* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 10-2014 NSAIDsnew
Discovery and development of proton pump inhibitors wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Drug interaction wikipedia , lookup
Hyaluronic acid wikipedia , lookup
Psychopharmacology wikipedia , lookup
Neuropharmacology wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
Local hormones and immune reaction
+Antinflamatory drugs
1
Definition of the drugs & their categories
2 The inflammatory response & inhibition
3
side effects
A therapeutic agent which relieves pain and
fever by inhibiting the inflammatory response.
These drugs are available over the counter and
by prescription.
Some common examples include aspirin,
ibuprofen, Celebrex, and less commonly
acetaminophen (Tylenol).
The body’s response to a stimuli which causes pain
and/or tissue damage.
Physiologically capillaries become “leaky” through
vasodilation.
The response is initiated by the chemical
messengers prostaglandins.
Redness - due to local vessel dilatation
Heat - due to local vessel dilatation
Swelling – due to influx of plasma proteins and
phagocyte cells into the tissue spaces
Pain – due to local release of enzymes and increased
tissue pressure
occurs in vascularised tissues in response to injury.
It is part of the innate nonspecific immune response.
Inflammatory responses require activation of
leukocytes: neutrophils, eosinophils, basophils,
mast cells, monocytes, and lymphocytes, although not all cell
types need be involved in an inflammatory episode.
The cells migrate to the area of tissue damage from the
systemic circulation and become activated.
Diseases with a chronic inflammatory component
Inflammatory disease
Inflammatory cell infiltrate
Acute respiratory distress
syndrome
Bronchial asthma
Neutrophil
Eosinophil,T cell, monocyte,
basophil
T cell, monocyte
Atherosclerosis
Monocyte,T cell, neutrophil
Glomerulonephritis
Inflammatory bowel disease Monocyte, neutrophil,T cell,
eosinophil
Monocyte, neutrophil
Osteoarthritis
T cell, neutrophil
Psoriasis
Monocyte, neutrophil
Rheumatoid arthritis
T cell, monocyte
Sarcoidosis
FUNCTION OF MEDIATORS IN INFLAMMATION
Inflammatory mediators
Activated leukocytes at a site of inflammation release
compounds which enhance the inflammatory response
mainly cytokines and eicosanoids (arachidonic acid
metabolites). But the complexity of the response
many mediators:
is indicated by the range of
complement products, kinins (bradykinin)
and the contact system (coagulation factors XI and
XII, pre-kallikrein, high molecular weight kininogen);
nitric oxide and vasoactive amines (histamine,
serotonin and adenosine); activated forms of oxygen;
platelet activating factor (PAF); metalloproteinases
(collagenases, gelatinases, and proteoglycanase), etc.
PROSTANOIDS (PGs & Txs)
PGI2 (prostacyclin)
is located predominantly in vascular
endothelium.
Main effects:
•vasodilatation
•inhibition of platelet aggregation
TxA2 is found in the platelets.
Main effects:
•platelet aggregation
•vasoconstriction
PGE2 causes:
• inhibition of gastric acid secretion
•contraction of pregnant uterus
•contraction of GI smooth muscles
PGF2α – main effects:
•contraction of bronchi
•contraction of myometrium
Cytokines (ILs, TNFs, IFNs, CSFs, etc.)
are peptides regulating cell growth,
differentiation, and activation, and some have
therapeutic value:
• IL-1 plays a part in the sepsis syndrome
and rheumatoid arthritis, and successful
blockade of its receptor offers a
therapeutic approach for these conditions.
• TNFα is similar to IL-1. Agents that block him,
e.g. etanercept, infliximab are finding their place
among Disease modifying antirheumatic drugs.
Prostaglandins were isolated from human semen in
1936 by Ulf von Euler. He named them
Prostaglandins because he believed they came
from the prostate gland.
The Swedish scientist received the Nobel Prize in
medicine in 1970 for this work.
Since his work in this area it has been determined
that they exist and are synthesized in almost every
cell of the body.
They are synthesized in the same cell on which
they act.
The goal is to inhibit the biosynthesis of
prostaglandins in order to relieve the symptoms
caused by the inflammatory response.
Prostaglandins are synthesized from arachidonic
acid in a pathway mediated by the Cyclooxygenase
enzymes.
PATHOLOGIC
FEVER
ASTHMA
ULCERS
DIARRHEA
DYSMENORRHEA
INFLAMMATION
BONE EROSION
PAIN
PHYSIOLOGIC
TEMPERATURE CONTROL
BRONCHIAL TONE
CYTOPROTECTION
INTESTINAL MOBILITY
MYOMETRIAL TONE
SEMEN VIABILITY
COX-1: beneficial
COX-2: harmful
Peripheral injury site
Inflammation
Brain
Modulate pain
perception
Promote fever
(hypothalamus)
Stomach
protect mucosa
Platelets
aggregation
Kidney
vasodilation
COX
Expression
Function
Inhibitors
COX-1
organ pain, platelet
constitutively
function, stomach
throughout the body
protection
COX-2
Inducible: inflammation, NSAIDs, COX 2
Inducible and
pain, fever
inhibitors including
constitutively in brain, Constitutive: synaptic celecoxib
kidney
plasticity
(Celobrex )
COX-3
Constitutively, high in pain pathways, not
acetaminophen
inflammation pathways some NSAIDs
brain, heart
NSAIDs including
aspirin
There are two major categories for non-steroidal
anti-inflammatory drugs
The first is non-selective anti-inflammatory drugs.
The second is selective anti-inflammatory drugs,
COX-2 inhibitors.
NSAIDs block the COX enzymes , reduce
prostaglandins, inflammation, pain, and fever are
reduced.
COX-1 produced prostaglandins that support platelets
and protect the stomach.
Reduced prostaglandins that protect the stomach and
support blood clotting, so NSAIDs can cause ulcers in
the stomach and promote bleeding.
three major pharmacologically desirable actions,
stemming from the suppression of prostanoid synthesis
in inflammatory cells through inhibition of the cyclooxygenase (COX)-2 isoform of the arachidonic acid
COX. They are as follow.
An anti-inflammatory action: the decrease in prostaglandin E2
and prostacyclin reduces vasodilatation and, indirectly,
oedema. Accumulation of inflammatory cells is not reduced.
An analgesic effect: decreased prostaglandin generation means
less sensitisation of nociceptive nerve endings to inflammatory
mediators such as bradykinin and 5-hydroxytryptamine. Relief
of headache is probably a result of decreased prostaglandinmediated vasodilatation.
An antipyretic effect: interleukin-1 releases
prostaglandins in the central nervous system, where
they elevate the hypothalamic set point for temperature
control, thus causing fever. NSAIDs prevent this. Some
important examples are aspirin , ibuprofen , naproxen ,
indometacin, piroxicam and paracetamol. Newer
agents with more selective inhibition of COX-2 (and
thus fewer adverse effects on the gastrointestinal tract)
include celecoxib and etoricoxib
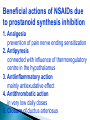
Beneficial actions of NSAIDs due
to prostanoid synthesis inhibition
1. Analgesia
prevention of pain nerve ending sensitization
2. Antipyresis
connected with influence of thermoregulatory
centre in the hypothalamus
3. Antiinflammatory action
mainly antiexudative effect
4. Antithrombotic action
in very low daily doses
5. Closure of ductus arteriosus
INHIBITION OF
◦
◦
◦
◦
◦
◦
◦
◦
CYCLOOXYGENASE ENZYMES
LIPOXYGENASE ENZYMES
SUPEROXIDE GENERATION
LYSOSOMAL ENZYME RELEASE
NEUTROPHIL ACTIVITY
LYMPHOCYTE FUNCTION
CYTOKINE RELEASE
CARTILAGE METABOLISM
COX-1
Gastric ulcers
COX-2
Reduce inflammation
Bleeding
Reduce pain
Acute renal failure
Reduce fever
NSAIDs : anti-platelet—decreases ability of blood to clot
Due to inhibition of the constitutive housekeeping
enzyme cyclo-oxygenase (COX)-1 isoform of COX,
are common, particularly in the elderly, and include the
following.
Dyspepsia, nausea and vomiting. Gastric damage may
occur in chronic users, with risk of haemorrhage. The
cause is suppression of gastroprotective prostaglandins
in the gastric mucosa.
Skin reactions. Mechanism unknown.
Reversible renal insufficiency. Seen mainly in
individuals with compromised renal function when the
compensatory prostaglandin E2-mediated vasodilatation
is inhibited.
'Analgesic-associated nephropathy'. This can occur
following long-continued high doses of NSAIDs (e.g.
paracetamol) and is often irreversible.
Liver disorders, bone marrow depression. Relatively
uncommon.
Bronchospasm. Seen in 'aspirin-sensitive' asthmatics
For analgesia (e.g. headache, dysmenorrhea,
backache, bony metastases, postoperative
pain):
◦ short-term use: aspirin , paracetamol or
ibuprofen
◦ chronic pain: more potent, longer lasting
drugs (e.g. diflunisal , naproxen , piroxicam )
◦ to reduce the requirement for narcotic
analgesics (e.g. ketorolac postoperatively).
For anti-inflammatory effects (e.g. rheumatoid arthritis
and related connective tissue disorders, gout and soft
tissue disorders).
◦ Note that there is substantial individual variation in clinical
response to NSAIDs and considerable unpredictable patient
preference for one drug rather than another.
To lower temperature (antipyretic): paracetamol.
is the oldest non-steroidal anti-inflammatory drug. It acts by
irreversibly inactivating both cyclo-oxygenase (COX)-1 and
COX-2.
In addition to its anti-inflammatory actions, aspirin inhibits
platelet aggregation, and its main clinical importance now is
in the therapy of myocardial infarction.
It is given orally and is rapidly absorbed; 75% is metabolised
in the liver.
Elimination follows first-order kinetics with low doses (halflife 4 hours), and saturation kinetics with high doses (half-life
over 15 hours).
Clinical Uses of Aspirin® (Bayer, 1899)
As analgesic (300 to 600 mg during 6 to 8 h) for headache, backache, toothache, neuralgias.
As antipyretic in fever of any origin in the same
doses as for analglesia.
Acute rheumatic fever.
Rheumatoid arthritis.
Aspirin a dose of 3 to 5 g/24 h after meal is effective in most
cases. Since large doses of Aspirin are poorly tolerated for a
long time, the new NSAIDs (diclofenac, ibuprofen, etc.) in depot
form are preferred.
Postmyocardial infarction and poststroke patients.
By inhibiting platelet aggregation in low doses (100 mg
daily) Aspirin decreases the incidence of re infarction.
Unwanted effects:
◦ with therapeutic doses: some gastric bleeding (usually slight
and asymptomatic) is common
◦ with large doses: dizziness, deafness and tinnitus ('salicylism');
compensated respiratory alkalosis may occur
◦ with toxic doses (e.g. from self-poisoning): uncompensated
respiratory acidosis with metabolic acidosis may occur,
particularly in children
◦ aspirin has been linked with a postviral encephalitis (Reye's
syndrome) in children.
Aspirin therapy in children with rheumatoid arthritis
has been found to raise serum concentration transaminases, indicating liver damage. Most cases are
asymptomatic but it is potentially dangerous.
If given concomitantly with warfarin, aspirin can
cause a potentially hazardous increase in the risk of
bleeding.
Seen in children under 15 after an acute viral illness
Results in encephalopathy, fatty infiltration of the liver, pancreas,
kidneys, spleen, and lymph nodes
Cause is unknown
An association between salicylate therapy and
“Reye’s syndrome”, a rare form of hepatic
encephalopathy seen in children, having viral infection
(varicella, influenza), has been noted.
Aspirin should not be given to children under 15
years unless specifically indicated, e.g. for juvenile
arthritis (paracetamol is preferred).
Aspirin-previously thought of as an old anti-inflammatory
workhorse-is now approaching the status of a wonder drug
that is of benefit not only in inflammation, but in an increasing
number of other conditions. These include:
cardiovascular disorders: through the antiplatelet action of
low-dose aspirin
colonic and rectal cancer: aspirin (and COX-2 inhibitors)
may reduce colorectal cancer-clinical trial results are awaited
Alzheimer's disease: again, clinical trial results are awaited
radiation-induced diarrhoea.
has potent analgesic and antipyretic actions
but rather weaker anti-inflammatory effects
than other NSAIDs. It may act through
inhibition of a CNS -specific (COX) isoform
such as COX-3, although this is not yet
conclusive.
It is given orally and metabolised in the liver
(half-life 2-4 hours).
Toxic doses cause nausea and vomiting, then, after
24-48 hours, potentially fatal liver damage by
saturating normal conjugating enzymes, causing
the drug to be converted by mixed function
oxidases to N-acetyl-p-benzoquinone imine. If not
inactivated by conjugation with glutathione, this
compound reacts with cell proteins and kills the
cell.
Agents that increase glutathione (I.V acetylcysteine
or oral methionine ) can prevent liver damage if
given early.
Nonselective COX-1/COX-2 inhibitors
DERIVATIVES OF ACIDS
Salicylates
Acetylsalicylic acid (Aspirin®, 1899), Diflunisal
Methyl salicylate (revulsive drug)
Phenylacetates: Acelcofenac, Diclofenac
Indolacetates: Indometacin, Sulindac
Enolates (oxicams)
Piroxicam, Piroxicam beta-cyclodextrin (prodrug),
Lornoxicam, Tenoxicam
Propionates
Flurbiprofen, Ibuprofen, Ketoprofen, Naproxen
OTHERS (with less application)
Pyrazolones: Phenazone, Propyphenazone, etc.
Pyrazolidinediones: Oxyphenbutazone, Phenylbutazone
Celecoxib (Celebrex), blocks COX-2 but little on
COX-1, classified as a selective COX-2 inhibitor ,cause
less bleeding and fewer ulcers.
Aspirin is a unique NSAID, the only NSAID inhibits
clotting of blood for a prolonged period (4 to 7 days),
ideal for preventing blood clots that cause heart attacks
and strokes
Most NSAIDs inhibit the clotting of blood for only a few
hours
Ketorolac (Keto) is a very potent NSAID and is used for
moderately severe acute pain that usually requires narcotics
Ketorolac (Keto) causes ulcers more frequently than other
NSAID. Therefore, it is not used for more than five days.
Individuals who do not respond to one NSAID may respond
to another.
Propionic acid derivatives such as ibuprofen,
ketoprofen (Orudis), naproxen and fenoprofen (Nalfon)
Acetic acid derivatives include indomethacin (Indocin),
sulindac (Clinoril) and tolmetin (Tolectin)---these drugs
have more severe adverse reactions than the proprionic
acid derivatives
Ibuprofen
is a derivative of phenylpropionic acid.
In doses of 2.4 g daily it is is equivalent to 4 g
of Aspirin in anti-inflammatory effect. Oral ibuprofen is
often prescribed in lower doses (< 2.4 g/d), at which
it has analgesic but not antiinflammatory efficacy.
It is available in low dose forms under several trade
names).
A topical cream preparation is absorbed into muscle.
A liquid gel preparation of ibuprofen provides
prompt relief in postsurgical dental pain. In comparison
with indometacin, ibuprofen decreases urine
output less and also causes less fluid retention. It is
effective in closing ductus arteriosus in preterm infants,
with much the same efficacy as indometacin.
IV indomethacin is approved for the tx of patent ductus
arteriosus in premature infants.
Remember: patent ductus is a communication between
the pulmonary artery and the aorta
Toradol (ketoralac) is used only for pain. Is the only
NSAID that can be given by injection. Use limited to 5
days as can cause bleeding.
Oxicam drugs include Mobic (meloxacam) and Feldene
(piroxicam)
Celebrex (celecoxib)
Affect bleeding only while drug is still in the system
Drug interactions with NSAIDs
Drugs
Diuretics
Beta-blockers
ACE inhibitors
Anticoagulants
Sulfonylurea
Cyclosporine
GCS
Alcohol
Result
Decrease diuresis
Decrease antihypertensive effect
Decrease antihypertensive effect
Increase of GI bleeding
Increase hypoglycemic risk
Increase nephrotoxicity
Increase of GI bleeding
Increase of GI bleeding
Cardiovascular
80% increase in AMI risk with newer COX-2
and high dose traditional NSAID
Heart failure risk
( with CHF history x10, without x2)
Gastrointestinal
Direct irritation : acidic molecules
Indirect irritation: inhibit COX-1, reduce protective
prostaglandins
S/S: nausea, vomiting, dyspepsia, gastric ulcer/bleeding,
diarrhea
Duration of therapy, dose
Renal
Decrease prostaglandins→ constriction of afferent
arteriole → decreased renal perfusion
→alter renal function
S/S: salt and fluid retension, hypertension
Caution: NSAID with ACE inhibitor, diuretic
Rare: ARF, ATN, nephrotic syn.
Others
Allergy: shortness of breath
Asthma : a higher risk for serious allergic reaction
with a serious allergy to one NSAID are likely to have
similar reaction to a different NSAID
photosensitivity
Not recommended during pregnancy, particular 3rd
trimester
Cause early closure of fetal ductus arteriosus,
and fetal renal toxicity, premature birth
Acetaminophen ia more safe during pregnancy
In France, NSAID and aspirin is contra-indicated after
6 months of pregnancy
Arthrotec (diclofenac/misoprostol)
Diclofenac (Voltaren® Meitifen,Formax ®)
Ketorolac (Toradol Keto, Painoff,Keto Inj,
Kop Inj )
Tolmetin (Tolectin ®)
Etodolac (Lodine ® Lonine )
Indomethacin (Indocin® Acemet )
Sulindac (Clinoril Unidac ®)
Diflunisal (Dolobid ®)
Salsalate (Disalcid ®)
Meloxicam ( Mobic ® Subic )
Piroxicam (Feldene Tonmax inj, Foglugen)
Tenoxicam ( Tencam, Sutondin )
Nabumetone (Relafen ® Relifex, No-ton )
Flurbiprofen (Ansaid ® Flufen,Lefenine, Flur Di
Fen )
Ketoprofen (Orudis ®) Ketoprofen inj
Oxaprozin (Daypro ® )
Ibuprofen (Motrin ® Purfen ,Mac Safe syr, Arfen
inj )
Naproxen (Naprosyn ® Napton)
Celecoxib (Celebrex ® )
Rofecoxib (Vioxx ® )
Valdecoxib (Bextra ® )