSAIDs, they have some general properties in common. All but one of the NSAIDs are weak organic acids the exception, nabumetone, is a ketone prodrug that is metabolized to the acidic active drug Most of NSAIDs are well absorbed, and food does not substantially change their bioavailability Most of the NSAIDs are highly metabolized, some by phase I followed by phase II mechanisms and others by direct glucuronidation (phase II) alone NSAID metabolism proceeds, in large part, by way of the CYP3A or CYP2C families of P450 enzymes in the liver While renal excretion is the most important route for final elimination, nearly all undergo varying degrees of biliary excretion and reabsorption (enterohepatic circulation) Most of the NSAIDs are highly protein-bound (~ 98%), usually to albumin Adverse Effects of NSAID Therapy Because PGs are involved in gastric cytoprotection, platelet aggregation, renal vascular autoregulation and induction of labour, NSAIDs share, to some extent, a similar profile of mechanism-dependent side effects which include: I. Gastrointestinal Disturbances: Adverse GI events are the commonest unwanted effects of the NSAIDs These side effects result mainly from inhibition of gastric COX-1, which is responsible for the synthesis of the PGI2 and PGE2 that normally inhibit acid secretion and protect the mucosa by enhancing mucosal blood flow and secretion of cytoprotective mucus The damage is seen whether NSAIDs are given orally or systemically In some cases local damage to the gastric mucosa caused directly by the drug itself (e.g., aspirin) may compound the damage Common GI side effects include gastric discomfort, dyspepsia, nausea and vomiting, and in some cases gastric ulceration and bleeding The risk is further increased in those with Helicobacter pylori infection and the concurrent use of glucocorticoids Co-administration of the PGE1 analog misoprostol or proton pump inhibitors along with NSAIDs can be beneficial in the prevention of duodenal and gastric ulceration COX-2-selective inhibitors are associated with a decreased incidence of GI adverse events, however, they increase the incidence of thrombosis and myocardial infarction These drugs depress PGI2 formation by endothelial cells without concomitant inhibition of platelet TXA2 (PGI2 restrains the cardiovascular effects of TXA2), (cf. low-dose aspirin!) Adverse Effects of NSAID Therapy II.Blood Pressure, Renal, and Renovascular Adverse Events: NSAIDs have been associated with renal and renovascular adverse events NSAIDs have little effect on renal function or blood pressure in normal human subjects However, in patients with congestive heart failure, hepatic cirrhosis, chronic kidney disease, hypovolemia, and other states of activation of the sympathoadrenal or renin-angiotensin systems, PG formation becomes crucial PGI2 and PGE2 inhibit both the re-absorption of Cl- and the action of anti-diuretic hormone NSAIDs inhibition of synthesis of these prostanoids may lead to the retention of salt and water Hypertensive complications are suggested to occur more commonly in patients treated with COX-2 inhibitors than with tNSAIDs Analgesic Nephropathy. This is a condition of slowly progressive renal failure, decreased concentrating capacity of the renal tubule, and sterile pyuria Risk factors are the chronic use of high doses of combinations of NSAIDs and frequent urinary tract infections If recognized early, discontinuation of NSAIDs permits recovery of renal function III.Other, much less common, unwanted effects of NSAIDs include: All NSAIDs (except COX-2 inhibitors) prevent platelet aggregation and therefore may prolong bleeding. Aspirin is the main problem in this regard Liver disorders, which is more likely if there is already renal impairment Some Important NSAIDs Aspirin: Aspirin (acetylsalicylic acid, ASA) was among the earliest drugs synthesised, and is still one of the most commonly consumed drugs worldwide Sodium salicylate and aspirin are equally effective anti-inflammatory drugs, though aspirin may be more effective as an analgesic Mode of action. Aspirin is unique among NSAIDs in that it irreversibly inhibits COX by acylating the active site of the enzyme, so preventing the formation of products including thromboxane, prostacyclin and other PGs, until more COX is synthesised Aspirin irreversibly inhibits platelet COX, so that aspirin's antiplatelet effect lasts 8-10 days (the life of the platelet) Aspirin, being a weak acid, is protonated in the acid environment of the stomach, thus facilitating its passage across the mucosa. Most absorption, however, occurs in the ileum, because of the extensive surface area of the microvilli Aspirin is rapidly hydrolysed by esterases in the plasma and the tissues, yielding salicylate. Salicylate also has an anti-inflammatory action but additionally exerts important effects on respiration and it is highly irritant to the stomach. Aspirin inhibits platelet aggregation, while salicylates do not Alkalinization of the urine increases the rate of excretion of free salicylate and its water-soluble conjugates Aspirin Clinical Uses of aspirin: A. Analgesia, Antipyresis, & Anti-inflammatory Effects: 1. Aspirin is employed for mild to moderate pain of varied origin but is not effective for severe visceral pain 2. Aspirin and other NSAIDs have been combined with opioid analgesics for treatment of cancer pain, where their anti-inflammatory effects act synergistically with the opioids to enhance analgesia 3. High-dose salicylates are effective for treatment of rheumatic fever, rheumatoid arthritis, and other inflammatory joint conditions B. Other Effects: Aspirin decreases the incidence of transient ischemic attacks, unstable angina, coronary artery thrombosis with myocardial infarction, and thrombosis after coronary artery bypass grafting Epidemiologic studies suggest that long-term use of aspirin at low dosage is associated with a lower incidence of colon cancer, possibly related to its COXinhibiting effects Aspirin C. Aspirin in dentistry Aspirin has been used in dentistry as an anti-inflammatory, analgesic and antipyretic drug prescribed for use within short periods Clinical trials have shown repeatedly that aspirin is effective in the management of dental pain Tissue damage resulting from pulpits, periodontitis, or oral surgery induce the production of COX-2, which, in turn, leads to the synthesis of the PGs that sensitize pain fibers and promote inflammation Traditional NSAIDs, such as aspirin, act by blocking both COX-1 and COX-2. Aspirin, like all the other NSAIDs, induce inhibition of thromboxane synthesis resulting in a decrease in the platelet aggregation For most NSAIDs this effect is reversible within 24 hours; however, aspirin is unique in that it irreversibly damages COX for the life of the platelet Although an increase in the time of coagulation can be accepted in normal patients, aspirin might promote post-operative hemorrhage, mainly if the clot is not totally formed Aspirin Adverse Effects: 1. It irritates the gastric mucosa (direct acid effect and inhibition of cytoprotective PG synthesis). This may cause gastric and duodenal ulcers 2. It can precipitate bronchoconstriction (“aspirin asthma,” pseudoallergy) due to inhibition of PGE2 synthesis and overproduction of leukotrienes 3. Hepatotoxicity and renal toxicity occur less frequently 4. With higher doses, patients may experience salicylism (vomiting, tinnitus, decreased hearing, and vertigo) reversible by reducing the dosage 5. Still larger doses of salicylates cause hyperpnea through a direct effect on the medulla. At toxic salicylate levels, respiratory alkalosis followed by metabolic acidosis (salicylate accumulation) & respiratory depression can occur Salicylate poisoning is a medical emergency; it is more common, and more serious, in children than in adults 6. Caution is needed in children and juveniles because of Reye’s syndrome. The latter has been observed in association with febrile viral infections and ingestion of ASA; its prognosis is poor (liver and brain damage). 7. Because aspirin inhibits platelet aggregation and prolongs bleeding time, it should not be used in patients with impaired blood coagulability 8. Administration of ASA at the end of pregnancy may result in prolonged labor, bleeding tendency in mother and infant, and premature closure of the ductus arteriosus Aspirin Some important interactions with other drugs : 1. The plasma concentration of salicylates generally is little affected by other drugs, but concurrent administration of aspirin lowers the concentrations of indomethacin, naproxen, ketoprofen, and fenoprofen, at least in part by displacement from plasma proteins 2. Aspirin causes a potentially hazardous increase in the effect of warfarin, partly by displacing it from plasma proteins and partly because its effect on platelets interferes with haemostatic mechanisms. 3. Aspirin also interferes with the effect of uricosuric agents such as probenecid and sulfinpyrazone , and because low doses of aspirin may, on their own, reduce urate excretion, aspirin should not be used in gout 4. Antagonism of spironolactone-induced natriuresis