* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download INTRODUCTION TO SCIENTIFIC RESEARCH
Pharmaceutical marketing wikipedia , lookup
Specialty drugs in the United States wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Compounding wikipedia , lookup
Orphan drug wikipedia , lookup
Drug design wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmacognosy wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Psychopharmacology wikipedia , lookup
Neuropharmacology wikipedia , lookup
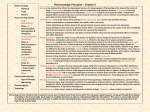
General Principles of Pharmacology Targets for drug action * A drug is a chemical that affects physiological function in specific way * Most drugs are effective because they bind to particular target protein including receptors TYPES OF RECEPTORS 2 TYPES OF RECEPTORS 1- Channel-linked receptors - coupled directly to an ion channel such acetylcholine, GABA & Glutamate receptors 2- G-protein-Coupled receptors - it produces second massenger as well as opening channel -stimulated by adrenergic drugs, muscarinic & hormones 3 Continue TYPES OF RECEPTORS 3- Kinase-linked receptors - insulin & growth hormone receptors - this type also linked to guanylate cyclase *** ALL PREVIOUS TYPES OF RECEPTORS ARE MEMBRANE BOUND 4- Receptors that regulate gene transcription * They are soluble receptor usualy inside the cell (cytosol or intranuclear protein) * Steroid , thyroid, retinoic acid & vit D 4 5 Drug Specificity * Drug binds only to certain targets * Individual targets recognise only certain class of drug * There rae no drugs completely specific in action * Increase the dose will affect other targets in cell 6 Binding of Drugs to Receptors * Binding of drugs to receptors obeys the law of mass action (the rate of chemical reaction is proportional to the product concentrations of reactants) *At equilibrium, receptor occupancy is related to drug concentration * The higher the affinity of drug for receptor, the lower the concentration needed for occupancy 7 Agonist & antagonist * drug acting on receptor may be agonist or antagonist A- Agonist initiates changes in cell function * Full agonist: has high efficacy * Partial agonist - it produces submaximal effects - it has intermediate efficacy What is is the efficacy ? It is the ability of drug to initiate biochemical changes leads to the effect of drug 8 9 Antagonist * it binds with receptor without initiating biochemical changes * it has zero efficacy * it binds with any state of receptor (active & inactive) 10 Types Drug Antagonist A- Chemical antagonist B- Pharmacokinetic antagonist * one drug affecting other drug via: - Absorption - Metabolism - Excretion C- Competitive antagonism * Reversible & * Irreversible 11 Continue Types Drug Antagonist D- Non-Competitive antagonism - interrupts receptor-effector linkage - e.g. calcium channel blocker prevents the effects epinephrine on the heart and blood vessels E- Physiological antagonism - Two drugs producing opposite effects - Omeprazole blocks histamine in gastric acid secretion 12 Desensitization and Tachyphylaxis * They are synonymous which describe RAPID loss in the effect of drug despite an increase in the dose of drug * Due to depletion of endogenous neurotransmitters TOLERANCE * It is a decrease in effects of drug as a result of repeated use of drug * It take few days or weeks to develop 13 14 Mechanism of Tolerance, Tachyphylaxis & desensitisation etc.. 1- Change in Receptors - (agonist failure to induce biochemical changes) 2- Loss of Receptors 3- Exhaustion of mediators (depletion) 4- increased metabolic degradation 5- Physiological adaptation (kidney & antihypertensive) 6- Active extrusion of drug from cells 15 DOSE RESPONSE RELATIONSHIP It is a relationship between the drug amount (concentration) and pharmacological effects • Types of responses a- Graded response - response increases by increase the dose b- All or none response such as anti-convulsant. 16 17 Therapeutic index * it is a measure of drug safety * How to calculate ? - LD50/ED50 Potency of drug * It is the minimum dose required to cause maximum response * Potency of drug is not important clinically 18 HOW DRUGS MEDIATE THEIR ACTIONS ? * Via interacting with its target(s) leading to: 1- activation or blocking of receptors 2- block endogenous mediators (counterfeit) 3-open or close ionic channels (Benzodiazepine &L.A. ) 4- compete with uptake system (carrier) - imipramine, cocaine, proton pump inhibitor, digoxin, probenecid 19 Continue HOW DRUGS MEDIATE THEIR ACTIONS ? 5- Enzymes (dihydrofolate reductase targeted by methotrexate & trimethoprim, cyclooxygenase, xanthine oxidase, MAO, Dopa decarboxylase, ACE etc…..) 6- Other targets such as * Immunophilins in lymphocyte targeted by immunosuppresants such as Cyclosporin & Tacrolimus * Tubulin of phagocytes and other cells including cancerous cells - Targeted by Colchicine, Vincristine & Taxol 20 Continue HOW DRUGS MEDIATE THEIR ACTIONS ? 7- Physical means - Osmotic diuretics - inhalational anesthesia 8- Chelating agent * reacts with DNA or ions 21 22 23 24 25 26 Examples on the mechanisms of drugs action 1- activation of muscarinic receptor in the heart(M2) * ACTIVATE Gi-protein which lead to decrease in Camp * This leads to decrease in calcium influx * This causeS bradycardia 2- Activation of muscarinic receptor in smooth muscle (M3) * This leads to activate Gs-protein leads which leads to increase calcium influx which causes contraction 27 Examples on the mechanisms of drugs action 3- activation of alpha-1 receptor in the blood vessels * ACTIVATE Gi-protein which lead to increase in IP3(Inositol triphosphate VIA activation of G-protein * This leads to an vasoconstriction increase in calcium influx and 4- Activation of beta-1 receptor in heart * This leads to activate Gs-protein leads which leads to activate adenylate cyclase which causes phosphorylation of calcium channel * calcium influx which causes contraction(Tachycardia & increase in the force of cardiac muscle contraction (+ve inotropic 28 29 Examples on the mechanisms of drugs action 5- Activation of beta-2 receptor in smooth muscle * This causes to activate Gs-protein and to activate adenylate cyclase •CAMPactives protein kinase which leads to series of phosphorylation of various protein •phosphorylation either activates or inhibits target enzyme or channel * in smoth muscle , CAMP dependent protein kinase phosphoryate myosin-light chain kinase which required for contraction (relaxation occurred) 30 31 Classification of adverse effects 1- TYPE A - It is dose related - It depends on therapeutic index 2- Type B - Non-dose related - immunological reactions - Pharmacogenetic 3- Long-Term effects - Adaptive changes 32 Classification of adverse effects - Rebound Phenomena - It depends on therapeutic index 4- Delayed effects - Non-dose related - Carcingenesis - impair fertility - Teratogenicity - drug in breast milk 33 Pharmacokinetic of drugs 1- ABSORPTION OF DRUG - From the site of administration 2- Distribution - To reach the site of action 3- metabolism - to inactivate or activate 4- Excretion 34 ROUTE OF DRUG ADMINISTRATION 1- Oral administration (P.O.) 2- Subcutaneous (S.C.) 3- Intradermal 4- Intramuscular (I.M.) 5- Intravenous (I.V.) 6- Sublingual 7- Rectal 35 ROUTE OF DRUG ADMINISTRATION 8- Intrathecal & epidural 9- Inhalation 10- Topical * skin * eye * mucous membrane -nasal, vaginal, oropharynx 36 37 Pharmacokinetics Disposition of Drugs Time Course of Drug Action 38 Major Topics • • • • • • Passage of drugs across membranes Absorption of drugs Distribution of drugs Metabolism of drugs Excretion of drugs Pharmacokinetic models 39 Passage of drugs across membranes • Structure of the plasma membrane 40 Mechanisms of transport • Passive diffusion: passage of drugs through the lipid surface (major mechanism of drug absorption) – Lipid-soluble drugs – Small water-soluble drugs – Noncharged form of weak electrolytes 41 Membrane permeability versus lipid (olive oil):water partition coefficient 42 Weak electrolytes and membrane permeability 43 Mechanisms of transport (2) • Filtration: bulk flow of water-soluble drugs through pores (glomerular, capillary) – Glomerulus: 80Å pores – Capillary endothelium: gap junctions – Blood brain barrier: 8Å passageways 44 Mechanisms of transport (3) • Facilitated diffusion: carrier-mediated, ATP not required (e.g., glucose) • Active transport: carrier-mediated, ATP required (e.g., Na+, K+, Ca++) 45 Mechanisms of transport (4) • Endocytosis and exocytosis: (e.g., for very large compounds) Receptor Dynamin Clathrin 46 Absorption of drugs • From gastrointestinal tract: lipid-soluble, nonionized forms of drugs are absorbed better than water-soluble, ionized forms of drugs – environmental pH important in absorption – acidic drugs (aspirin) absorbed better theoretically in stomach (pH 1-2), basic drugs (codeine) absorbed better in intestine (pH 7-8) 47 Henderson-Hasselbach equation base pH - pKa = log acid For an acidic drug: acid = HA; base = AFor a basic drug: acid = BH+; base = B 48 Theoretical absorption of aspirin and codeine for dental pain 49 Unique characteristics of the oral route • Influences of gastric emptying, mucosal surface area, and drug inactivation important for oral route • Small intestine usually most important because of large surface area (folds of Kerckring, villi, microvilli) 50 • Clinical advantages – Safest route – Cheapest route – Best patient acceptance • Disadvantages – Delayed effect – Patient cooperation required – Unique problems with GI toxicity 51 Absorption of drugs (2) • From oral, sublingual, or rectal mucosa: passive diffusion. – May bypass first-pass inactivation • From the lungs: passive diffusion – rapid absorption, dependent on particle size (6 µm cutoff) 52 Absorption of drugs (3) • From injection sites: subcutaneous tissues, muscle or fat, absorbed by diffusion and affected by blood flow • From miscellaneous sites: skin, spinal canal, tooth pulp • Intravenous, intraarterial injection avoids absorption 53 Bioavailability • Clinical pharmacology of differential absorption • Related terms – biologic equivalence – chemical equivalence – therapeutic equivalence 54 Distribution • Absorbed drugs leave capillary wall quickly and freely (via filtration and diffusion) to enter interstitial fluid; blood flow being important in the regional distribution of drugs 55 • Binding to plasma proteins (mostly to albumin and, for basic drugs, a1-acid glycoprotein) – major distribution site – highest drug concentrations usually found in blood; serve as drug depots, thus prolonging half-life of drugs – pharmacologic effects and toxic manifestations affected by hypoalbuminemia and copresence of other drugs also bound effectively to albumin 56 • Central nervous system: permeable to lipidsoluble drugs only; limited permeability to water-soluble drugs when inflamed • Placental transfer: limited by blood flow, not by a "barrier" 57 • Fat tissue: depot for thiopental and chlorinated hydrocarbon insecticides (e.g., DDT) • Sites for metabolism and excretion: liver, kidney, intestine, lungs • Redistribution: especially important for IV injection of lipophilic drugs 58 Redistribution of thiopental after intravenous injection 59 Metabolism • General considerations - drug metabolism (biotransformation) usually results in more watersoluble, more polar metabolites, thus facilitating their excretion by reducing renal tubular reabsorption • drug metabolism does not always result in detoxification and inactivation of drugs, although these usually occur 60 Chemical reactions • Phase I – – – – – microsomal oxidation (important) nonmicrosomal oxidation (e.g., alcohol) reduction hydrolysis dehalogenation 61 Microsomal enzyme oxidation system 62 • Role of cytochrome P450 system – CYP3A4 – CYP2D6 – CYP2C 54 22 17 25 CYP1A2 CYP2E1 CYP3A CYP2D6 CYP2C 63 Chemical reactions (2) • Phase II (conjugation) – – – – – – glucuronidation (microsomal, important) acetylation amino acid synthesis methylation sulfate addition others (e.g., glutathione addition) 64 Factors affecting drug metabolism • reversible binding to plasma proteins • localization of drugs (e.g., fat) • hepatic blood flow 65 Factors affecting drug metabolism (2) • pathology-, age-, or genetics-related deficiency or alteration in drug metabolizing enzyme (e.g., pseudocholinesterase deficiency and succinylcholine) • inhibition of drug metabolizing enzyme (e.g., by erythromycin) • induction of drug metabolizing enzyme (e.g., by phenobarbital) 66 Excretion • Renal excretion – involves glomerular filtration and tubular reabsorption and secretion 67 – excretion increased by decreasing tubular reabsorption, thus basic drugs are excreted better in acidic urine, acidic drugs better in alkaline urine – clinical application—aspirin and barbiturate poisonings are treated by alkalization of patients’ urine by giving sodium bicarbonate 68 • phase II reactions (conjugation) increases tubular secretion and prevents reabsorption (exception: methylation) 69 • Others – – – – – – Bile Lung Feces Saliva (pp. 24-25, Table 2-1) Sweat Milk 70 Time Course of Drug Action • General rules • Compartment models – Single-compartment – Multiple-compartment • Exceptions to general rules 71 General rules • Plasma concentration related to degree of receptor binding, thus magnitude of drug effect • Disposition processes usually first order • Elimination usually slower process than absorption or distribution 72 • First-order process: – dC/dT = k•C (constant fraction) • Zero-order process: – dC/dT = k (constant amount) • Capacity limited process: – low C, first-order; high C, zero-order 73 Single-compartment model ka Absorption Vd Body ke Elimination C = D/Vd or Vd = D/C 74 Single compartment model: no absorption, first-order elimination 75 • Clearance (CL): the measurement of blood cleared of the drug by elimination per unit time (as in units of mL/sec). It and the volume of distribution (Vd) create the dependent variable T1/2. They are related by the following formula: T1/2 = 0.693Vd/CL 76 With renal excretion C•Cl = U•V Where C = plasma concentration, Cl = clearance, U = urinary concentration, and V = urinary volume Cl = U•V/C 77 • Drug disappearance – usually follows first-order kinetics (exponential decay), with a constant fraction (not amount) of drug being eliminated per unit of time – the process is independent of the kind and amount of drug – half-life (T1/2), not dose, is the primary factor in prolonging drug effects 78 Overriding importance of halflife on duration of drug effect 79 Drug accumulation with repeated dosing 80 Multicompartment models • combine kinetics of redistribution and elimination • provide best description of drugs with high lipid solubility and drugs given intravenously 81 Two-compartment model 82 83 84 ORAL ADMINISTRATION 1- PROS • Convenient • Safe ? • Economical (does not need sterilization) 2- CONS • Requires patient compliance • Drugs irritant to stomach • Drugs not stable in GIT • Drugs extensively metabolize by the liver • Drugs NOT absorb from GIT • Leads to food drug interaction 85 INTRAVENOUS ADMINISTRATION 1- PROS • Rapid action • Delivered the desired amount • irritant drug can be given only I.V. but NOT S.C. 2- CONS • Increase the risk of adverse effects • Must inject slowly in order to minimize the effects of drug on the heart • It needs constant monitoring the reponse of patient 86 SUBCUTANEOUS ADMINISTRATION 1- PROS • It provides sustain effects because of slow absorption • Addition of vasoconstrictor decreases further the rate of absorption from the site of injection • It is suitable for insoluble drugs such as pellets and suspension 2- CONS • can not inject large volume • can not inject irritant drug • repeated injection leads to necrosis (atrophy of skin) 87 INTRAMUSCULAR ADMINISTRATION 1- PROS • Suitable for oily vehicle and irritant drug • The rate of absorption is very high because of high blood flow in the muscle 2- CONS • It is not recommended in patient taking Anticoagulant • Increase CPK 88 PULMONARY ADMINISTRATION 1- PROS • Rapid absorption • Local administration into the lung is beneficial in bronchial asthma •Avoid hepatic effects •Can absorb fine droplets (aerosol), prticle size, gaseous and volatile drugs 2- CONS • Difficult to regulate & administered the dose • some drugs cause lung irritation 89 TOPICAL ADMINISTRATION 1- Mucous membrane • Rapid absorption such as local anesthetic & ADH 2- Skin • Lipophilic drugs absorb rapidly from skin such as nitroglycerin skin batch, scopolamine batch • Inflammed, burned, abraded skin absorb drug faster 90 TOPICAL ADMINISTRATION 3- Ophthalmic absorption • it is used for local effectss • systemic absorption occurs through NASOLACRIMAL CANAL such as β-adrenergic blockers eye drops •Ointment and suspension minimized systemic absorption •Ocular insert provides continous delivery of drug with minimum systemic absorption 91 SUBLINGUAL ADMINISTRATION • Excellent absorption for non-ionized drug Example Nitroglycerin, apomorphine (Uprima) • It has high absorption rate close to intravenous injection • Avoid hepatic first pass metabolism 92 RECTAL ABSORPTION • It is used when oral route is warranted such as vomiting or coma • It has erratic, irregular and incomplete absorption (50%) • It goes in partial hepatic first pass metabolism •Some drugs may cause rectal irritation 93 DRUGS DISTRIBUTION Factors influence drug distribution 1- Permeability of drug to biological membranes •Blood brain barrier •Testicular barrier •Placental barrier - LIPID SOLUBLE DRUGS -They have large Vd (volume of distribution) 2- Extent of plasma protein - Highly protein bound stay in circulation & also have large Vd 94 DRUGS DISTRIBUTION Factors influence drug distribution -Drugs with large Vd have the following properties •High protein binding •High lipid solubility •High affinity to other tissues such as bone & liver 95 DRUGS DISTRIBUTION Factors influence drug distribution 3- Availability of transport mechanism - passive diffusion: The drug must be in unionized form - Active transport: require ATP - Facilitative diffusion: it requires carrier but without energy such vit B12, glucose and amino acid - ion pair transport: the ionic compound combines reversibly with endogenous compound such as MUCIN in GIT 4- Regional pH - breast milk more acidic than blood: Weak base drugs accumulate in breast milk 96 DRUGS DISTRIBUTION Factors influence drug distribution 4- Rate of blood flow to tissues - Skeletal muscles have high blood flow 5- Regional pH - breast milk more acidic than blood: Weak base drugs accumulate in breast milk 6- Tissues mass 97 DRUG METABOLISM OBJECTIVES OF METABOLISM 1- To make the drug more water soluble in order to facilitate its excretion 2- To activate or inactivate the drug * Some drugs become highly toxic or carcinogenic 98 Factors influence Metabolism 1- Drugs - inducer: rifampicin, dilantin, barbiturate - inhibitors: cimetidine, macrolide & antifungal drugs 2- Liver diseases 3- Diet - grape fruit, vitamins deficeincy such vit B6 is cofactor for decarboxylation 99 Types of reactions in metabolism * Phase-I reaction - consist of oxidation (dealkylation & deamination) , reduction or hydrolysis - the product is reactive such as hydroxyl -Some time highly toxic - the product ready to enter other phase of metabolism * Phase-II - Normally results to inactive compound - involve conjugation of glucuronyl, sulfate Play a role in enterohepatic cycle 100 EXCRETION OF DRUGS 1- TYPES OF EXCRETION • Renal excretion • Biliary excretion • Pulmonary excretion • Excretion via other body fluids - Saliva -Breast milk 101 RENAL EXCRETION OF DRUGS Some drugs mainly excreted via kidney such as metformin & sotalol etc… •Factors influence renal excretion •GFR • Interference with renal active transport of drug such as probenecid • Altering passive diffusion by change PH, lipid solubility 102 RENAL EXCRETION OF DRUGS •Altering passive diffusion by change PH - When pH of urine acidic, weak base drug will not be reabsorb from renal tubule -When pH of urine alkaline, weak acid drugs will not reabsorb from renal tubule •Lipid water solubility - Highly lipid soluble drug stay in circulation for longer time 103 BILIARY EXCRETION & ENTEROHEPATIC CYCLE OF DRUGS Liver cells transfer various drug from plasma to bile by • Transport system similar to renal tubule • conjugates drugs and concentrate these drugs in bile and the delivered into the intestine • Some conjugate drugs which is delivered into the intestine hydrolyzed to unconjugated drug (free drug) • The free drug reabsorb back into circulation • This called enterhepatic cycle. 104 BILIARY EXCRETION & ENTEROHEPATIC CYCLE OF DRUGS • This creates a reservoir of recirculating drugs which represent around 20% of total drug in the body • This cycle maintains drug blood levels leading to prolongs the drug action • Examples of drugs go through enterohepatic cycle: - Digoxin - morphine - steroids including sex hormones 105 PULMONARY EXCRETION OF DRUGS Pulmonary excretion does not require metabolism • Factors influence pulmonary excretion 1- Rate of respiration 2- Cardiac output 3- solubility of gas in blood - High blood solubility decreases gases loss from lung - In contrast less blood soluble, leads to faster loss of gas via lung such nitrous oxide 106 Excretion of drugs via other body fluids 1- Sweat - Drugs or its metabolite may be responsible for induction of dermatitis or other skin reactions 2- Saliva - change in taste or induction metallic taste 3- Milk - The PH of milk is 6.5, therefore the weak base drugs will concentrate in milk 107 Thank you 108